Transversus Abdominis Plane Block versus Caudal Epidural Block for Lower Abdominal Pediatric Surgeries. A Randomized Prospective Comparative Study
Amir Abouzkry Elsayed1*, Ahmed Ahmed Saad Awad2, Ahmed Elsaied Abdul Rahman3, Aymen Mohamady Eldemerdash2
1Department of Anesthesia and Surgical Intensive Care, Faculty of Medicine, Kafrelsheikh University, Kafrelsheikh, Egypt
2Department of Anesthesia and Surgical Intensive Care, Faculty of Medicine, Aswan University, Aswan, Egypt
3Department of Anesthesia and Surgical Intensive Care, Faculty of Medicine, Sohag University, Sohag, Egypt
Submission: September 08 2022; Published: October 04, 2022
*Corresponding author: Amir Abouzkry Elsayed, Department of Anesthesia and Surgical Intensive Care, Faculty of Medicine, Kafrelsheikh University, Kafrelsheikh, Egypt, Tel: 00201016326544
How to cite this article: Amir A E, Ahmed A S A, Ahmed E A R, Aymen M E. Transversus Abdominis Plane Block versus Caudal Epidural Block for Lower Abdominal Pediatric Surgeries. A Randomized Prospective Comparative Study. J Anest & Inten care med. 2022; 12(2): 555834. DOI 10.19080/JAICM.2022.12.555834
Abstract
Background and Objectives: To check the advantages of ultrasound guided transversus abdominis plane block (TAPB) and the gold standard caudal block as regards pain control and associated complications in children assigned for unilateral abdominal surgeries.
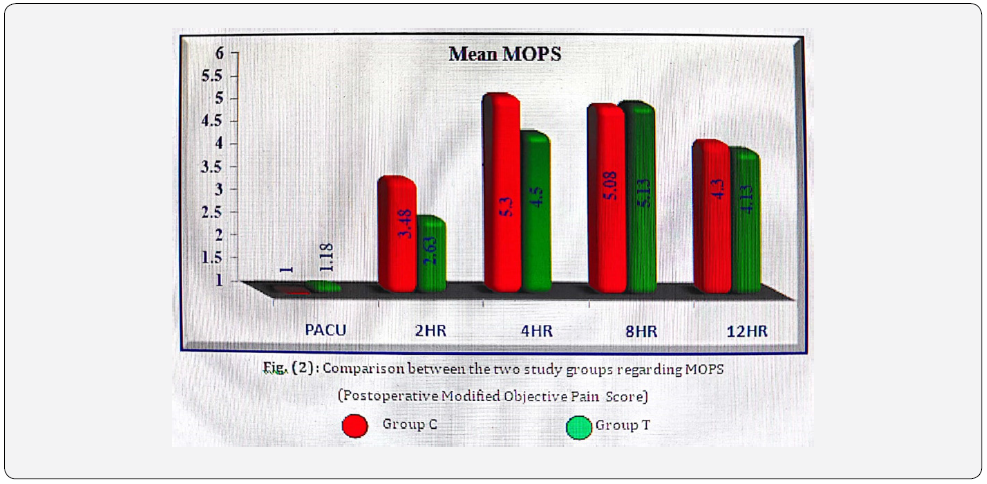
Methodology: Eighty children, aged 1-4 years old were categorized into group C; received caudal block, and group T; received TAPB immediately after induction of general anesthesia using bupivacaine. Postoperative (PO) pain was monitored for 12-hrs using 10-points Modified Objective Pain Score (MOPS) as a primary outcome. A paracetamol suppository (20 mg/Kg) was given if the MOPS score was ≥ 6 in two consecutive measurements. Intraoperative (IO) and PO hemodynamic responses as well as incidence of complications were also recorded. Results were analyzed using unpaired t-test, Mann-Whitney and Chi-square test.
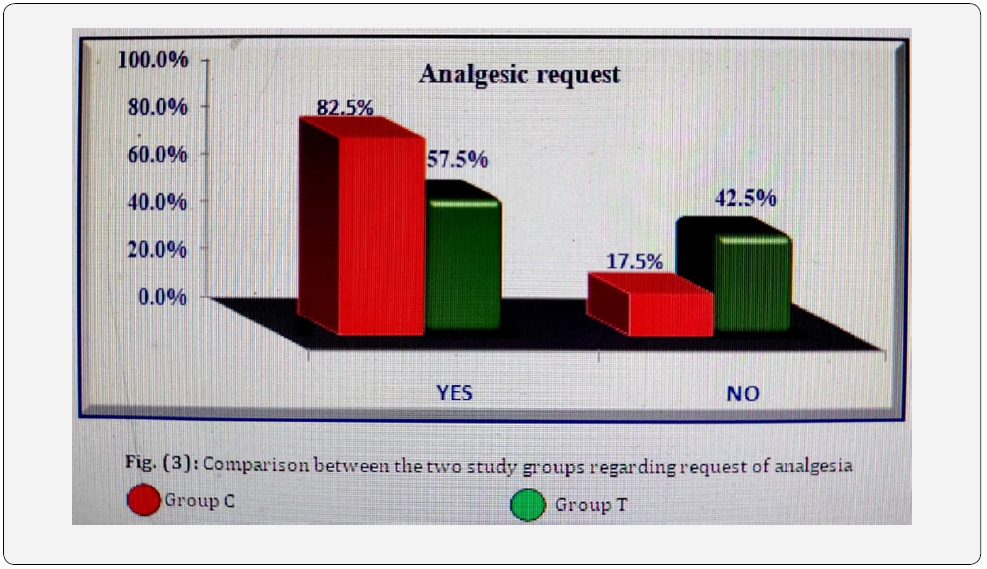
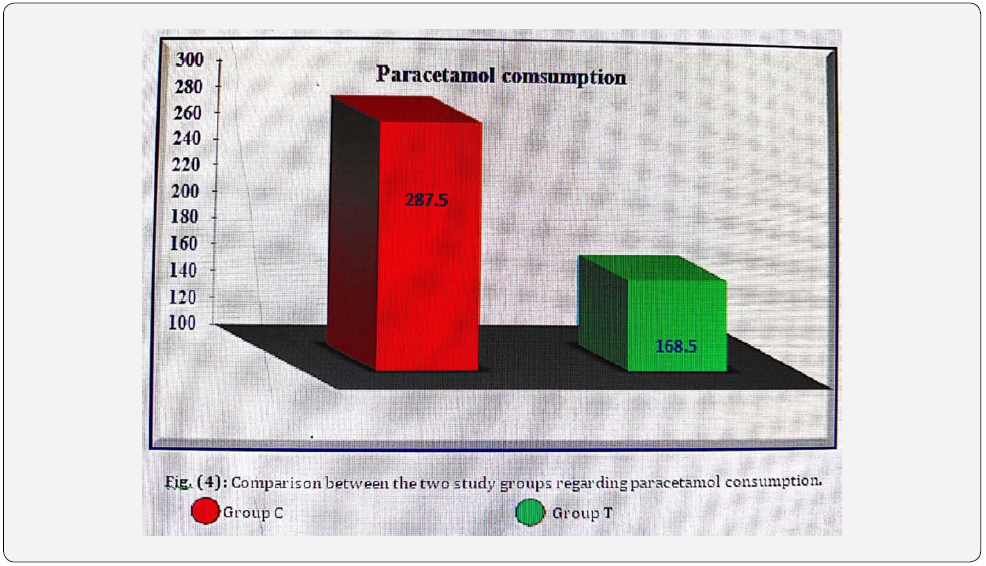
Results: Postoperative Modified Objective Pain Score (MOPS) was statistically significant higher in group (C) in comparison to group (T) 2hrs & 4hrs postoperatively (P= 0.044, 0.020, respectively). Duration of postoperative analgesia was significantly longer in group T than in group C (P= 0.001). As regard request for rescue analgesia, 33 patient (82.5%) of group C requested rescue analgesia that was significantly greater than group T where 23 patients (57.5%) requested rescue analgesia (P=0.027). Regarding total paracetamol consumption, it was statistically significant greater in group C than group T (P=0.004).
