Retrospective Study about Standard Coagulation Test Alterations in Major Burns and its Clinical Relevance
Patricia Guilabert1*, Gemma Usua1, Carlos Muñoz1, Roger Moreno1, Juan P Barret2 and Maria J Colomina3
1Department of Anesthesia and Critical Care, University Hospital Vall d’Hebron, Autonomous University of Barcelona, Spain
2Department of Plastic Surgery and Burn Centre, University Hospital Vall d’Hebron, Autonomous University of Barcelona, Spain
2Department of Anesthesia and Critical Care, University Bellvitge Hospital, University of Barcelona, Spainn
Submission: December 09 2021; Published: May 20, 2022
*Corresponding author: Patricia Guilabert Anesthesia and Critical Care Department. University Hospital Vall d’Hebron. Autonomous University of Barcelona. Barcelona, Spain
How to cite this article: Patricia G, Gemma U, Carlos M, Roger M, Juan P B, et al. Retrospective Study about Standard Coagulation Test Alterations in Major Burns and its Clinical Relevance. J Anest & Inten care med. 2022; 12(2): 555831. DOI 10.19080/JAICM.2022.12.555831
Abstract
Background: In the days following heat trauma, major burn patients (MBP) present a multifactorial coagulation disorder known as acute burn-induced coagulopathy. Some studies have reported early alterations in prothrombin and partial thromboplastin times in 30%-40% of these patients, and have associated these alterations with burn severity and evolution.
Objective: To describe alterations in standard coagulation tests in major burn patients and their clinical relevance.
Methods: Retrospective observational study performed in the Burn Unit of the tertiary referral Vall d’Hebron University Hospital to determine early alterations in standard coagulation tests in MBPs between 1 January 2013 and 31 December 2019. Analysis of mortality and transfusion rates.
Results: Of the 90 patients finally included in the study, 66.7% presented some type of alteration in coagulation tests. ROC curve analysis showed that patients with an Abbreviated Burn Severity Index score ≥ 8 and a total body surface area ≥ 32% were more likely to present alterations in standard coagulation tests. Significant difference in 28-days mortality were observed - 25% in patients with coagulation abnormalities compared to 6.7% in those without. Patients with coagulation abnormalities required significantly more red blood cells and fresh frozen plasma.
Conclusion: Abnormalities in standard coagulation tests are associated with burn severity and affect transfusion rates and mortality. The significance of these abnormalities in the overall coagulation status of MBPs has yet to be defined.
Keywords:Burns, blood coagulation, prothrombin time, partial thromboplastin time, blood coagulation tests, blood coagulation disorders
Visual Abstract

Background
In the days following heat trauma, many major burn patients (MBP), defined as burns covering ≥ 20% of the body surface area [1], present a multifactorial coagulation alteration [2] known as acute burn-induced coagulopathy (ABIC). ABIC is mainly the result of trauma-induced activation of the extrinsic coagulation pathway, hypothermia, hypoperfusion, acidosis, and activation of the inflammatory cascade [2-5]. Subsequent blood loss from surgical procedures and possible sepsis will also affect coagulation in these patients [2].
Although some studies have already investigated MBPs, the pathophysiology and immunochemistry of the coagulation and anticoagulation mechanisms activated during the evolution of these patients are not fully understood [2,6]. Studies performed so far have evaluated the different factors involved in the coagulation process, and the results suggest that the MBP will progress from an initial hypocoagulable state to a hypercoagulable state [4,7,8] that can even lead to disseminated intravascular coagulation [9,10].
