Anemia Management Clinic: A Cost-effective Patient Care Model
Sundara Reddy, MBBS., MBA1* and Usha Perepu, MBBS., MRCP2
1Department of Anesthesia, University of Iowa Healthcare, USA
2Department of Internal Medicine - Hematology, Oncology and Blood and Marrow Transplantation, University of Iowa Healthcare, USA
Submission: April 02, 2021; Published: February 28, 2022
*Corresponding author: Sundara Reddy, MBBS., MBA, Department of Anesthesia, University of Iowa Healthcare, 6 JCP, 200 Hawkins Dr, Iowa City, Iowa 52242, USA, Tel: +1 319-356-2108
How to cite this article: Sundara R, Usha P. Anemia Management Clinic: A Cost-effective Patient Care Model. J Anest & Inten care med. 2022; 11(5): 555824. DOI 10.19080/JAICM.2022.11.555824
Abstract
Introduction:Most patients presenting for major elective surgery with preoperative anemia can be managed without allogeneic transfusion. However, prompt access to an outpatient setting that can provide comprehensive anemia management while accommodating the time constraints of surgical scheduling is a major challenge.
Description:Therefore, to address this problem, we developed a novel anemia management clinic (AMC), which offers easy access and comprehensive anemia management services to patients scheduled for major elective surgery.
Discussion:We present our experience in implementation and subsequent expansion of this clinic into a high demand service attending to multiple disciplines, including surgical and medical specialties across our healthcare system.
Abbrevations:AMC: anemia management clinic, US: United States, APP: advanced practice provider, EBL: estimated blood loss, EMR: electronic medical records
Introduction