Conclusion: Transversus abdominis plane block with ultrasound-guidance was effective and hemodynamically safe with no documented intra- or postoperative adverse events and had longer duration as regard postoperative analgesia. The close ultrasound monitoring of local anesthetic diffusion in allowed space increased success rate and maintained the quality of the block.
Keywords: Transversus abdominis block, Caudal epidural block, Ultrasound guidance, Abdominal surgery
Abbreviations: TAPB: Transversus Abdominis Plane block; MOPS: Modified Objective Pain Score; PO: Postoperative; IO: Intraoperative
Introduction
Lower abdominal surgeries in children include inguinal hernia repair, hydrocelectomy, etc. The most common lower abdominal surgery in children is inguinal hernia repair [1].
Following surgery, patients reported somatosensory pain at the site of the incision as well as visceral discomfort and irritation [2].
The use of regional anesthetic methods on pediatric patients has grown significantly in popularity. The main benefits of regional supplementation are reduced intraoperative anesthetic requirements and effective postoperative pain management [3].
The time needed to establish acceptable pain control is frequently used to define the typical duration of hospital stay, which usually lasts between 12 and 24 hours [4].
Children’s regional blockage under ultrasound guidance is probably less likely to fail. It prolongs the block and most likely lowers pain scores following surgery. The probability of some minor complications varying little or not at all [5].
As it inhibits both visceral and somatic pain with a low complication rate and better patient pain scores than patients receiving general anaesthesia alone, caudal epidural anaesthesia is regarded as the gold standard regional technique for pain management following paediatric pelvic and lower abdominal operations [6].
Neuraxial block should not be used in cases of compromised hemostasis, bacteremia, and neuraxial abnormalities, and may have more serious potential complications than peripheral nerve blocks [7].
The effectiveness of ultrasound in reducing the risk of complications has not yet been established. Caudal blocks are increasingly performed with ultrasound as an auxiliary technique to direct cannula insertion and to demonstrate proper distribution of local anesthetic in the caudal epidural space [8].
The transversus abdominis plane block (TAPB) was created as a result of improved knowledge of the anatomy of the abdominal wall to treat pain following lower abdominal surgery [9].
TAPB significantly reduced postoperative pain scores and opioid requirements by providing reliable unilateral sensory block in the T10-L1 distribution with a single injection, after major abdominal surgeries with rare complications, especially when carried out under direct ultrasound guidance [10].
Some pediatric studies used TAPB for postoperative analgesia recorded 10 to 15 hours duration of analgesia [11].
In this study, we used ultrasonography to perform either TAPB or caudal block to check the advantages of TAPB over traditional caudal block as regards pain control and associated complications in 1 to 4 years old patients assigned for unilateral abdominal surgeries.
Methodology
This prospective, comparative study was carried out at Aswan University hospital, Anesthesia, ICU and pain management department, between June 2017 and June 2019. The institutional ethics review board (EC Ref No.: aswu/168/9/17) gave its approval to the study protocol. The protocol of the study was described to the parents and the informed agreement was taken.
All children aged 1-4 years and assigned for short-duration surgery (as hernia repair, orchiopexy, hydrocelectomy) under general anesthesia were eligible for study. Patients with any sort of active infection at local anesthetic injection site, mental retardation, anatomical variations that made it unsafe to place either caudal epidural block or TAPB, presence of a preexisting chronic pain disorder, coagulation disorders, presence of uncontrolled respiratory or cardiac diseases, or sensitivity to study drugs were excluded from the study.
All eligible children were clinically evaluated to assure absence of exclusion criteria. An anesthesiologist who was not involved in the study concealed the computer-generated random numbers that were used to randomize the patients inside the sealed, opaque envelopes. Both parents and outcome assessor were blind to the grouping of the patients.
All patients had to be fasted for at least 6 hours for solids and 2 hours for water. Routine preoperative assessment to fulfill patient’s inclusion criteria for the study by history, Physical examination, and laboratory study (CBC, coagulation profile…). Laryngeal mask intubation with intraoperative monitoring included non-invasive measurements of mean arterial blood pressure (MAP), ECG, heart rate (HR), capnography, and oxygen saturation using oximetery (SpO2) and after laryngeal mask intubation.
Anesthesia was initiated using inhalational induction (oxygen and sevoflurane 8%) through pediatric anesthesia breathing circuit (Mapleson F) using assisted spontaneous respiration. After establishing venous access fentanyl 1 μg/kg IV was administered, appropriate size of laryngeal mask was placed, and sevoflurane 2%and oxygen were used to maintain anesthesia. Before making the surgical incision, blocks were done. Sevoflurane was withdrawn when the procedure was completed. Extubation was carried out when regular respiration and cough reflex were restored. Then patients were shifted to post anesthesia care units (PACU) with monitoring of oxygen saturation and vital signs.