Miter et al. [7] define ABIC as an international normalised ratio (INR) value higher than 1.5 or activated partial thromboplastin time (aPTT) of more than 60 seconds, while (Sherren et al.) define it as an INR of more than 1.2 and aPTT of more than 45 seconds. In both studies [4,7] ABIC appears in 35%-40% of MBPs and is determined by abnormalities in standard coagulation tests (prothrombin time (PT) and aPTT), with prolonged PT being more common than prolonged aPTT. This coagulation abnormality appears to correlate with both the severity of the initial trauma and the prognosis [4,7,11]. However, ABIC has not yet been clearly defined, and does not appear in coagulation studies performed using viscoelastic techniques [2,12-15]. Other factors, such as fibrinogen [2] and platelets [16], will increase 48 hours and 7 days after the injury, respectively, leading to the hypercoagulability found in the MBP. Unfortunately, because of the low incidence of major burns, there is insufficient scientific evidence to confirm these finding, and few articles have been published in this regard.
The objective of this study has been to assess the incidence of ABIC in MBPs based on PT and aPTT. We also compared the presence of this alteration with burn severity measured with the Abbreviated Burn Severity Index (ABSI) and with mortality.
Methods
Setting
The Burn Unit of the Vall d’Hebron University Hospital (VHUH) is the reference centre for all burn patient in Catalonia, the Balearic Islands and Andorra, with a total population of 8.4 million. In 2019 it was accredited as a verified burn centre by the European Burns Association - the only Spanish hospital to have received this recognition. Burns cause 1800 emergencies per year, 352 acute surgeries and about 30 interventions for sequelae. Of the total number of patients seen annually about 60 are classified as MBPs because they present burns on a body surface greater than 15%, or greater than 10% in patients aged over 65 or under 10 years of age.
Given the scarcity of studies published in major burns to date, we considered the status of our hospital as a tertiary burns centre to be an appropriate setting for a study to determine the incidence, possible causes, and consequences of ABIC.
Patients
Burn patients over 18 years of age with a burned body surface greater than or equal to 20% who were admitted between 1 January 2013 and 31 December 2019 were included in the study. Exclusion criteria: Patients transferred to other hospitals before the end of the study period; patients who did not undergo coagulation tests in the first 6 hours after the thermal trauma and 24 hours after admission; patients treated with anticoagulants; patients with known coagulation disorders; or multiple trauma patients in whom coagulopathy would not be caused by the burn but by the multiple trauma.
Study Design
This is a retrospective observational study on abnormalities observed in basic coagulation tests in the initial phase of burn trauma in MBPs between January 1, 2013, and December 31, 2019, approved by the VHUH Ethics Committee under registration number PR (ATR) 367/2016.
Demographic variables: Age, gender, ABSI, percentage of total body surface area (TBSA) burned, smoke inhalation, and thirddegree burns.
Other clinical variables collected were: Prothrombin time ratio (PTr) or INR and activated partial thromboplastin time ratio (aPTTr) at admission (first 6 hours after thermal trauma) and at 24 hours; time (days) needed to correct the coagulation alteration; blood transfusion due to coagulopathy (according to the information noted in the clinical and laboratory history and data obtained from the blood bank registry) or equivalent time in patients who did not present alterations; persistence of ABIC on the day of surgery; 28-day mortality; 90-day mortality; and cause of death.
Coagulation alterations were defined as values greater than 1.2 for PTr or INR and aPTTr, according to the upper limit of normal defined by the VHUH laboratory and the recent definition of acute traumatic coagulopathy (ATC) used by Davenport et al. [17]. Coagulopathy was defined as clinically significant if clotting agents (prothrombin complex, fibrinogen, tranexamic acid or others) were administered at the discretion of the attending physician, and not significant if it was self-limiting.
Data Collection
The clinical history was retrieved from the electronic health record data base where all clinical data are stored, using SAP Frond End®. We performed a structured review of the admission report, lab tests performed, blood bank records, and the clinical course annotated in the medical record.