Preoperative management of modifiable risk factors such as anemia, frailty, malnutrition, diabetes, smoking, and chronic pain prior to major elective surgery remains sub-optimal at many healthcare institutions in the United States (US), resulting in poor patient outcomes and increased cost of care [1,2] A well-coordinated, interdisciplinary approach that is inexpensive, easy to access, has revenue generation potential, providing comprehensive optimization of all modifiable risk factors in one setting is the ideal solution for perioperative care. The optimal care delivery model for such a solution remains unclear [1,3]
Preoperative anemia is an independent predictor of poor perioperative outcomes [2,4-6] in addition to being strongly associated with blood transfusion [7,8]. Lack of timely screening for anemia and prompt access to an outpatient setting that can serve as a comprehensive solution for all aspects of anemia management are major limitations [8,9]. Surgeons in the US largely rely on primary care physicians or hematologists to manage preoperative anemias, who may not always be flexible enough to accommodate surgical schedules, which in turn interferes with prompt diagnosis and treatment of anemia prior to surgery.
Description
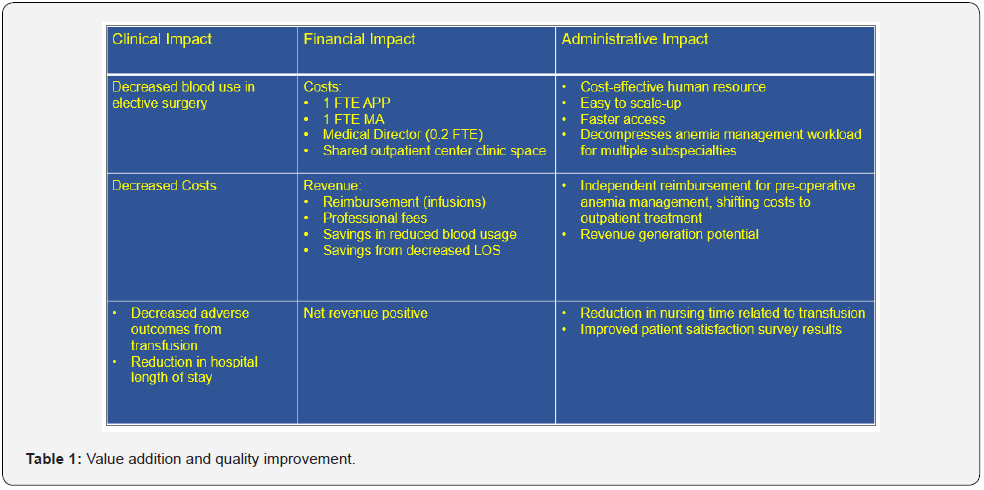
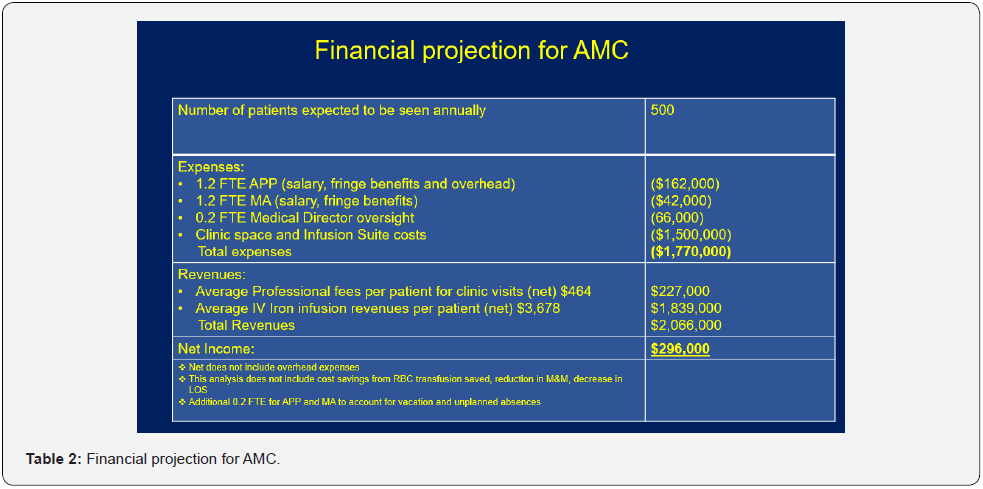
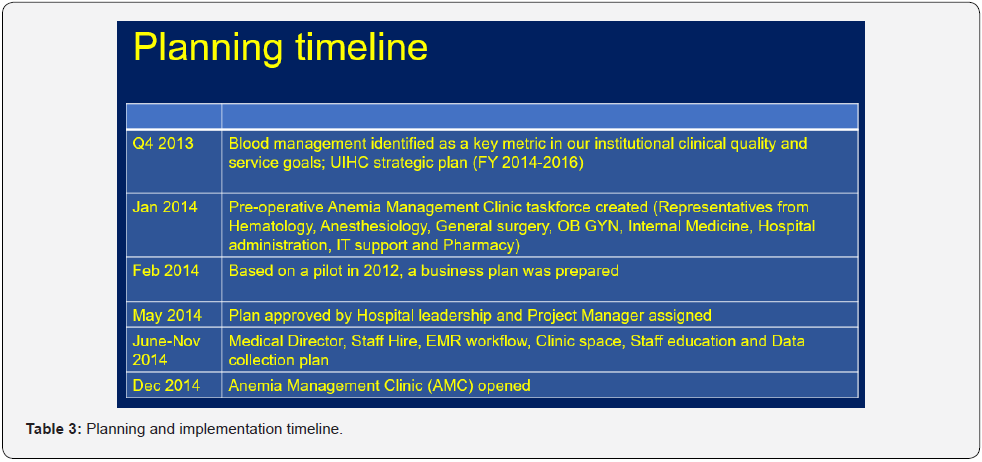
To ensure rapid and reliable access, we developed a novel clinic model staffed by an advanced practice provider (APP) to offer a comprehensive outpatient anemia management service at a large academic tertiary health care system, performing more than 30,000 surgeries annually. Planning and implementing the AMC occurred over a one-year period. Key aspects of added value and quality improvement in the business plan presented to hospital leadership are illustrated in Tables 1,2 and the timeline for planning and implementation is illustrated in Table 3.
