An Alternative Technique in Case of PICC Difficult Implantation
Remo Caramia1*, Giuseppina Caputi1, Ludovico Galiano2, Francesco Mangini3 and Pietro Fedele1
1Anesthesia, Resuscitation and Pain Therapy Unit, “D. Camberlingo” Hospital, Francavilla Fontana (BR), Italy
2Radiology Unit, “D. Camberlingo” Hospital, Francavilla Fontana (BR), Italy
3ICU/Cardiology Unit, “D. Camberlingo” Hospital, Francavilla Fontana (BR), Italy
Submission: August 23 2022; Published: September 23, 2022
*Corresponding author: Remo Caramia, Anesthesia, Resuscitation and Pain Therapy Unit, “D. Camberlingo” Hospital, Francavilla Fontana (BR), Italy
How to cite this article: Remo C, Giuseppina C, Ludovico G, Francesco M, Pietro F. An Alternative Technique in Case of PICC Difficult Implantation. J Anest & Inten care med. 2022; 12(2): 555833. DOI 10.19080/JAICM.2022.12.555833
Abstract
Background: Peripherally inserted central catheters are central venous access devices designed for intermediate to long-term use, which are usually placed via a peripheral upper arm vein (i.e., basilica, brachial or cephalic vein) with the catheter tip placed at the distal third of the superior vena cava. In some cases, it is difficult to correctly position the PICC in its ideal location.
Objective: In cases where it is not possible to target the catheter tip correctly, before giving up the technique or trying the contralateral arm, we have developed a technique that allows you to be successful in most of these difficult cases using a preformed guide wire.
Results and Conclusion: In our experience we have been successful in almost all cases and no short or long-term complications occurred.
Keywords: Peripherally Inserted Central Catheter; Difficult Placement; Guide Wire; Tip Location; New Technique
Introduction
Peripherally inserted central catheters (PICCs) are central venous access devices which are usually placed via a peripheral upper arm vein (i.e., basilica, brachial or cephalic vein) with the catheter tip placed at the distal third of the superior vena cava (SVC). The average time in situ ranges between 1 week and 6 months; longevity of up to 1 year has been described.
They offer the advantages of greater safety for infusion of vesicant/irritant and hyperosmolar solutions and enable administration of antibiotics, prolonged parenteral nutrition, and chemotherapy agents [1].
In some cases, it is difficult to correctly position the PICC in its ideal location. Tip location and tip navigation techniques are useful and indispensable for establishing the correct position of the catheter tip. The most used method currently is the intracavitary ECG [2].
Unfortunately, in some cases the catheter does not follow the correct intravenous route along the SVC but deviates towards the ipsilateral internal jugular vein or the contralateral anonymous vein.
The operator from the outside can try to correctly target the catheter, compressing the jugular vein or changing the position of the arm.
Although the technical success rate of PICCs has been reported to be 74-100%, in patients with unsuspected asymptomatic venous steno-occlusive lesion (VSOL), there might be difficulties in performing the procedures regardless of whether the catheter is placed through the VSOL or through other venous access routes [3].
In cases where it is not possible to target the catheter tip correctly, before giving up the technique or trying the contralateral arm, we have developed a technique that allows you to be successful in most of these difficult cases.
Methods
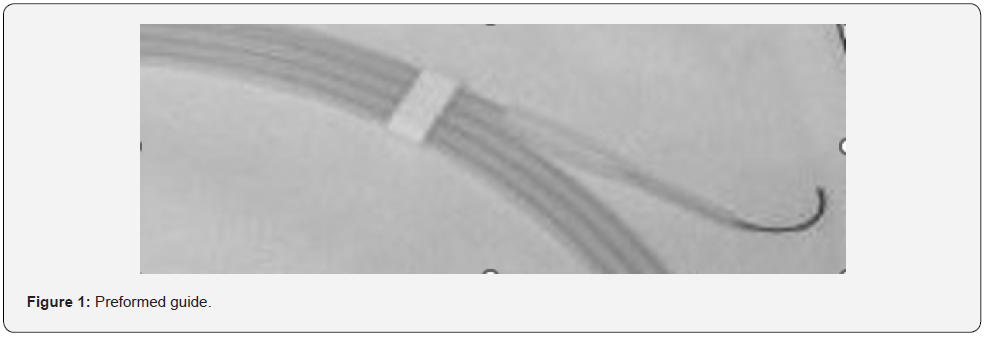
We use a preformed guide that manages to project towards the superior vena cava (Radifocus™ Guide Wire M, Terumo Interventional System) (Figure 1). This device is a nitinol hydrophilic guide wire covered with polyurethane containing a hydrophilic polymer coating for low friction, designed to direct a catheter in the vascular system has a rounded, atraumatic curved tip, features adaptable shape memory and high flexibility prevents kinking, is radiopaque and is often used in interventional radiology procedures.