Statistical analysis
Qualitative variables were described as frequencies and percentages and quantitative variables as mean (standard deviation) and median (interquartile range). The Chi square or Fisher’s exact tests were used to correlate the qualitative variables with the outcome variables (resolution, death at different time points, etc.), and the student’s t or U Mann-Whitney nonparametric test, according to the symmetry of the variable, were used to compare differences between quantitative variables in groups. A ROC curve was plotted for the ABSI and TBSA variables to find the point with the best sensitivity and specificity according to the Youden index. Multivariate analysis could not be performed due to a lack of n.
Results
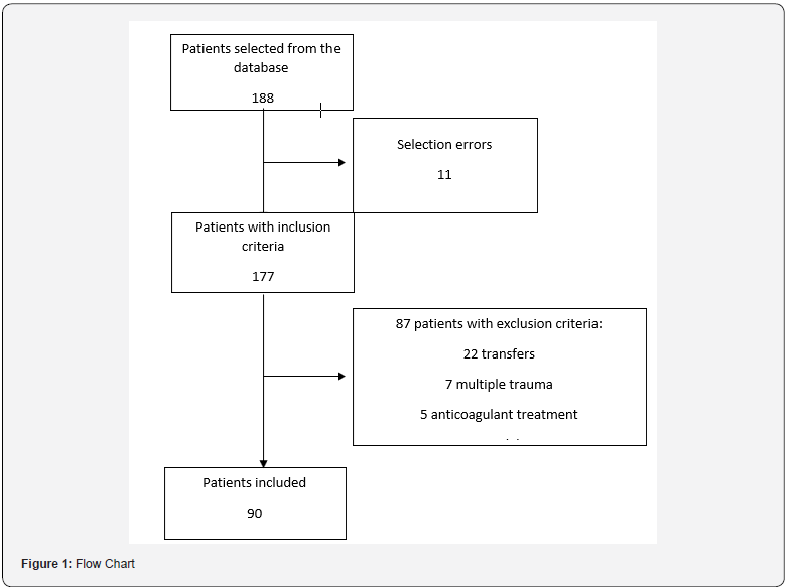
In total, 188 patients with burns greater than or equal to 20% TBSA were registered in the database during the study period. Of the 188 potential study patients, 1 was duplicated and 10 did not meet the inclusion criteria. Of the remaining 177, 87 met one or more of the exclusion criteria (22 were transferred without completing the study period, 7 had associated trauma, 5 were on anticoagulant treatment, some lab samples were missing in 43 cases, and 8 died before extractions were performed). This gave a total of 90 patients for inclusion in the study (Figure 1).
Ninety patients were finally included in the study. The mean age was 50 years, mean ABSI score was 8, and mean TBSA was 37.7% (Table 1); 27.8% were women, 43.3% presented third degree burns, and 23.3% presented smoke inhalation.
Many (66.7%) presented some type of coagulation abnormality according to our definition: 14.4% with PT alterations, 5.6% with aPTT alterations, and in 46.7% both parameters were altered.
When coagulopathy was broken down by type (PT alteration, aPTT alteration, or both), it was observed that patients with aPTT alterations had higher ABSI scores, greater TBSA, and were more likely to have suffered smoke inhalation.
Coagulation abnormalities correlated significantly with third degree burns, ABSI score, TBSA, and smoke inhalation in the univariate analysis (Table 1), and the ROC curve showed that patients with ABSI ≥ 8 and TBSA ≥ 32% were more likely to present coagulopathy.