To avoid incomplete or unsuccessful blocks, all blocks (including caudal) were carried out utilizing ultrasound guidance, standard techniques, and predefined end points for needle placement and local anesthetic dissemination. A 7 MHz linear portable ultrasound probe was used for continuous in-plane ultrasound guidance. The patient was withdrawn from the trial if proper local anesthetic distribution could not be verified.
The patients were split into two groups; each included40 patients either to undergo TAPB or caudal block.
Group C (40 patients): Received caudal block.
After initiation of anesthesia a left lateral decubitus was attained with flexion of hips and knees, then the region was swabbed with alcohol solution, after the correct position and disinfection, the ultrasound probe was covered in a sterile cover. Initially scanning to visualize midline and to identify sacrococcygeal ligament in between the 2 sacral cornua. Next, a 90-degree rotation of the probe is performed to obtain a longitudinal view. A 22-gauge needle is inserted at a 20-degree angle, keeping needle tip visible, with a noticeable pop as the sacrococcygeal ligament was punctured by the needle. Once the caudal area was identified on the screen by the needle position, careful aspiration was done to verify that there was no CSF or blood present. Then 1 ml/Kg of bupivacaine 0.25% was slowly injected.
Group T (40 patients): Received TAPB block.
These children received unilateral transversus abdominisplane (TAP) block with 0.5 ml/Kg of 0.25% bupivacaine with ultrasound visualization as follows: Following induction of general anesthesia, using portable ultrasound with7MHz linear probe was used to identify targeted plane. To obtain the best ultrasonographic images of the abdominal wall muscles and the nearby anatomical structures, modifications were made to depth, low and far gain, and probe frequency. Following sterilization of the needle insertion point and the ultrasonographic probe with the child in supine position, a linear ultrasound probe was positioned in the axial plane approximately cephalic to iliac crest or where the three muscle layers were most easily distinguished on ultrasound. The anterior abdominal wall muscles were identified at this level as the external oblique lays most superficially, the internal oblique is just deep to the external oblique and transversus abdominal muscle is the deepest of the three and is just superficial to the peritoneum. An in-plane approach from anterior to posterior that was nearly perpendicular to the ultrasound beam was used for needle placement with 22 g blunt-tip needle. After being able to see the needle tip in the TAP, 0.5 ml/kg of 0.25% bupivacaine was injected while keeping an eye on the proper spread inside the plane.
Twenty minutes after the block, skin incisions were made in both groups. General anesthesia was stopped and the laryngeal mask was removed once the procedure was finished and the skin was closd.
Any incidence of complications such as bloody or wet tap (in group C) or adjacent structure injury (in group T) was considered as failure of technique.
Measurements
The primary endpoint of our study was the Postoperative Modified Objective Pain Score (MOPS) which was recorded on admission to PACU, 2hr, 4hr, 8hr, and 12hr post-operatively. Parameters: included crying, movement, agitation, posture, and verbal response (Table 1) [12].
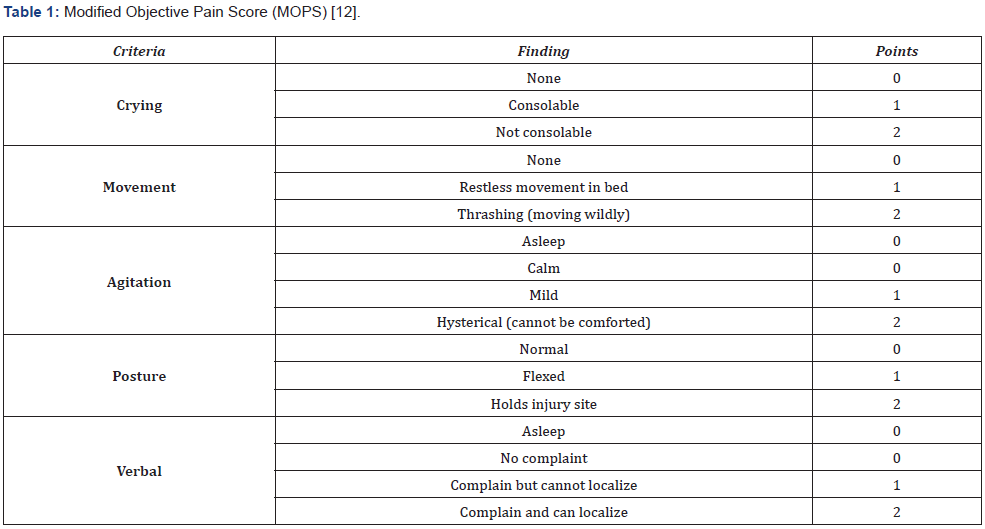
Interpretations of MOPS were: minimum score: 0, maximum score: 10.
As the pain score increased, the child’s level of suffering increased. A paracetamol suppository (20 mg/Kg) was given to the child if the MOPS score was ≥ 6 in two consecutive measurements (rescue analgesia).
Secondary outcome of the study included:
-Intraoperative hemodynamic responses (mean arterial blood pressure heart rate, and respiratory rate) in both groups: As base line values (before the block), 10 min after establishment of the block, at skin incision, at 25 min and 40 min after block and at end of operation were recorded.
-Postoperative analgesia duration (Time to first rescue analgesia).
-Postoperative hemodynamic responses (heart rate and MAP): The kids were observed every 30 minutes for the first hour and every hour for the following 6 hours, then every two hours for the next 6 hours. Then hemodynamic responses were recorded on admission to PACU, 2hr, 4hr, 8hr, and 12hr postoperatively.
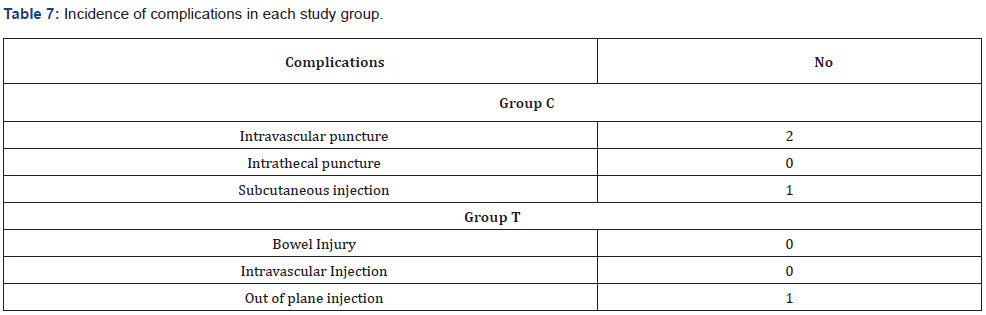
- The incidence of complications:
· For group C: Intravascular, intrathecal puncture and misplacement of the needle (subcutaneous injection).
