Post-Operative Analgesia: Are Patients Receiving Adequate Cover?
Mushosho Tendai1, Mpe Matela1, Masehla Benvolio1, Mkhwanazi Senzo1, Mokhothu Refilwe1, Molehe Relebogile1, Masilo Keorapetse1, Mshayisa Nkosinathi1, Mukoma Moloko1, Nokwe Yanga1, Ntjana Kgauhelo1, Ntshangase Ndumiso1, Phiri Cynthia1, Tambudze Katherine1 and Luvhengo Thifhelimbilu2*
1Faculty of Health Sciences, University of the Witwatersrand, Republic of South Africa
2Department of Surgery, Charlotte Maxeke Johannesburg Academic Hospital, Republic of South Africa
Submission: September 04 2021; Published: October 19, 2021
*Corresponding author: Luvhengo Thifhelimbilu, Department of Surgery, Area 397, Charlotte Maxeke Johannesburg Academic Hospital, P.O. Box 2694, Montana Park, Pretoria, 0159, Republic of South Africa, Tel: +27 83 995 2552
1. Mushosho Tendai - ORCID Number: https://orcid.org/0000-0002-8047-9263,
2. Mpe Matela - ORCID Number: https://orcid.org/0000-0795-757X
3. Masehla K, - Orcid Number: https://orcid.org/0000-0001-8156-0461.
4. Mkhwanazi Senzo - Orcid Number: https://orcid.org/0000-0001-8870-9708.
5. Mokhothu Refilwe - ORCID Number: https://orcid.org/0000-0002-9527-7306.
6. Molehe Relebogile - ORCID Number: https://orcid.org/0000-0001-7922-5373
7. Masilo Keorapetse - ORCID Number: https://orcid.org/0000-0001-9510-5961.
8. Mshayisa Nkosinathi - ORCID Number: https://orcid.org/0000-0001-9530-7029.
9. Mukoma Moloko - ORCID Number: https://orcid.org/0000-0003-1610-1079.
10. Nokwe Yanga - ORCID Number: https://orcid.org/0000-0002-2901-2895.
11. Ntjana Kgauhelo - ORCID Number: https://orcid.org/0000-0002-6940-1326.
12. Ntshangase Ndumiso - ORCID Number: https://orcid.org/0000-0002-5586-4477.
13. Phiri C - ORCID Number: https://orcid.org/0000-0002-1888-740X
14. Tambudze Katherine - ORCID Number: https://orcid.org/0003-0882-0954.
15. Luvhengo TE - ORCID Number: https://orcid.org/0000-0002-2901-1809.
How to cite this article: Mushosho T, Mpe M, Masehla B, Mkhwanazi S, Mokhothu R, et al. Post-Operative Analgesia: Are Patients Receiving 002 Adequate Cover?. J Anest & Inten care med. 2021; 11(4): 555816. DOI 10.19080/JAICM.2021.11.555816
Abstract
Introduction: Acute postoperative pain increases the risk of complications including chronic pain syndrome.
Aim: To determine if patients at the tertiary academic hospitals of University of the Witwatersrand are given adequate postoperative analgesia.
Method: A prospective cross-sectional observational study of patients who were post elective surgery was conducted. Participants included patients aged 18 to 60 years. Data collected included patients’ demographics, surgical procedures, type of anaesthesia, analgesic agent used and pain score. The Universal Pain Assessment Tool was used to obtain pain scores. Mean or median was used when appropriate to summarize data. The Student t-test and chi-square tests were utilized for comparison if suitable and a p-value below 0.05 was considered significant.
Results: 146 patients participated of which 40.4% and 33.6% were following general and orthopaedics procedures, respectively. General anaesthesia was used in 84.2% and 21 postoperative analgesic options were used of which 80.8% was as drug combination. An opioid was used in 46.6%. The mean pre-analgesic pain score was 6.45 ± 2.92. Pethidine was relied on for analgesia in 17.8%. 96.7% of females experienced postoperative pain before administration of analgesia compared to 93.0% in males. The mean post-analgesic pain score was 3.23 ± 2.62. Post-operative pain remained moderate or severe in 35.0% of females compared to 22.1% in males despite treatment. The difference was however not statistically significant (p-value= 0.09). Pain was either moderate or severe in 81.3% following general surgery as compared to 65.3% after orthopaedics procedures. In 12.3% of participants who had orthopaedics procedures pain was severe despite analgesics compared to 8.5% following general surgery operations.