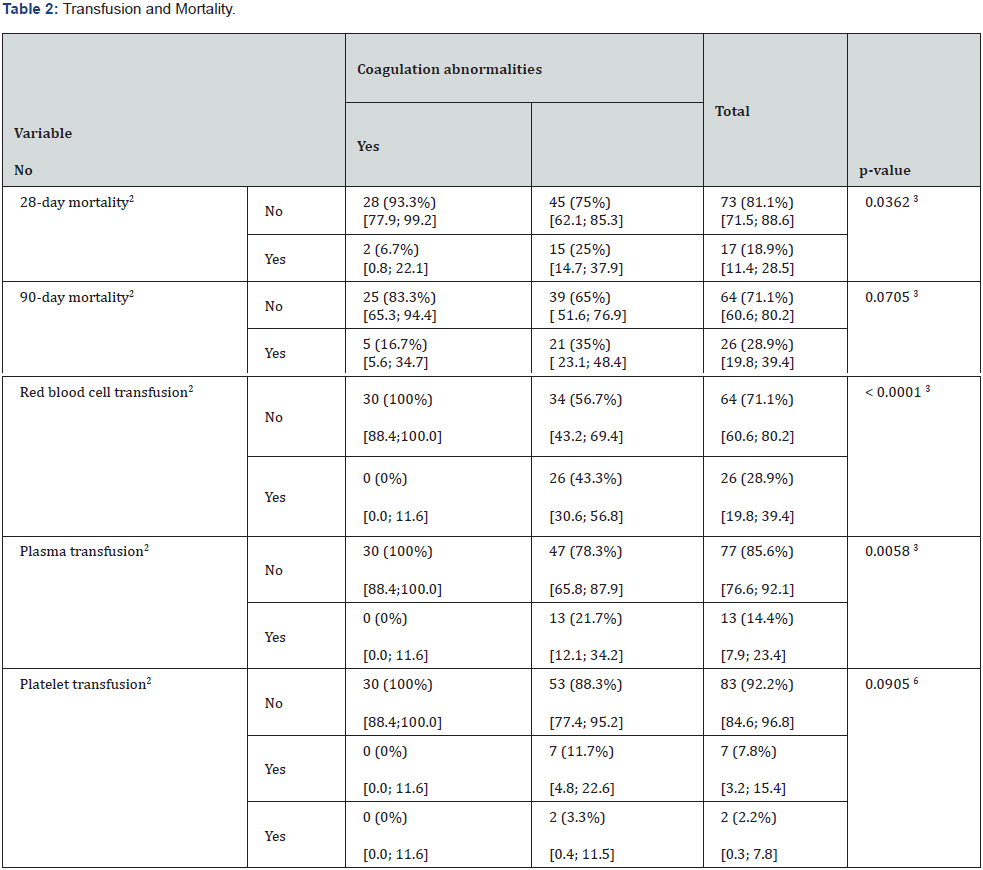
Patients with coagulation alterations required red blood cell (RBC) transfusion in 43.3% of cases and fresh frozen plasma (FFP) in 13%; in patients with no coagulation alterations only 10% received RBCs and none required FFP, both differences being statistically significant. With regard to platelets, 11.7% of patients with coagulation alterations and 0% of those without received transfusions (p = 0.0905). No differences were found in consumption of blood product or haemostatic agents among patients with PT, aPTT or PT + aPTT abnormalities (Table 2).
In total, 86.7% of coagulation alterations were corrected, 100% in those with altered PT, 80% in those with altered aPTT, and 83.3% in those with altered PT + aPTT. The median number of days required to correct the alterations was 4 days for PT, 4 for aPTT, and 5 for patients with PT + aPTT, with a global median of 5 days (Table 3).