· For group T: Colonic injury, intravascular injection.
Sample size calculation
Using the Clin Calc calculator setting alpha errors at 5%, Beta errors at 20%, confidence interval at 95%, power at 80% & result from previous study [13] who organized a comparison between ultrasonography-guided transversus abdominis plane block and caudal epidural block for relieving pain in children undergoing lower abdominal surgery; a more caudal group patients (75%) complained of pain in 6- to 24- hour postoperative period than TAP group patients (44.1%). Therefore, a total of 76 children (38 per group) will be needed. The sample size was 40 patients per group since 2 additional patients were recruited to each group to compensate for dropouts.
Statistical analysis
IBM SPSS Statistics 24.0 was used to collect, code, tabulate, and then analyse the data. Categorical data were expressed as number of cases (%) while numerical data were expressed as mean (SD). Between-groups comparisons of numerical variables were made using unpaired student (t-test) or the Mann-Whitney test when required, while those of categorical variables were done using Chi-square test or by Fisher exact test whenever appropriate. Any difference with p < 0.05 was regarded of statistical significance.
Results
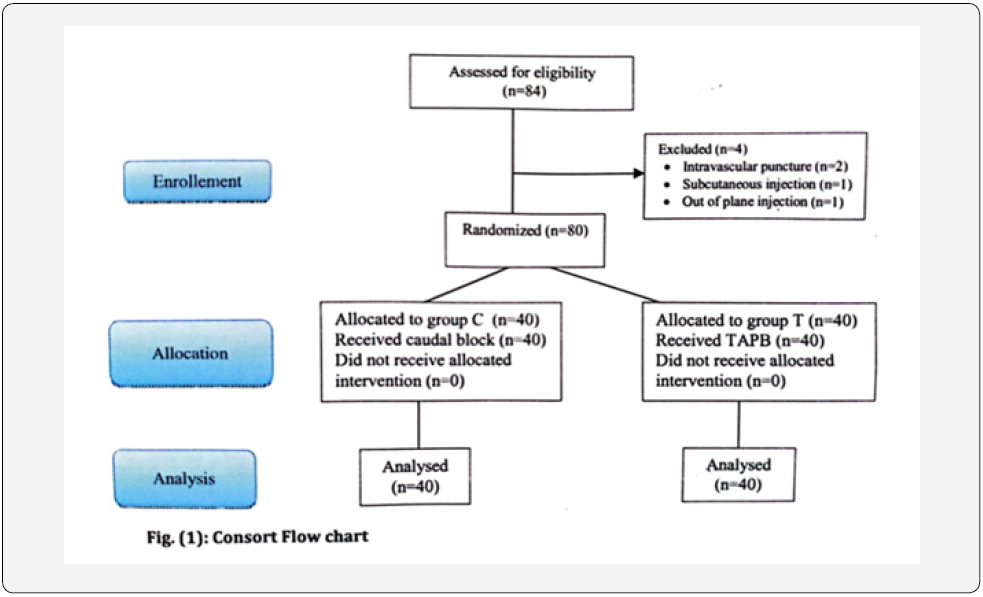
Therewere 84 patients in the current study but only 80 patients who were eligible to participate in our study (Figure 1).
Concerning age, gender, weight, ASA class, type, or duration of operation, no statistically significant difference (p˃0.05) was detected between the two study groups (Table 2).
Postoperative Modified Objective Pain Score (MOPS) was statistically significant higher in group (C) in comparison to group (T) 2hrs & 4hrs postoperatively (P= 0.044, 0.020, respectively) (Table 3, Figure 2).
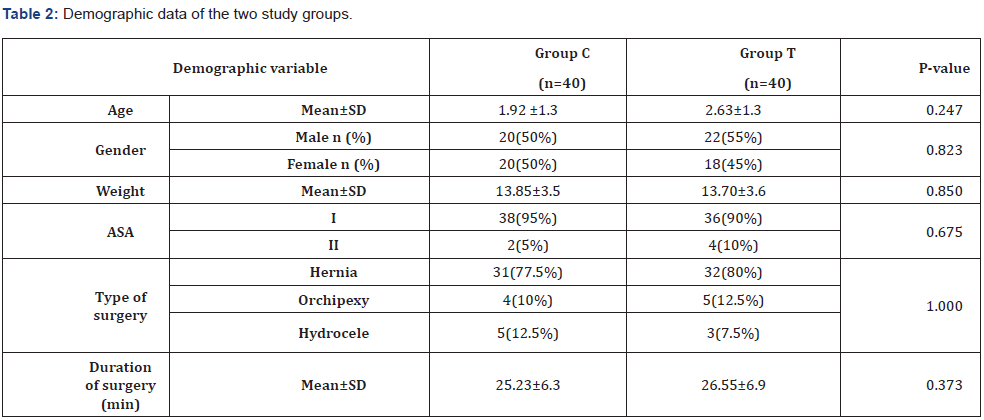
Data were presented as mean ±SD, numbers & percentages; P-value indicated the significance of variance between studied groups.
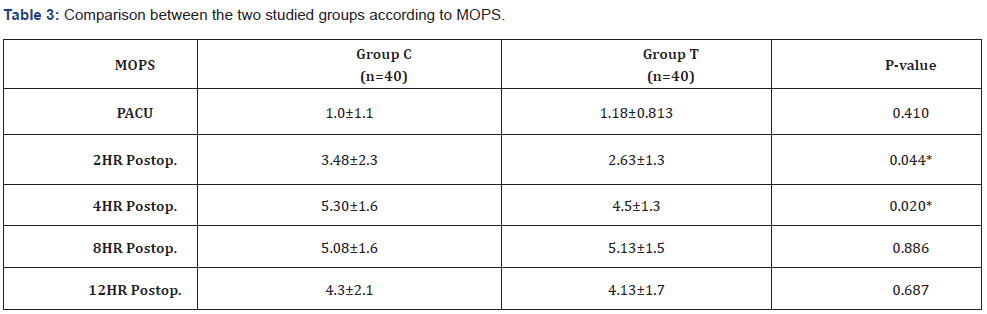
Data were presented as mean ±SD; P-value indicated the significance of variance between studied groups; *: significance of difference between studied groups.