Conclusion: Postoperative pain management is haphazard and does not appear to be based on guidelines. More than 70% of patients experience moderate to severe pain despite treatment with analgesics. Freedom from severe postoperative is less achieved in women.
Keywords:Postoperative pain, pain score, adequate, control
Introduction
Unlike accidental pain, postoperative pain is never beneficial to a patient because if it is not adequately eliminated it predisposes patients to complications including development of chronic pain syndrome [1,2]. Complications resulting from acute postoperative pain may lead to prolonged hospitalization and/or unplanned admission to a higher dependency unit resulting in the escalation of cost of health care. Adequate management of acute postoperative pain is a key component of strategies for enhanced recovery following surgery [1,3].
Currently multimodal management strategies are relied on to achieve a balanced analgesic effect in the perioperative period while limiting side effects of analgesic drugs, especially opioids [1,3-5]. Whenever it is feasible opioids should be avoided [6-10]. Selection of which analgesic drug(s) to use is influenced by amongst others the severity of pain, availability of pain management guidelines, preference by a clinician and drug availability [5,8,11]. It is recommended that management of acute postoperative pain should be by a multidisciplinary acute pain service (APS) team led by an anesthetist [12].
Several studies have shown that acute postoperative pain is universally not adequately managed and decision regarding what to use is usually left to a surgeon who performed the procedure [11- 14]. Consequently, a pain free state in the immediate postoperative period is rarely achieved and worrisomely in majority of situations around 70% of patients experience moderate to severe acute postoperative pain [1]. The aim of this study was to determine if patients at academic hospitals in University of the Witwatersrand circuit were being given adequate postoperative analgesia.
Method
A prospective observational study of consecutive patients who had elective surgical procedures at Chris Hani Baragwanath Academic Hospital (CHBAH) and Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) from 1st of May 2015 to 31st of August 2015 was conducted. Study population included patients aged 18 to 60 years who were able to give consent. Participants were enrolled between 24 to 48 hours following various surgical procedures: general surgery, orthopedics, otorhinolaryngology, ophthalmology, gynecology, maxillofacial, vascular and urology. Patients who had caesarian section were excluded.
Consent was sought from each patient before data collection. Data were collected by members of the group and included patients’ demographics and type of operation, analgesia, and anesthesia.
The Universal Pain Assessment Tool (UPAT) (http://www. anes.uncla.edu/unclapainmanagment ratingscales.php) was used to rate severity of acute postoperative pain before and after analgesia. The UPAT was preferred because it was considered easier for patients to understand and would not be markedly influenced by the level of education. Collection sheet was given to each patient to complete but in cases where this was not possible, participants were assisted by the investigators. Each patient was asked to rate his or her acute postoperative pain before and after administration of analgesic(s).
Permission to conduct the study was obtained from the Human Research Committee of University of the Witwatersrand (M150431) and Research Review Boards of Charlotte Maxeke Johannesburg Academic Hospital and Chris Hani Baragwanath Academic Hospital. Participation in the study was on a voluntary basis and anonymity was assured. The study was conducted according to guidelines contained in the World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects adopted in 1964 and amended in 2013.
Data was entered into an excel spreadsheet. The obtained pain perception scores were divided into four categories: Category A= pain free (Score: 0), Category B=mild pain (Score: 1-4), Category C = moderate pain (Score: 5-6) and Category D = severe pain (Score: 7-10). Pain scores before and after administration of analgesic(s) were analyzed according to gender, age, hospital and surgical procedures. Mean with standard deviation or median and interquartile range (IQR) was used for continuous data. Categorical data were expressed in percentage. The student t-test was used to compare continuous data and Chi-square test for categorical data. Level of significance was set at a p-value below 0.05.