The AMC opened in December 2014, initially targeting patients with anemia undergoing elective, high blood loss surgery defined as expected blood loss (EBL) > 500 mL. These included vascular, general, orthopedic, cardiothoracic, urologic, neurologic, and gynecologic surgeries. The target patients were screened by matching with a list of elective high blood loss procedures, which was generated for each surgical service by means of historical review of EBL data from the electronic medical record (EMR). The selected procedures were further vetted by surgeons from each service to ensure accuracy. If a high blood loss procedure is contemplated, surgeon proceeds to screen for anemia. Screening is done by using a hemoglobin value obtained within the last thirty days or by point of care hemoglobin testing on site. If the patient is anemic (Hb < 12 g/dL), a nurse can initiate a protocolbased order set in the EMR, enabling referral to AMC and blood sample collection for further testing (lavender top EDTA tube – CBC and light green top PST tube – for serum Ferritin, Iron panel, Creatinine, Vit B12, TSH etc.) [9]. The AMC provider then promptly triages the referral, assigns scheduling priority, orders additional lab tests from the pre-drawn PST sample, initiates insurance preauthorization if iron infusion or erythropoietin administration is anticipated and secures a provisional infusion slot. Same-day clinic appointments are offered during weekdays if possible and patients needing infusion therapy may choose to receive their treatment at our outpatient infusion suite, or in their own community, which AMC staff coordinate.
Our original model was a self-contained clinic with two monitored infusion chairs staffed by a part time APP (0.4 FTE), medical assistant (0.4 FTE), and a medical director (0.2 FTE) open two days per week. In addition to direct clinical care such as focused history and physical, formulate treatment plan, insert intravenous catheters, administer iron infusions, and monitor patients. The clinic staff also managed clerical tasks such as facilitate patient schedules, insurance pre-authorizations and field phone calls. With the high task load and staffing constraints, this model became unsustainable as the number of referrals increased. It became obvious that we needed to rethink our strategy to reduce clerical and some clinical task load specifically - infusion management to decompress the workload of our staff and grow the clinic to accommodate more consults. We readjusted our strategy to establish several important partnerships within our healthcare system to streamline our workflow and to enable sustained growth of the AMC. Examples include:
a. Partnership with outpatient infusion center within our healthcare system to outsource infusion management and allow AMC staff to focus solely on consults
b. Partnership with the hospital patient appointment center to manage all scheduling and insurance pre-authorizations
c. Partnership with pharmacy, resulting in addition of sterile hoods and staff to prevent delays in preparing iron infusions.
d. Partnership with IT services to implement data analytics software (TableauTM) to generate monthly reports for surgical providers showing their transfusion rates, referral trends to AMC and missed opportunity for pro-active anemia management resulting in peri-operative transfusion and increased length of stay.

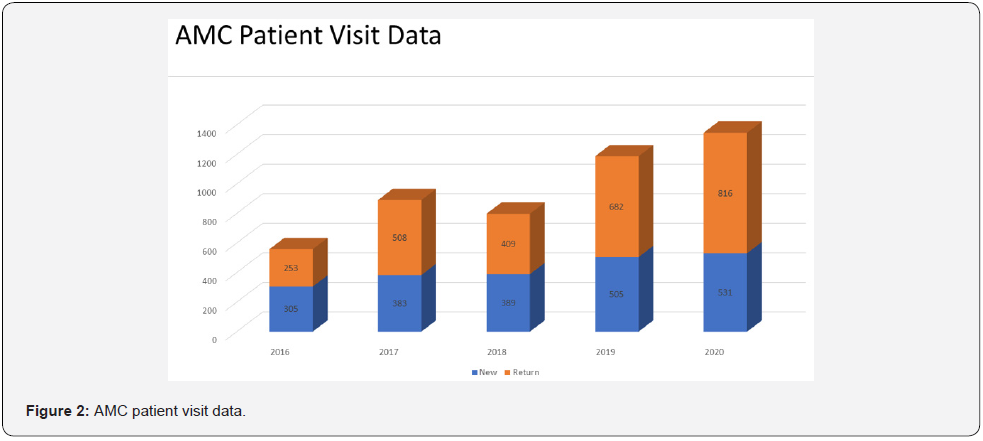
These changes, along with initiatives such as simplified EMR referral pathway, improved surgical provider awareness of the value of pre-operative anemia management through internal communication channels and patient education through information leaflets enabled us to increase our surgical patient volumes. In the five years since its founding, the AMC increased its scope of practice beyond perioperative care to several other service lines, including obstetrics gynecology, internal medicine, family medicine, gastroenterology, cardiology, and nephrology - Figure 1. Since implementation, AMC received over 5000 clinic visits, of which 40% were new consults and 60% were followup visits to assess response to treatment. The number of patient visits has increased steadily with a 30% increase in new consults and 65% increase in follow-ups over the last 2 years - Figure 2. In addition, the clinic has become a referral center for Jehovah’s Witnesses and others whose religious beliefs prohibit the acceptance of blood products.