Duration of postoperative analgesia (The time from completion of blocks to the first administration of rescue analgesia) was significantly longer in group T than in group C (P= 0.001).
As regard request for rescue analgesia, 33 patient (82.5%) of group C requested rescue analgesia that was significantly greater than group T where 23 patients (57.5%) requested rescue analgesia (P=0.027) (Table 4, Figure 3).
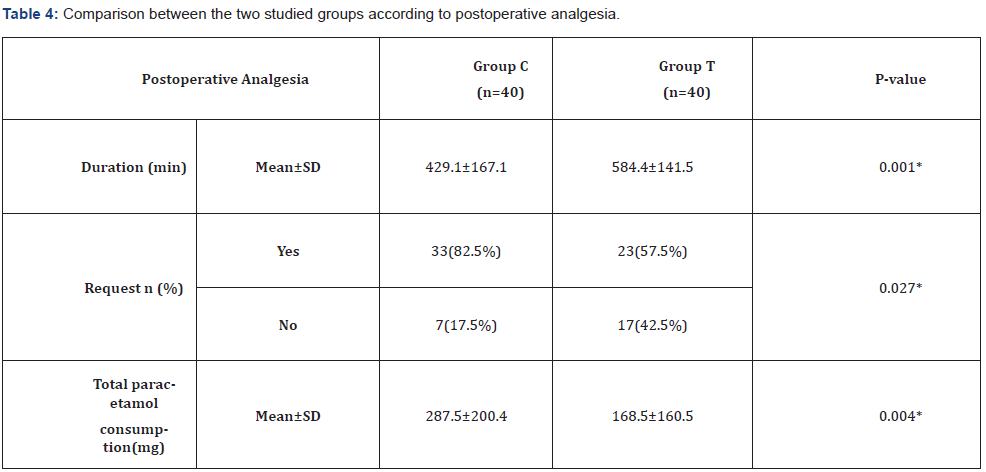
Data were presented as mean ±SD, numbers & percentages; P-value indicated the significance of variance between studied groups.
Regarding total paracetamol consumption, it was statistically significant greater in group C than group T (P=0.004) (Table 4, Figure 4).
- Hemodynamic data:
[A] MAP:
MAP was significant higher in group T when compared with group C after 10min of the block, at skin incision, after 25min,40min, at end of the procedure& at PACU (P=0.016, 0.014, 0.047, 0.015, 0.022,0.044, respectively) (Table 5).
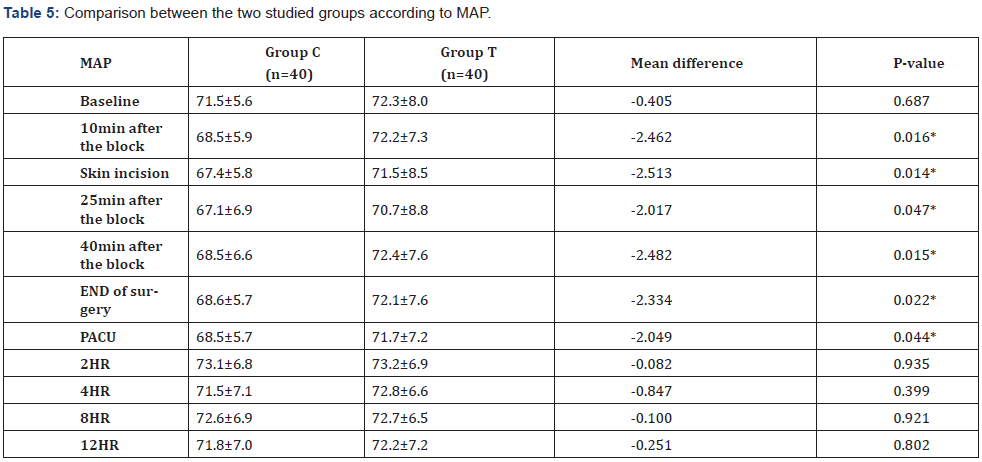
Data were represented as mean ±SD, numbers & percentages; P-value indicated the significance of variance between studied groups.
B) HR:
Between the two study groups, there was no significant statistical difference in HR (Table 6).
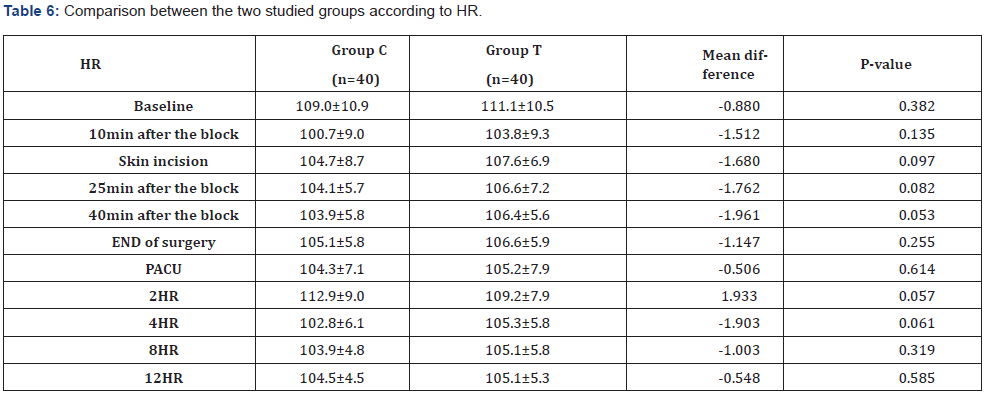
Data were presented as mean ±SD, numbers & percentages; P-value indicated the significance of variance between studied groups.
The occurrence of complications in group C, was recorded as two cases of intravascular puncture, and one case of subcutaneous injection, while the incidence of complications in group T, was recorded as one case of out of plane injection (Table 7). All these cases with recorded complications were excluded from our study.
Discussion
An increased use of regional anesthesia techniques in infants and children was integrated in an effort to enhance postoperative analgesia while minimizing opioid-related side effects [14].
The ultrasound in pediatric regional anesthesia could be of greater value. It could confirm that the local anesthetic was delivered around the nerve with precise needle insertion. This should permit high-quality regional anesthesia and reduce the risk of intra-neuronal or intra-vascular injection [15].
The goal of current study was to assess use of transversus abdominis plane (TAP) block with ultrasound guidance in pediatric patients and compare it with caudal epidural anesthesia as regard the efficacy of the block, onset time and duration of action, and the incidence of complications.