Results
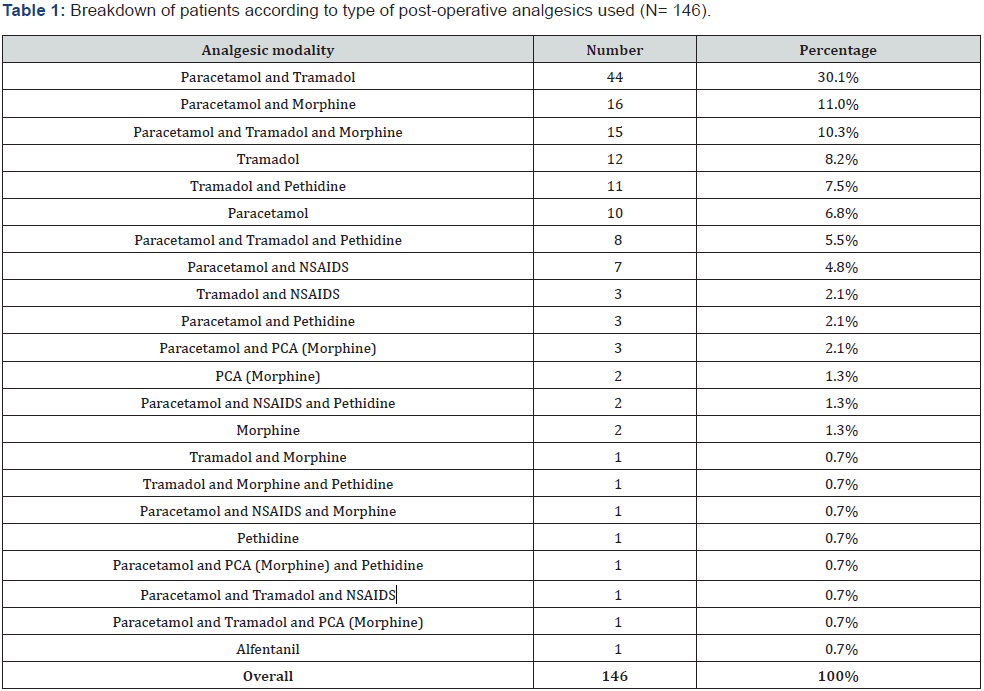
A total of 146 patients participated and an overwhelming majority of participants were classified as blacks and 86/146 (58.9%) of whom were males. Their average age was 38.5 years (range: 18-60). The bulk of study participants were following general surgery (40.4%) and orthopedics (33.6%) procedures. Majority 123/146 (84.2%) of the operations were performed under general anaesthesia. Participants were interviewed 33.2 ± 8.75 hours (range: 20-48 hours) (95th confidence interval of 33.2 ± 8.75: ± 4.28%) after they had had surgical procedures. The mean pain score as reported by participants before administration of analgesics 6.45 ± 2.92 (95th confidence interval of 6.44 ± 0.47: ± 7.36%). A total of 21 postoperative analgesic options were used but a combination of paracetamol and tramadol was preferred in 44/146 (30.1%) as shown in Table 1.
A combination of analgesic drugs was used in 118/146 (80.8%) of patients and in 68/146 (46.6%) an opioid was used either alone or in combination with other analgesic drug(s). Pethidine was utilized in 26/146 (17.8%). Relationship between severity of postoperative pain and analgesic choice is shown in Table 2 and Table 3.
The mean pain score reported following administration of analgesics was 3.23 ± 2.62 (95th confidence interval of 3.43 ± 0.43: 13.18%). A complete pain free state, meaning Category A was achieved in 27/146 (18.5%) whereas 19/146 (13.0%) still had severe pain after administration of analgesic(s) (Figure 1).