Discussion
Anemia is prevalent in the general population [10,11] and specifically in certain populations such as perioperative [7,12- 14] and peripartum patients [15,16], in whom anemia needs to be addressed in a time-sensitive manner. Lack of easy access to a comprehensive anemia management service in the outpatient setting can be a major limitation, resulting in adverse patient outcomes [5,7,15].
A novel AMC staffed by an APP was created to address this limitation and improve quality of care in preoperative patients. The key supportive rationale for this model is:
a. Cost-effective human resource compared to the clinic being staffed by a full-time physician anesthesiologist
b. Easier to scale because of lower HR cost
c. Faster access for patients requiring basic anemia management
d. Consistent patient care guided by simple management algorithms derived through multidisciplinary consensus
e. Amenable to remote supervision by physician medical director
Majority of the referrals (85%) include anemias from nutritional deficiencies (40%), chronic blood loss (10%), chronic inflammation (25%) or a combination (25%). The remaining (15%) are hereditary or acquired hemolytic anemias and anemia from chronic kidney disease are routed back to hematology and nephrology services, respectively to establish specialist care.
The clinic quickly established itself as a useful resource for anemia management and gained acceptance across the institution. Based on rising demand for our service, we recognized early in our experience that there is a large, underserved need for basic anemia management in our community and the scope for the AMC extended well beyond managing preoperative anemias alone. The ability to scale created an opportunity to improve patient access, experience and population health in a cost-efficient manner across the institution- The triple aim of healthcare [17,18]. The AMC evolved as a service that could decompress basic anemia management workload for multiple subspecialties including obstetrics gynecology, hematology, nephrology, and gastroenterology. The increased patient numbers enabled the clinic to generate break even revenue from clinic visits alone to support staff expense (APP & MA- 1 FTE and Medical Director - 0.2 FTE). AMC also created new revenue streams for the healthcare system via infusions, pharmacy, and laboratory test charges in addition to cost savings generated by means of decreased blood transfusions and hospital length of stay (yet to be quantified accurately). As the number of referrals grew, we increased the clinic days from 2 to 4 per week. Our sole focus on clinic visits, without the distraction of clerical tasks and managing infusions, helped us implement a clinic scheduling template with 40-minute slots for new patients and 20-minutes for follow-up visits. This template enabled us to better define our clinic capacity, monitor capacity utilization and forecast future staffing needs.
We prioritize patients scheduled for surgery within 3 weeks for same or next day appointments by holding two new patient slots in the schedule twice weekly with a two-day release and by overbooking if needed while accommodating referrals from nonsurgical specialties to maximize our capacity utilization. We were fortunate to find a willing partner in our hospital’s infusion center which had excess capacity that was underutilized. We learned through experience that managing consults and infusions in a selfcontained setting is both resource intensive and makes patient throughput less predictable. We also learnt that more clinic consults will translate to more infusions and gave us leverage in building strategic partnerships with infusion center and pharmacy and the ability to negotiate dedicated resources such as infusion chairs and staff. With some modifications this model could be successfully replicated at other academic medical centers and community hospitals.
Authors Contribution
Dr. Sundara Reddy helped conceptualize and design the work; acquire, analyze, and interpret the data; draft and revise the manuscript; and gave final approval of the version to be published. Dr. Usha Perepu helped conceptualize the work, interpret the data, revise the manuscript, and gave final approval of the version to be published.