1: n (row percentage),
[95% Confidence Interval]
2: n (column percentage)
[95% Confidence Interval]
3: Chi-squared test
4: N
Arithmetic mean (SD)
[95% Confidence Interval]
Median (P25; P75)
5: t-test / U Mann-Whitney test
1: n (row percentage)
[95% Confidence Interval]
2: n (column percentage)
[95% Confidence Interval]
3: Chi-squared test
4: N
Arithmetic Mean (SD)
[95% Confidence Interval]
Median (P25; P75)
5: t-test / U Mann-Whitney test
6: Fisher’s exact test

1: N
Arithmetic mean (SD)
Median (P25; P75)
Minimum / Maximum
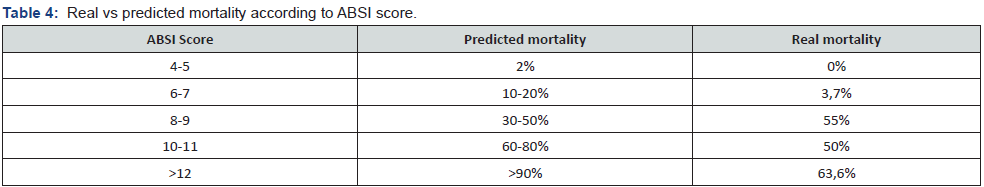
Mortality according to ABSI was 0% in patients with a score of 4-5, 3.7% with a score of 6-7, 55% with a score of 8-9, 50% with a score of 10-11, and 63.6% with a score ≥ 12; overall mortality was lower than predicted [18] given the severity of the patients in almost all scores ranges (Table 3). Less than half (40.74%) of all patients died from sepsis, 25.92% died from multiple organ failure, 18.51% from respiratory failure, 3.7% from airway problems, and 11.11% from other causes.
A significant difference in 28-day mortality was observed between patients with coagulation alterations (25%) versus those without (6.7%) (p = 0.0362) Ninety-day mortality in patients with coagulation alterations was 35% versus 16.7% in those without, p = 0.0705. There were no significant differences between the different types of alteration. Consumption of blood products and clotting agents did not correlate with higher mortality. Twentyeight- day (87.5% vs 15.4%) and 90-day (87.5% vs 26.9%) mortality were higher in patients in whom coagulation alterations were not corrected; these differences were significant. In some cases, patients entered the operating room with some type of persistent coagulation abnormality, but this did not lead to an increase in 28-day or 90-day mortality. All patients who did not undergo surgery and who presented persistent coagulopathy died within 28 days.
Discussion
In our study, coagulation alterations were observed in 66.7% of major burn patients. This incidence is higher than that described in previous studies [4,7,19]. Lu et al. [20] did not describe ABIC in their series, and Sherren et al. [4] and Mitra et al. [7] recorded an incidence of 39% and 37%, respectively. These differences could be due to the parameters used to define coagulation alteration - our criteria were more inclusive than Sherren et al. [4] (INR > 1.2, aPTT > 45s), Mitra et al. [7] (INR> 1.5 aPTT> 60s) and Lu et al. [20] (INR> 1.3, aPTTr > 1.5), and the patients in our cohort were more severely burned.
Like Mitra et al. [7] and Sherren et al. [4] we found that coagulation alterations were more frequent in more severely burned patients, particularly alternations of the intrinsic coagulation pathway (aPTT), suggesting that more than a mere marker of coagulopathy this parameter could serve as a marker of severity, since both in this and other studies [4,7] it correlates with prognosis. In fact, patients with coagulation disorders required more blood products and presented a higher 28-day and 90-day mortality rate. Although the difference was only significant in 28-day mortality, we observed a clear trend that could have been significant if the n had been greater
In our study, most coagulation alterations were corrected within a week (median 4-5 days); only 13% patients required FFP, and this alteration was self-limiting in most cases. This clearly shows a discrepancy between the standard description of coagulopathy and the patient’s symptoms.
Viscoelastic tests have recently been introduced as a more comprehensive method of assessing coagulation disorders. In this and other studies [4,7], the coagulation alterations described by PT and aPTT laboratory tests would normally indicate the presence of coagulopathy and therefore a risk of haemorrhage. However, in some cases the results of viscoelastic tests [2] indicate hypercoagulability [12-15], so clinicians need to know how to interpret these data [21].
Park et al. [12] suggest that viscoelastic tests are a better indicator of hypercoagulability than standard tests such as those used in our study, and that in a study in burn and trauma cases, patients with prolonged PT and aPTT showed hypercoagulability
Schaden et al. [13] performed a study in which alterations in mean PT, aPTT and platelet count suggested the presence of burninduced coagulopathy and could have led to the administration of FFP and platelet concentrates; however, thromboelastometry performed in the same patients did not reach values that would indicate the need for haemostatic therapy.