PCA= Patient Controlled Analgesia
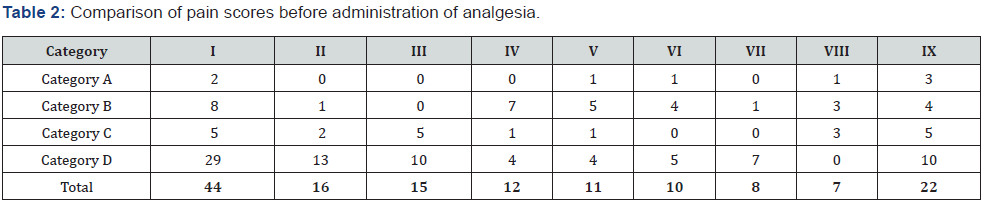
I= Paracetamol +Tramadol, II= Paracetamol +Morphine, III= Paracetamol + Tramadol + Morphine IV= Tramadol, V= Tramadol + Pethidine, VI= Paracetamol, VII= Paracetamol + Tramadol + Pethidine, VIII= Paracetamol + NSAIDS, IX= All others combined.
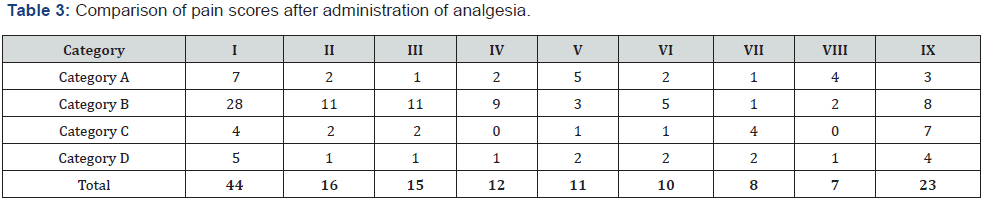
I= Paracetamol +Tramadol, II= Paracetamol +Morphine, III= Paracetamol + Tramadol + Morphine IV= Tramadol, V= Tramadol + Pethidine, VI= Paracetamol, VII= Paracetamol + Tramadol + Pethidine, VIII= Paracetamol + NSAIDS, IX= All others combined.
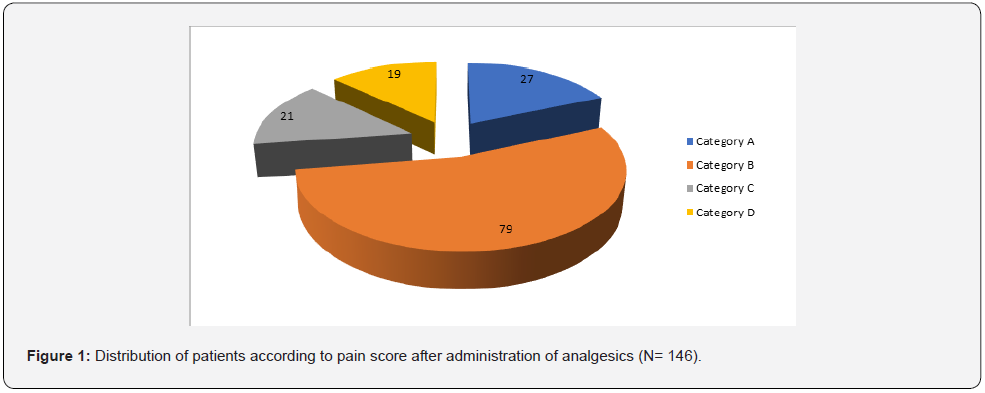
Category A = Pain free, Category B= Mild pain, Category C= Moderate pain, Category D= Severe
Close to 96.7% (58/60) of female patients suffered acute postoperative pain before analgesics were administered compared to 93.0% (80/86) in males. 16.7% (10/60) of females still had severe acute postoperative pain even after administration of analgesic(s) as compared to 10.5% (9/86) in males. Postoperative pain remained moderate or severe in 35.0% (21/60) of females compared to 22.1% (19/86) in males after administration of analgesic drugs. The difference was however not statistically significant with a p-value of 0.09 (Table 4).