Regarding age, sex, weight, surgery type, duration of the procedure, ASA classification (P > 0.05), and onset of block, there was no statistically significant difference between both groups in the present study.
In the present study, both caudal epidural anesthesia and transversus abdominis plane (TAP) blocks with ultrasound guidance offered good intraoperative analgesia and there was no statistical significant difference between both groups as regard changes in heart rate and respiratory rate 25 min, 30 min, 35 min after block and at end of operation.
This was consistent with the findings by Fredrickson [16]. [16] who had a prospective audit of TAP block in eight patients undergone repair of inguinal hernia; 5 of the 8 kids requested no opioid intraoperatively while the other 3 patients requested fentanyl supplementation (<0.5 μg/kg) during manipulation of the spermatic cord, which involves stimulating the genitofemoral nerve, which is partially supplied by L2. Using the Children’s Hospital Eastern Ontario Pain Scale (CHEOPS) and the Objective Behavioral Pain Score (OPS), the analgesic quality was evaluated.
This also was agreed by another study done by Baeriswyl et al. [17] who concluded that there is “moderate evidence” that epidural analgesia and TAP block are equally efficient in alleviating postoperative pain in both adults and pediatric patients. TAP block was also associated with a fairly short length of stay and fewer incidents of hypotension.
Another study agreed with us, done by Kumar et al. [18] who concluded that postoperative analgesia for children having inguinal herniotomy can be effectively provided by both TAP block and caudal block. When compared to caudal block following inguinal herniotomy, USG-guided-TAP block was shown to be preferable because it extended the duration of analgesia and reduced the rescue analgesic dose without having any apparent adverse effects.
Our results also agreed with the results of Jacobs et al. [19] in a retrospective case series study involved 10 patients. All patients aged 1 day to 6 months underwent laparotomy (n5), colostomy (n2), closure of gastroschisis (n1), reversal of ileostomy (n1), and cholangiogram(n1), using subcostal or posterior approach with ultrasound guidance by 0.25% levobupivacaine, 1 ml/kg except in two patients where surgical incision needed TAP blocks in which 0.25% levobupivacaine, 0.5 ml/kg was administered on each side. They recorded the hemodynamic response to the surgical incision, the need for intraoperative opioids, the need for postoperative analgesia, and the neonatal infant pain scale (NIPS), and discovered that the (TAP) block had an opioid-sparing effect in all except one case involved extensive bowel manipulation.
Our findings were also in line with a study of Al-Sadek and her colleagues [20] who compared bilateral (TAP) block using ultrasound guidance with regular analgesics for 108 kids, 3-7 years old with undescended testis undergone laparoscopic surgery and found significant reduction in intraoperative fentanyl requirement in TAP group.
Also, the randomized control trial of El Fawy and El Gendy [21] who enrolled 75 kids with ASA I or II who were booked for day-case unilateral lower abdominal operations randomly assigned to caudal block and TAP block groups. The two groups were equal as regard intraoperative fentanyl administration, requested postoperative tramadol, time to first rescue analgesia, postoperative pain scores, and post anesthesia care unit time. Compared to the caudal group, children in the TAP group were sent home far sooner. Comparing TAP group to caudal group, the parent satisfaction score was statistically considerably higher in the TAP group. The reasons for the improved satisfaction, however, may differ from those in their study because our study attributed it to less rescue postoperative analgesia and lower pain scores while their study attributed it to fewer side effects and quicker achievement of criteria for home discharge in children with TAP.
As regard hemodynamic effects, in current study there was statistical significant difference observed between caudal and ultrasound-guided (TAP) block groups with regard to intraoperative mean arterial blood pressure (MAP), where blood pressure decreased in the caudal group more than the (TAP) group 10 minutes after the block, at skin incision, 25 min, 40 min, and at the end of operation however all readings were in the clinically accepted range, this could be related to the hypotensive effect of the neuraxial blocks.
Our study agreed with the results of Ashrey and Bosat [22] who reported significant decrease in MAP and the HR in caudal group compared with penile block group due to the inhibitory effect of bupivacaine on the sympathetic nervous system without significant increase in the rate of adverse events.
However, our results contradicted with those of Galante et al. [23] that proved by using transesophageal Doppler in a study of 62 pediatric patients, 6 months to 7 years old, ASA I-II who undergone genitourinary surgery that balanced general anesthesia with either caudal levobupivacaine or remifentanil infusion did not differ in hemodynamic parameters. Both techniques demonstrated excellent hemodynamic stability with only slight variations from the baseline across the time, which are of no clinical importance with possible exception in patients who already have cardiovascular dysfunction. To fully comprehend the effects of caudal blockage on cardiac output and regional blood flow in children, further studies with noninvasive monitoring in a larger population are necessary.
In our study both caudal and transversus abdominis plane (TAP) blocks with ultrasound guidance offered effective postoperative pain management during the first two hours postoperatively indicated by no significant rise in mean arterial blood pressure (MAP), heart rate, and modified objective pain score (MOPS) in both groups.
But starting from the second hour postoperatively there was a distinct rise in heart rate (P <0.05) and significant increase in MOPS (P<0.001), while the statistical significant difference in MAP(P<0.05) between the two groups disappeared due to MAP increase in caudal group in comparison to TAP group, which indicated inadequate analgesia provided by caudal block after 2 hours postoperatively compared to transversus abdominis plane (TAP)block with ultrasound-guidance.
Also, in current research the duration of postoperative analgesia which was determined by the time to first need of rescue analgesia (paracetamol suppository 20 mg/Kg) was much longer in the ultrasound-guided TAP group (mean ± SD = 648±154.9 min) compared to (mean ± SD = 227± 81.2 min) in caudal group. This was considered as advantage of transversus abdominis plane (TAP) block with ultrasound-guidance which had longer duration of action.
This was in line with a study done by Kodali et al. [24], who found that children underwent TAP block had longer analgesic duration and reduced scores of pains in comparison to those who were given caudal analgesia evidenced by decreased rescue analgesic dosage with no significant side effects after inguinal herniotomy.
In another study ten pediatric patients, aged between 10 months and 8 years were examined by Tobias [25] guided by ultrasound, TAP block was applied to both flanks using 0.25% bupivacaine, 0.3 mL/kg plus adrenaline 1:200,000 at the end of surgery. The TAP block was deemed to be effective because no postoperative painkiller was needed for the first 7-11 hours following surgery.