Van Haren et al. [14] found mean thromboelastographic values within normal ranges on admission and signs of hypercoagulability 1 week later, while Wade et al. [15] found that subjects with burns or trauma at the time of admission, compared with controls, were hypercoagulable based on thromboelastography and calibrated automated thrombogram.
After a review of the foregoing findings and bearing in mind that this alteration was self-limiting many of our patients, we would not recommend administering clotting agents to correct these parameters unless there is active bleeding or risk of bleeding.
In our study, mortality was significantly higher (87.5%) in patients in whom PT and aPTT were not corrected, particularly among those in whom coagulopathy was not treated, probably due to their critical condition.
Patients in whom coagulopathy was not corrected all died within the first 28 days of admission, suggesting that persistent coagulopathy could be considered a factor of poor prognostic. Considering that coagulopathy resolves within a median of 4-5 days, this parameter could be an early indicator of poor prognosis in patients in whom it persists beyond this time.
Some of our patients underwent surgery despite persistent coagulation alterations. Some might find this surprising; nevertheless, in our study coagulation alteration was defined strictly in accordance with the laboratory’s normal ranges, but slight alterations are not necessarily a contraindication for surgery, particularly when the benefit outweighs the risk surgical delay.
In 2011, Forster et al. [18] suggested that the ABSI had become obsolete after more than 30 years in use, and although they concluded that it was still a valuable tool for assessing the severity and survival of burn patients, in our series mortality was lower than predicted in nearly all cases. This was probably due to progress made in the treatment of MBPs, and suggests this severity score may have to be re-evaluated.
Due to the complexity of the mechanisms involved in coagulation and inflammation in these patients, the high likelihood of glycocalyx degradation caused by large-volume fluid replacement [22-25] that promotes cell adhesion [23,26], and the potential need to administer various factors and cofactors, a comprehensive study of these factors is needed to clarify whether patients with severe burns are in a state of hyper or hypocoagulability, or even whether these alterations normalise 24 hours after thermal trauma. What is clear to us is that alterations in basic coagulation tests correlate with severity and prognosis, and that prognosis is worse in patients with persistent coagulopathy, bearing in mind that in most patients coagulopathy resolves in less than a week.
Limitations
According to the data at our disposal, our unit receives about 60 major burn patients per year; however, the hospital defines a major burn patient as having a TBSA ≥ 15% and ≥ 10% in children under 10 and over 65 years of age. Our inclusion criteria were stricter (18 years or older and TBSA ≥ 20%), and during the 6-year study period we were able to identify 187 potential patients, of which only 90 were finally included. The n of our study is one of our limitations since it prevented us from performing a multivariate analysis. In addition, it should be noted that ours is a retrospective chart review, and we therefore cannot guarantee the quality of the data.
Another limitation is the lack of other laboratory tests, such as thrombin, Clauss fibrinogen, viscoelastic tests or inflammation markers that would have allowed us to obtain more comprehensive data on ABIC and its different clinical implications; unfortunately, these tests were not requested at the time our study patients were treated, and are still not requested in many hospitals.
Data on the volume of fluids administered is also missing, so dilution coagulopathy could have affected our results. However, haemodilution due to aggressive fluid replacement in the first few hours following admission is often impossible to avoid in these patients, since stability takes precedence over possible haemodilution and the resulting coagulopathy.
Conclusion
The most severely burned patients are more likely to present alterations in standard coagulation tests, particularly those with ABSI ≥ 8 and TBSA ≥ 32%.
Coagulation abnormalities will affect the administration of blood products and mortality. Persistent coagulopathy can be considered a factor of poor prognosis.
Alteration of PT and aPTT does not necessarily indicate a patient with coagulopathy; this should be borne in mind when administering clotting agents.