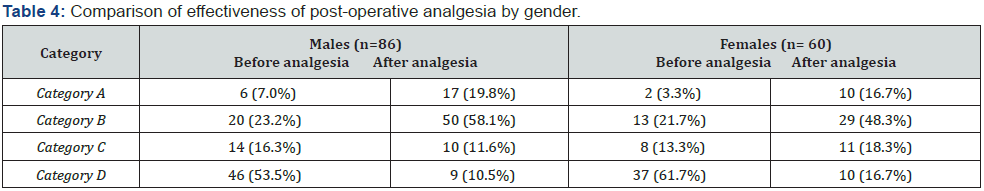
Category A = Pain free, Category B= Mild pain, Category C= Moderate pain, Category D= Severe.
Around 98.4% (61/62) of patients at CHBAH experienced postoperative pain which was either moderate or severe in 80.7% (50/62). Comparatively, 91.7% (77/84) of patients never had freedom from postoperative pain and the pain was moderate or severe in 65.5% (55/84). Only 6.5% (4/62) patients at CHBAH still had severe pain post analgesic use contrasted to 17.8% (15/84) at CMJAH (Table 5).
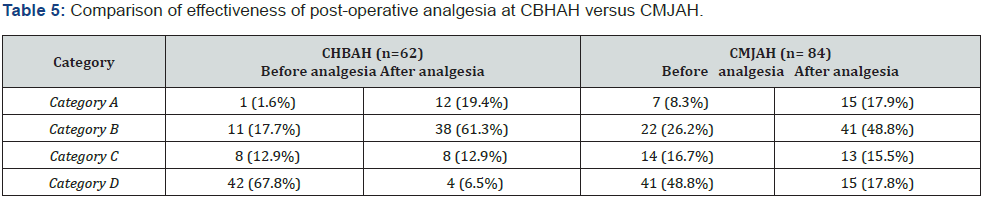
Category A = Pain free, Category B= Mild pain, Category C= Moderate pain, Category D= Severe.
Following general surgery and orthopedics procedures; 96.6% (57/59) and 93.9% (46/49), respectively experienced postoperative pain. The pain was either moderate or severe in 81.3% (48/59) following general surgery as compared to 65.3% (32/49) after orthopedics surgery. In close to 12.3% (6/49) of participants who had orthopedics procedures the pain was severe despite analgesics use as opposed 8.5% (5/59) following general surgery operations (Table 6).
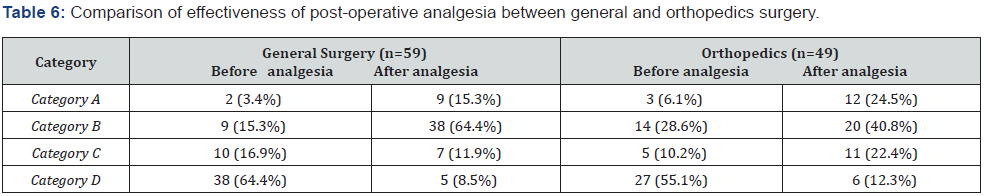
Category A = Pain free, Category B= Mild pain, Category C= Moderate pain, Category D= Severe.
Discussion
Perception of acute postoperative pain is influenced by various factors which include the magnitude of surgical trauma, the site of operation, pre-morbid state, age, gender, activity level, culture, and psychological state [1,8]. The above factors also influence how patients respond to treatment modalities including analgesics. Unfortunately, pain perception and the magnitude of benefit which would be derived from a particular analgesic modality are not predictable [1]. Management of acute postoperative pain control is an essential component of postoperative care. Achievement of a pain-free postoperative state has remained elusive despite the existence of numerous guidelines, discovery of new drugs and implementation of innovative treatment strategies [12].d tramadol was preferred in 44/146 (30.1%) as shown in Table 1.
Current recommendation regarding management of postoperative pain is to start pre-operatively and to rely on multimodal strategies including counselling [1,3,15-18]. Ideally, post-operative pain management should be by a dedicated acute pain management team led by a perioperative care physician anesthetist [12,19,20]. The choice of which analgesic modality to use is often driven by individual bias and institutional or national guidelines. However, in certain instances existing institutional, national, or international guidelines are guidelines are not followed. The use of more than 20 postoperative analgesic options in this study did not seem to be influenced by type or magnitude of surgical procedures, and prescription of analgesics appear not to have been following available guidelines for management of acute post-operative pain [21,22].