Additionally, our findings supported those of a study by Carney and his colleagues [26] on forty appendectomy patients who were randomly allocated to receive a unilateral TAP block with ropivacaine (n = 19) against a placebo (n = 21) beside the usual postoperative pain relief using IV morphine, diclofenac, and acetaminophen. They found that TAP block using ropivacaine decreased the mean (±SD) morphine consumption during the first 48 hours postoperatively (10.3 ± 12.7 vs 22.3 ± 14.7 mg; P< 0.01) in comparison to placebo block. Additionally, TAP block decreased visual analogue pain scale postoperatively both at rest and when moving in comparison to placebo. Throughout the first 24 hours postoperatively, there was a reduction in interval morphine administration. The TAP block wasn’t the cause of any postoperative complications.
Our results were not coincided with those of Niraj et al. [27] who evaluated the pain relieving potency of Subcostal transversus abdominis plane (TAP) catheters against that of epidural anesthesia following upper abdominal operations in a randomized controlled study, beside the postoperative analgesic regimen consisted of paracetamol and tramadol as needed, and discovered no statistically significant variations in visual analogue scores (VAS) among epidural group (4.0 (2.5–5.3)) and TAP group. The TAP group consumed considerably more tramadol (p = 0.002).
Fredrickson et al. [28] also compared 20 Single shots ultrasound-guided posterior approach TAP blocks against 21 ilioinguinal blocks in children, Aged 6 months to 12 years undergone elective inguinal surgery, regarding post-operative pain score, consumption of analgesia, and parental satisfaction, they found that the TAP group experienced more frequent pain and used ibuprofen more frequently during the recovery period.
Also Sandeman et al. [29] performed a study on 87 patients aged 7–16 years undergone laparoscopic appendectomy, of which 45 controls received skin infiltration with ropivacaine against 42 patients received bilateral single shot posterior Approach TAP blocks with ultrasound-guidance using 0.2% ropivacaine (0.5 ml/kg) (total 2 mg/kg) then, compared the percent of patients required>0.2 mg/kg of Morphine postoperatively. They found no changes in total postoperative opioid administration. Nonetheless, TAP block group patients had improved postoperative pain management (median score 0 vs 2). However, in that study a greater proportion of patients from TAP group suffered complicated appendicitis from the start (TAP 13/42 (31%), control 5/45 (11%), P<0.02] which may account for the increased need of postoperative analgesia in TAP group.
In the present study, as regard incidence of complications there was one case of out of plane injection in ultrasound TAP group while, there were two cases of intravascular puncture and one case of subcutaneous injection in the caudal group. All these cases with recorded complications were excluded from our study.
This coincided with the results of Fredrickson and Seal [30] who described four newborns who had abdominal operations and received intraoperative and early postoperative pain management using transversus abdominis plane block (TAPB) and stated that transversus abdominis plane bock with ultrasound-guidance is an essentially suitable substitute to local anesthetic infiltration of the wound in newborns.
Also, in another study done by Carney and his colleagues [26] on forty children undergone appendectomy, they didn’t detect any adverse effects related to the TAP block.
This was agreed also by the study of Al-Sadek and her colleagues [20] who concluded that TAP block guided by ultrasound visualization, was simple to apply and was safe hemodynamically with no documented intra- or postoperative adverse effects.
However, the complications documented with TAP block has been mentioned in the literature by Farooq and Carey [31] who described an incident of liver injury with a blunt local anesthetic needle during execution of TAP block. However, because they only used the blind “double-pop” approach for the block, they were unable to assess the anatomical structures or the precise placement of the needle.
On the other hand, “Caudal epidural anesthesia was considered to be safe and easy to perform”. Giaufre and his colleagues [32] stated that statement after analysis of 84412 anesthetic procedures of which 24409 had been managed with regional blocks (50% was by caudal epidural anesthesia) and reported only complications of eight patients with dural perforation, four unintended spinal, two convulsions (due to unintended intravascular infusion), and one case of rectal perforation.
Also, Aprodu and his colleagues [33] studied the safety and effectiveness of caudal analgesia on intra and postoperative pain relief in 150 children scheduled for various surgical procedures and revealed that, the estimated incidence of complications was 13.33%. The most common adverse event was retention of urine (5.33%).
In comparison to the popular caudal analgesia, our research showed that TAP block could give good analgesia after a variety of lower abdominal surgeries. As in TAP block we could avoid needle insertion close to neuraxial region or peripheral motor nerves, it can be successfully performed on patients with vertebral abnormalities and can be done right after general anesthesia induction. To increase precision and reduce the possibility of unintentional harm to intraperitoneal components, ultrasound guidance should be used. Local anesthetic toxicity is the most likely significant adverse event when using any regional anesthetic technique on infants and children, hence it is crucial to pay close attention to both concentration and volume. The total dose of bupivacaine should not be more than 3 mg/kg.
Conclusion
We concluded from present study that although caudal epidural anesthesia for children has a similar effectiveness as transversus abdominis plane block with ultrasound-guidance regarding intraoperative and immediate postoperative pain relief, yet the ultrasound guidance of transversus abdominis plane block offered the advantages of direct vision of muscles and nearby structures. The close ultrasound monitoring of local anesthetic diffusion in allowed space increased success rate and maintained the quality of the block. Also, transversus abdominis plane block with ultrasound-guidance was safe hemodynamically with no documented intra- or postoperative adverse events and had longer duration as regard postoperative analgesia.
Limitations of the Study
Some probable restrictions on our study must be taken into account. First, the research only considered the first 12 hours following surgery when assessing postoperative analgesia. Meanwhile, it has been proven that the TAP block results in clinically beneficial degrees of postoperative analgesia. Second, we did not qualify sevoflurane’s impact on postoperative agitation into account.
Conflict of interest
No conflict of interest.
References
- Wang KS, Papile L-A, Baley JE, Benitz W, Cummings J, Carlo WA, et al. (2012) Assessment and management of inguinal hernia in infants. Pediatrics. 130(4): 768-773.
- Aiken JJ (2004) Inguinal hernias. In: Behman RE, Kliegman RM, Jenson HB. (Eds) Nelson Textbook of Pediatrics. 17th, Saunders, Philadelphia. p.1293.
- Morgan GE, Mikhail MS, Murray MJ (2022) Clinical anesthesiology. In: Paediatr Anaesth Chapter 42, Pp: 1441-1487.