Disclosure
There is no HIPAA protected data disclosed in this manuscript.
References
- Cline KM, Clement V, Rock-Klotz J, Kash BA, Steel C, et al. (2020) Improving the cost, quality, and safety of perioperative care: A systematic review of the literature on implementation of the perioperative surgical home. J Clin Anesth 63: 109760.
- Fowler AJ, Ahmad T, Phull MK, Allard S, Gillies MA, et al. (2015) Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg 102(11): 1314-1324.
- Aronson S, Murray S, Martin G, Blitz J, Crittenden T, et al. (2020) Roadmap for Transforming Preoperative Assessment to Preoperative Optimization. Anesth Analg 130(4): 811-819.
- Gomez-Ramirez S, Jerico C, Munoz M (2019) Perioperative anemia: Prevalence, consequences and pathophysiology. Transfus Apher Sci 58(4): 369-374.
- Musallam KM, Tamim HM, Richards T, Spahn DR, Rosendaal FR, et al. (2011) Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet 378(9800): 1396-1407.
- Hare GMT, Mazer CD 2021() Anemia: Perioperative Risk and Treatment Opportunity. Anesthesiology 135(3): 520-530.
- Munoz M, Gomez-Ramirez S, Campos A, Ruiz J, Liumbruno GM (2015) Pre-operative anaemia: prevalence, consequences and approaches to management. Blood Transfus 13(3): 370-379.
- Munoz M, Laso-Morales MJ, Gomez-Ramirez S, Cadellas M, Nunez-Matas MJ, et al. (2017) Pre-operative haemoglobin levels and iron status in a large multicentre cohort of patients undergoing major elective surgery. Anaesthesia 72(7): 826-834.
- Okocha O, Dand H, Avram MJ, Sweitzer B (2020) An Effective and Efficient Testing Protocol for Diagnosing Iron-deficiency Anemia Preoperatively. Anesthesiology 133(1): 109-118.
- Petry N, Olofin I, Hurrell RF, Erick Boy E, Wirth JP, et al. (2016) The Proportion of Anemia Associated with Iron Deficiency in Low, Medium, and High Human Development Index Countries: A Systematic Analysis of National Surveys. Nutrients 8(11): 693.
- Kassebaum NJ, Collaborators GBDA (2016) The Global Burden of Anemia. Hematol Oncol Clin North Am 30(2): 247-308.
- Goodnough LT, Schrier SL (2014) Evaluation and management of anemia in the elderly. Am J Hematol 89(1): 88-96.
- Trentino KM, Mace HS, Symons K, Sanfilippo FM, Leahy MF, et al. (2021) Screening and treating pre-operative anaemia and suboptimal iron stores in elective colorectal surgery: a cost effectiveness analysis. Anaesthesia 76(3): 357-365.
- Richards T, Baikady RR, Clevenger B, Butcher A, Abeysiri S, et al. (2020) Preoperative intravenous iron to treat anaemia before major abdominal surgery (PREVENTT): a randomised, double-blind, controlled trial. Lancet 396(10259): 1353-1361.
- Beckert RH, Baer RJ, Anderson JG, Jelliffe-Pawlowski LL, Rogers EE (2019) Maternal anemia and pregnancy outcomes: a population-based study. J Perinatol 39(7): 911-919.
- Guinn NR, Cooter ML, Maisonave Y, Grimsley A, Cellura C, et al. (2020) How do I develop a process to effectively treat parturients with iron deficiency anemia? Transfusion 60(11): 2476-2481.
- Sinclair RC, Duffield KE, de Pennington JH (2020) Improving preoperative haemoglobin using a quality improvement approach to treat iron deficiency anaemia. BMJ Open Qual 9(1): e000776.
- Berwick DM, Nolan TW, Whittington J (2008) The triple aim: care, health, and cost. Health Aff (Millwood) 27(3): 759-769.






