Another disturbing finding is that opioids were relied on for postoperative analgesia in close to 50% of the study population. In certain cases in the current study opioids were solely relied on for management of acute postoperative pain. Reliance on opioids for treatment of acute postoperative pain is against recommendations contained in the enhanced recovery after surgery (ERAS) program [1,3,18]. Limited use of opioids especially intravenously would be possible if multimodal strategies are utilized [1,23].
A more worrying finding from the study is the continued use of pethidine, even as a sole agent; despite universal condemnation and a call for it to be banned. Reasons why pethidine is not preferred for management of acute postoperative pain it is associated with enumerable side effects. Some of the side effects of pethidine and other opioids include respiratory depression,delirium, ileus, immune suppression, pruritus, serotonin syndrome and dependency [1,24-26]. It was however not possible to establish in the current study if in patients for whom pethidine was used, it was part of drug combination, top up for persistent pain or breakthrough pain or was prescribed ab initio [23,27].
Neither of the hospitals would pass a test to become a “Pain Free Hospital” [28]. At both hospitals more than 70% of patients experienced moderate to severe acute postoperative pain. A pain free state was achieved in less than 25% of patients at both hospitals regardless of gender and type of procedure. However, women and patients following orthopedics procedures experienced comparatively more severe pain. Close to 35% of women and patients following orthopedics operations still had significant pain (moderate to severe) despite administration of analgesics.
Finding of heightened acute postoperative pain perception and relatively poor response to post-analgesia in women compared to men is consistent with report from prior studies [29- 33]. Possible reasons for gender difference include prevalence of painful episodes in females and a different hormonal milieu [29,30]. Similarly, acute post-operative pain is reported to be less readily achieved in patients following orthopedics procedures as compared to general surgery operations [1,32]. Gender differences, the type of surgical procedures, availability of guidelines for management of acute pain and psychological issues are just some of the issues which explain why a pain-free state in the immediate postoperative periods remains elusive [8,34-38].
Limitation of the Study
Pain is complex regarding both how it is perceived and its assessment. The Universal Pain Assessment Score was chosen for its simplicity and may not have been the appropriate method as it has not been tested in our setting. Background pre-operative pain, prior analgesic use, concomitant use of other drugs and substances, pre-operative counselling, implementation of multimodal nonpharmacological strategies and different activity level of patients could have influenced pain perception and therefore response to analgesia, but were not factored in. Notwithstanding, the goal of any method used to treat acute postoperative pain should be to obtain a complete pain free state for all patients around the clock following any surgical procedure.
Conclusion
Postoperative pain management at the two hospitals is haphazard and does not appear to be based on available acute postoperative pain management guidelines. More than 70% of patients still experience moderate to severe pain despite treatment.
Recommendation
Follow up studies should look at the prevalence of postoperative complications and chronic pain syndrome in our setting. Management of acute postoperative pain should be prioritized and be on based national or international guidelines.
Funding:
The study was self-funded.
Acknowledgement
We sincerely appreciate all the criticism and contributions made by our GEMP 2 Classmates and Undergraduate Research Committee of University of the Witwatersrand both during protocol development and when we presented our work at the Undergraduate Research Day.
Declaration
All authors have no conflict of interest to declare. The research was done as part of promotional requirement for 5th Year Medical Students (MBBch 5) of University of the Witwatersrand. Abstract of the study was presented at Pre-graduate Research Day of Faculty of Health Sciences of University of the Witwatersrand in 2015 and 44th Annual Meeting of the Surgical Research Society of Southern Africa in Cape Town in 2016.