- Ecoffey C, Lacroix F, Giaufré E, Orliaguet G, Courrèges P (2010) Epidemiology and morbidity of regional anesthesia in children: a follow‐up one‐year prospective survey of the French‐Language Society of Paediatric Anaesthesiologists (ADARPEF). Paediatr Anaesth 20(12): 1061-1069.
- Guay J, Suresh S, Kopp S (2019) The use of ultrasound guidance for perioperative neuraxial and peripheral nerve blocks in children. Cochrane Database Syst Rev 17(2): 74-79.
- Shah R, Suresh S (2013) Applications of regional anaesthesia in paediatrics. Br J Anaesth 111(Suppl 1): i114-i124.
- Murni Sari Ahmad A, Azarinah I, Esa K, Khairulamir Z, Hamidah I, et al. (2015) Intravenous dexamethasone in combination with caudal block prolongs postoperative analgesia in pediatric daycare surgery. Middle East J Anaesthesiol 23(7): 177-183.
- Mirjalili SA, Taghavi K, Frawley G, Craw S (2015) Should we abandon landmark‐based technique for caudal anesthesia in neonates and infants? Paediatr Anaesth 25(5): 511-516.
- Abdallah F, Laffey J, Halpern S, Brull R (2013) Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth 111(5): 721-735.
- Mai CL, Young MJ, Quraishi SA (2012) Clinical implications of the transversus abdominis plane block in Paediatr Anaesth Paediatr Anaesth 22(9): 831-840.
- Long JB, Birmingham PK, De Oliveira Jr GS, Schaldenbrand KM, Suresh S (2014) Transversus abdominis plane block in children: a multicenter safety analysis of 1994 cases from the PRAN (Pediatric Regional Anesthesia Network) database. Anesth Analg 119(2): 395-399.
- Wilson GAM, Doyle E (1996) Validation of three pediatric pain scores for use by parents. Anesthesia 51(11): 1005-1007.\
- Sethi N, Pant D, Dutta A, Koul A, Sood J, et al. (2016) Comparison of caudal epidural block and ultrasonography-guided transversus abdominis plane block for pain relief in children undergoing lower abdominal surgery. J Clin Anesth 33(6): 322-329.
- Morton NS, Errera A (2010) APA national audit of pediatric opioid infusions. Paediatr Anaesth 20(2): 119-125.
- Marhofer P, Greher M, Kapral S (2006) Ultrasound guidance in regional anaesthesia. Br J Anaesth 94(1): 7-17.
- Frederickson M (2008) Early experience with the transversus abdominis plane block in children. Paediatr Anaesth 18(6): 891-892.
- Baeriswyl M, Zeiter F, Piubellini D, Kirkham KR, Albrecht E (2018) The analgesic efficacy of transverse abdominis plane block versus epidural analgesia: a systematic review with meta-analysis. Medicine (Baltimore) 97(26): 78-79.
- Kumar A, Dogra N, Gupta A, Aggarwal S (2020) Ultrasound-guided transversus abdominis plane block versus caudal block for postoperative analgesia in children undergoing inguinal hernia surgery: A comparative study. J Anaesthesiol Clin Pharmacol 36(2): 172.
- Jacobs A, Bergmans E, Arul GS, Thies KC (2011) The transversus abdominis plane (TAP) block in neonates and infants–results of an audit. Paediatr Anaesth 21(10): 1078-1080.
- Al-Sadek WM, Rizk SN, Selim MA (2014) Ultrasound guided transversus abdominis plane block in pediatric patients undergoing laparoscopic surgery. Egyptian Journal of Anaesthesia 30(3): 273-278.
- El Fawy DM, El Gendy HA (2014) Ultrasound-guided transversus abdominis plane block versus caudal block for postoperative pain relief in infants and children undergoing surgical pyeloplasty. Ain-Shams Journal of Anaesthesiology 7(2): 177-184.
- Ashrey EM, Bosat BE (2014) Single-injection penile block versus caudal block in penile pediatric surgery. Ain-Shams Journal of Anaesthesiology. 7(3): 428-431.
- Galante D, Pellico G, Meola S, Caso A, De Capraris A, et al. (2008) Hemodynamic effects of levobupivacaine after pediatric caudal anesthesia evaluated by transesophageal doppler. Paediatr Anaesth 18(11): 1066-1074.
- Kodali VR, Kandimalla A, Vakamudi M (2020): Comparison of analgesic efficacy of ultrasound-guided transversus abdominus plane block and caudal block for inguinal hernia repair in pediatric population: A single-blinded, randomized controlled study. Anesth Essays Res 14(3): 478-482.
- Tobias JD (2009) Preliminary experience with transversus abdominis plane block for postoperative pain relief in infants and children. Saudi Journal of Anaesthesia 3(1): 2-9.
- Carney J, Finnerty O, Rauf J (2010) Ipsilateral transversus abdominis plane block provides effective analgesia after appendectomy in children: a randomized controlled trial. Anesth Analg 111(7): 998-1003.
- Niraj G, Kelkar A, Fox A (2010) Application of the transversus abdominis plane block in the intensive care unit. Anaesth Intensive Care 37(4): 650-652.
- Fredrickson MJ, Paine C, Hamill J (2010) Improved analgesia with the ilioinguinal block compared to the transversus abdominis plane block after pediatric inguinal surgery: a prospective randomized trial. Pediatr Anesth 20(7): 1022–1027.
- Sandeman D, Bennett M, Dilley AV, Perczuk A, Lim S, et al. (2011) Ultrasound-guided transversus abdominis plane blocks for laparoscopic appendicectomy in children: a prospective randomized trial. Br J Anaesth 106(6): 882-886.
- Fredrickson M, Seal P (2009) Ultrasound-guided transversus abdominis plane block for neonatal abdominal surgery. Anaesthesia and intensive care. 37(3): 469-472.
- Farooq M, Carey M (2008) A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane\ block. Reg Anesth Pain Med 33(6): 274-275.
- Giaufre E, Dalens B, Gombert A (1996) Epidemiology and morbidity of regional anesthesia in children: a one-year prospective survey of the French-Language Society of Pediatric Anesthesiologists. Anesth Analg 83(5): 904-912.
- Aprodu G, Munteanu V, Filciu G, Goţia D (2008) Caudal anesthesia in pediatric surgery. Rev Med Chir Soc Med Nat Iasi 112(1): 142-147.






