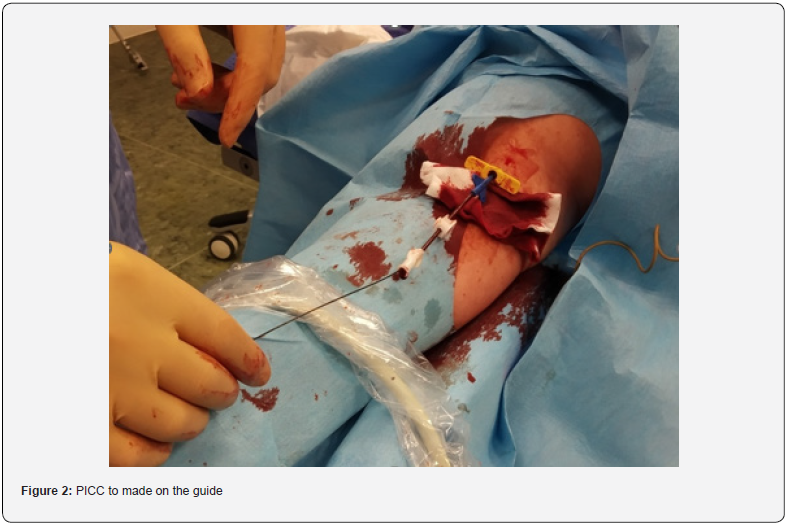
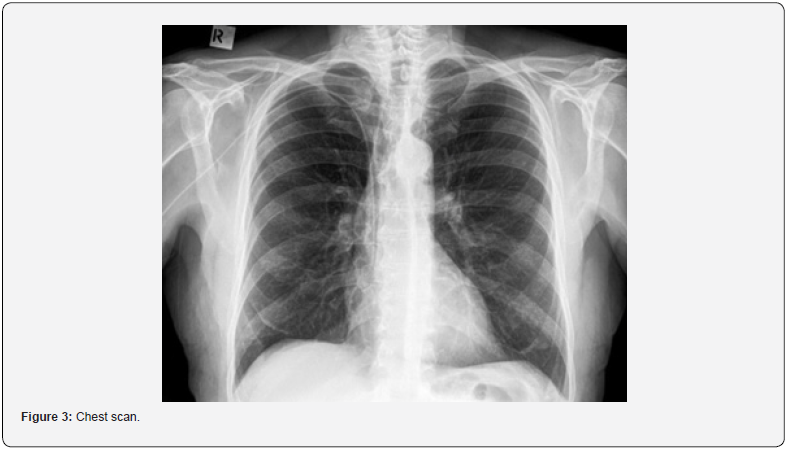
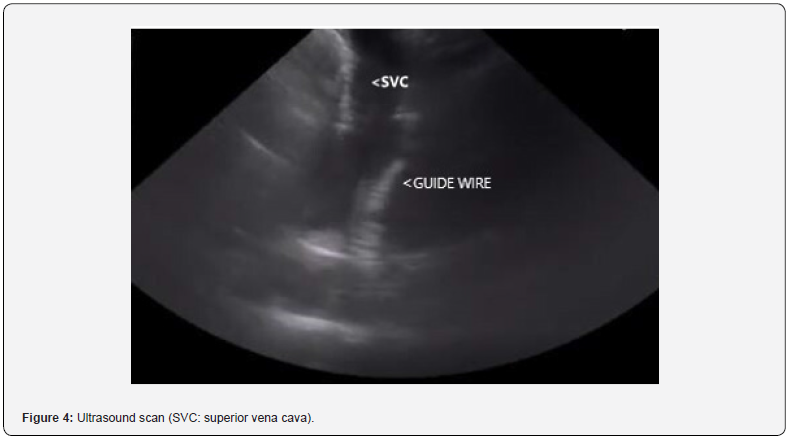
The guide is passed through the introducer and subsequently, with the direct Seldinger technique, the venous catheter (Delta Med® PICC power, 4 FR single lumen) (Figure 2) is made to slide on the guide that allows to take the right direction, finally the guide is removed, and the position is checked of the tip with the usual techniques using the intracavitary ECG. Correct direction can be checked with a chest scan [4] (Figure 3) or with ultrasound confirmation via a right supraclavicular fossa view before removing the guide [5,6] (Figure 4).