Ethics
The study was conducted following guidelines of the revised Declaration of Helsinki (2013). Only patients who could give a written informed consent were included. Permission to conduct the study was received from the Human Ethics Committee of University of the Witwatersrand and Research Review Boards of Chris Hani Baragwanath Academic Hospital and Charlotte Maxeke Johannesburg Academic Hospital.
Authorship and Contributions
1. Mushosho T: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
2. Mpe M: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
3. Masehla K: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
4. Mkhwanazi S: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
5. Mokhothu R: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
6. Molehe R: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
7. Motiang K: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
8. Mshayisa N: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
9. Mukoma M: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
10. Nokwe Y: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
11. Ntjana K: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
12. Ntshangase N: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
13. Phiri C: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
14. Tambudze K: Literature search, writing of research proposal, application for Ethics approval, data collection, data analysis and review of manuscript.
15. Luvhengo TE: Conception of idea, supervision of writing of research proposal, supervision of application for Ethics and Research Review Board approvals, supervision of data collection and analysis, drafting and review of manuscript, preparation of manuscript for submission and corresponding author.
References
- Hyland SJ, Brockhaus KK, Vincent WR, Spence NZ, Lucki MM, et al. (2021) Perioperative Pain Management and Opioids Stewardship: A Practical Guide. Healthcare 9(3): 333.
- Katz J, Weinrib A, Fashler SR, Katznelzon R, Shah BR, et al. (2015) The Toronto General Hospital Transitional Pain Service: development and implementation of a multidisciplinary program to prevent chronic postsurgical pain. J Pain Res 8: 695-702.
- Kehlet H, J B Dahl (1993) The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg 77(5): 1048-1056.
- Alam A, Rampes S, Patel S, Hana Z, Ma D (2021) Anesthetics or anesthetic techniques and cancer surgical outcomes: a possible link. Korean J Anesthesiol 74(3): 191-203.
- Johnson AP, Mahaffey R, Egan R, Twagirumugabe T, Parlow JL (2015) Perspectives, perceptions and experiences in postoperative pain management in developing countries: a focus group study conducted in Rwanda. Pain Res Manag 20(5): 255-260.
- Chia PA, Cannesson M, Myo Bui CC (2020) Opioid free anesthesia: feasible. Curr Opin Anaesthesiol 33(4): 512-517.
- Adjei MR, Letsa TS, Mahama E, Owusu-Agyei S (2015) The effect of opioids on field block for hernia repair: a study comparing pethidine with a placebo. S Afr J Surg 53(4): 1-4.
- Afolayan JA, Oyeleye DI, Adebiyi FO, Durojaiye AO, Bitrus D (2015) Factors influencing perception of pain among clients attending a Nigeria teaching hospital. Int J Nurs Midwifer 7(7): 133-140.
- Aziato L, Dedey F, Marfo K, Asamani JA, Clegg-Lamptey JNA (2015) Validation of three pain scales among adult postoperative patients in Ghana. BMC Nursing 14: 42.
- Lam KKY, Mui WLM (2016) Multimodal analgesia model to achieve low postoperative opioid requirement following bariatric surgery. Hong Kong Med J 22(5): 428-434.
- Masigati HG, Chilonga KS (2014) Postoperative pain management outcomes among adults treated at a tertiary hospital in Moshi, Tanzania. Tanzan J Health Res 16(1): 47-53.
- Meissner W, Coluzzi F, Fletcher D, Huygen F, Morlion B, et al. (2015) Improving the management of post-operative acute pain: priorities for change. Curr Med Res Opin 31(11): 2131-2143.
- Morin C, Patel Y, Javid M, Trevis SE, Fortes T, et al. (2021) Opioid-Sparing Multimodal Analgesia Protocol for Lumpectomy Patients Results in Superior Postoperative Pain Control. Ann Surg Oncol 28(11):5855-5864.
- Venkateswaran R, Prasad KN (2006) Management of postoperative pain. Indian J Anaesth 50(5): 345-354.
- Vadivelu N, Mitra S, Schermer E, Kodumudi V, Kaye AD, et al. (2014) Preventive analgesia for postoperative pain control: a broader concept. Local Reg Anesth 7: 17-22.