Prospective studies are needed to provide a more comprehensive description of coagulation alterations in MBPs and the different contributing factors involved. This will give insight into how the different coagulation, anticoagulation and fibrinolysis mechanisms are compensated.
Acknowledgements
We thank the entire Burns team at the Vall d’Hebron University Hospital, but especially to Dr N. Martín, Dr L. Abarca, Dr J. Cirbian, Dr M. Iborra, Dr JM. Herreros and Dr J. Serracanta, who, though not listed as authors, are an active part of all the studies we perform in the unit.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Highlights
• 66.7% of large burned patients developed some sort of PT-aPTT abnormalities within first 24 hours
•• Patients with PT-aPTT prolonged times showed a significant increase in the consumption of RBC & FFP
•• PT-aPTT prolonged times do not necessary mean clinically significant bleeding diathesis
PT-aPTT alterations were associated with higher ABSI and significantly greater mortality.
References
- Guilabert P, Usúa G, Martín N, Abarca L, et al. (2016) Fluid resuscitation management in patients with burns: update. Br J Anaesth. 117(3): 284-296.
- Glas GJ, Levi M, Schultz MJ (2016) Coagulopathy and its management in patients with severe burns. J Thromb Haemost 14(5): 865-874.
- Sherren PB, Hussey J, Martin R, et al. (2014) Lethal triad in severe burns. Burns 40(8): 1492-1496.
- Sherren PB, Hussey J, Martin R, et al. (2013) Acute burn induced coagulopathy. Burns. 39(6): 1157-1161.
- Rae L, Fidler P, Gibran N (2016) The Physiologic Basis of Burn Shock and the Need for Aggressive Fluid Resuscitation. Crit Care Clin. 32(4): 491-505.
- King DR, Namias N, Andrews DM (2010) Coagulation abnormalities following thermal injury. Blood Coagul Fibrinolysis. 21(7): 666-669.
- Mitra B, Wasiak J, Cameron PA, et al. (2013) Early coagulopathy of major burns. Injury 44(1): 40-43.
- Lavrentieva A, Kontakiotis T, Bitzani M, et al. (2008) Early coagulation disorders after severe burn injury: impact on mortality. Intensive Care Med 34(4): 700-706.
- Barret JP, Dziewulski PG (2006) Complications of the hypercoagulable status in burn injury. Burns 32(8): 1005-1008.
- Barret JP, Gomez PA (2005) Disseminated intravascular coagulation: a rare entity in burn injury. Burns 31(3): 354-357.
- Geng K, Liu Y, Yang Y, et al. (2020) Incidence and Prognostic Value of Acute Coagulopathy After Extensive Severe Burns. J Burn Care Res 41(3): 544-549.
- Davenport R, Manson J, De’Ath H, et al. (2011) Functional definition and characterization of acute traumatic coagulopathy. Crit Care Med 39(12): 2652-2658.
- Hippensteel JA, Uchimido R, Tyler PD, et al. (2019) Intravenous fluid resuscitation is associated with septic endothelial glycocalyx degradation. Crit Care 23(1): 259.
- Lu RP, Ni A, Lin F-C, et al. (2013) Major burn injury is not associated with acute traumatic coagulopathy. J Trauma Acute Care Surg 74(6): 1474-1479.
- Lu RP, Ni A, Lin FC, et al. (2013) Major burn injury is not associated with acute traumatic coagulopathy. J Trauma Acute Care Surg 74(6): 1474-1479.
- Winearls J, Reade M, Miles H, et al. (2016) Targeted Coagulation Management in Severe Trauma: The Controversies and the Evidence. Anesth Analg 123(4): 910-924.
- Park MS, Martini WZ, Dubick MA, et al. (2009) Thromboelastography as a better indicator of hypercoagulable state after injury than prothrombin time or activated partial thromboplastin time. J Trauma - Inj Infect Crit Care 67(2): 266-275.






