Results
In our experience, which we specify, however, counts few cases, we have been successful in almost all cases (9/10) and no short or long-term complications occurred in a manner different from PICCs implanted according to the classical technique.
Discussion
The aspect that we want to underline concerns the fact that this technique does not solve all the problems and is not an alternative to others, on the contrary it shows currently evident limits.
First, the guide we use is made up of material that does not conduct the ECG, therefore the verification of the correct direction is inferred from indirect evaluations: absence of the same in the ultrasound scans in the jugular vein or in the contralateral anonymous vein; or through direct evaluation with fluoroscopy and ultrasound confirmation which however requires a learning curve.
Then the diameter of the guide is only slightly smaller than that of a 4 FR catheter and it must be well “lubricated” with saline solution to make it slide along the guide. Proximal cut catheters cannot be used due to a slight narrowing at the tip that prevents passage.
Finally, after inserting the PICC and removing the guide, it is necessary to precisely check the position of the tip in the correct area.
Despite these limitations, however, it remains, in our opinion, a possible alternative to failure, as we have demonstrated.
These limits could be overcome if we could have available a guide with slightly different characteristics: slightly smaller diameter to make the catheter slide better, material capable of conducting the electrical impulses of the ECG and with clearly visible centered measurement, to verify its correct positioning before passing the catheter. The tip should always remain soft and curved.
Conclusion
We have used a preformed guide to be successful in inserting the PICC when correct advancement in the vena cava is difficult before giving up the technique or trying the contralateral arm. Our technique was effective, safe, and cost-effective in the patients in which it was employed.
Acknowledgements
We thank all the nursing team of the Anesthesia, Pain Therapy and Vascular Access Unit for their collaboration.
Conflicts of Interest and Funding
No conflicts of interest and no funding to declare.
Ethical Considerations
All persons gave their informed consent prior to their inclusion in the study and all ethical principles have been respected. The local ethics committee was notified of the study.
References
- Gonella S, Antonuzzo A, Bossi P (2021) Peripherally or centrally inserted central catheters: what is the best vascular access device for cancer patients? Support Care Cancer 29(6): 2803-2806.
- Sun W, Li J, Liu B, Liu Y, Ge R et al. (2021) Effects of indwelling centrally inserted central catheter on tip location of peripherally inserted central catheter with intracavitary electrocardiogram guidance: A retrospective case-control study. J Vasc Access 23: 11297298211015088.
- Yang WJ, Kang D, Shin H, Jang EH, Noh SY, et al. (2021) Comparison of different techniques for the management of venous steno-occlusive lesions during placement of peripherally inserted central catheter. Sci Rep 11(1): 10234.
- Erskine B, Bradley P, Joseph T, Yeh S, Clements W (2021) Comparing the accuracy and complications of peripherally inserted central catheter (PICC) placement using fluoroscopic and the blind pushing technique. J Med Radiat Sci 68 (4): 349-355.
- Adrian M, Kander T, Lundén R, Borgquist O (2022) The right supraclavicular fossa ultrasound view for correct catheter tip positioning in right subclavian vein catheterisation: a prospective observational study. Anaesthesia 77(1): 66-72.
- Greca AL, Iacobone E, Elisei D, Biasucci DG, D'Andrea V, et al. (2021) A structured protocol for ultrasound-based tip navigation and tip location during placement of central venous access devices in adult patients. J Vasc Access 11297298211044325 doi: 10.1177/11297298211044325.






