- Dong W, An B, Wang Y, Cui X, Gan J (2021) Effect of multimodal analgesia on gynecological cancer patients after radical resection. Am J Transl Res 13(4): 2686-2693.
- Gelman D, Gelmanas A, Urbanaite D, Tamosiunas R, Sadauskas S, et al. (2018) Role of Multimodal Analgesia in the Evolving Enhanced Recovery after Surgery Pathways. Medicina 54(2): 20.
- Gan TJ (2017) Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 10: 2287-2298.
- White PF, Kehlet H, Neal JM, Schricker T, Carr DB (2007) The role of the anesthesiologist in fast-track surgery: from multimodal analgesia to perioperative medical care. Anesth Analg 104(6): 1380-1396.
- Haller G, Agoritsas T, Luthy C, Piquet V, Griesser AC, et al. (2011) Collaborative quality improvement to manage pain in acute care hospitals. Pain Medicine 12(1): 138-147.
- Apfelbaum JI, Ashburn MA, Connis RT, Gan TJ, Nickinnovich DG, et al. (2012) Practice guidelines for acute pain management in the perioperative setting. An updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 116(2): 248-273.
- South African Acute Pain Guidelines (2009) SAJAA 15(6): 1-120.
- Koh W, Nguyen KP, Jahr JS (2015) Intravenous non-opioid analgesia for peri- and postoperative pain management: a scientific review of intravenous acetaminophen and ibuprofen. Korean J Anesthesiol 68(1): 3-12.
- MacPherson RD, Duguid M (2008) Strategy to eliminate pethidine use in hospitals. Journal of Pharmacy Practice and Research 38(2): 88-89.
- Neuman MD, Bateman BT, Wunsch (2019) Inappropriate opioid prescription after surgery. Lancet 393(10180): 1547-1557.
- Scotton WJ, Hill LJ, Williams AC, Barnes NM (2019) Serotonin Syndrome: Pathophysiology, Clinical Features, Management, and Potential Future Directions. Int J Tryptophan Res 12: 1178646919873925.
- De Roo AC, Vu JV, Regenbogen SE (2020) Statewise Utilization of Multimodal Analgesia and Length of Stay After Colectomy. J Surg Res 247: 264-270.
- Eldor J, Kotlovker V, Orkin D (2013) Pain free hospital – availability (24 hours) of anesthesiologists. Journal of Anesthesiology & Clinical Science 2013. Doi:10.7243/2049-9752-2-17.
- Greenspan JD, Craft RM, LeResche L, Arendt-Nielsen L, Berkley KJ, et al. (2007) Studying sex and gender differences in pain and analgesia: a consensus report. Pain 132(Suppl 1): S26-S45.
- Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL (2009) Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain 10(5): 447-485.
- Rokyta R, Yamamotova A (2013) Sex differences in pain perception and interpretation. Activitas Nervosa Superior Rediviva 55(3): 125-134.
- Ekstein MP, Weinbroum AA (2011) Immediate postoperative pain in orthopaedic patients is more intense and requires more analgesia than in post-laparotomy wounds. Pain Med 12(2): 308-313.
- Zheng H, Schnabel A, Yahiaoui-Doktor M, Meissner W, Van Aken H, et al. (2017) Age and preoperative pain are major confounders for sex differences in postoperative pain outcome: A prospective database analysis. PLoS One 12(6): e0178659.
- Gan TJ (2017) Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 10: 2287-2298.
- Eshete MT, Baeumler PI, Siebeck M, Tesfaye M, Haileamlak A, et al. (2019) Quality of postoperative pain management in Ethiopia: A prospective longitudinal study. PLoS One 14(5): e0215563.
- Yang MMH, Hartley RL, Leung AA, Ronksley PE, Jette N, et al. (2019) Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis. BMJ Open 9(4): e025091.
- Mimic A, Bantel C, Jovicic J, Mimic B, Kisic-Tepavcevic D, et al. (2018) Psychological factors as predictors of early postoperative pain after open nephrectomy. J Pain Res 11: 955-966.
- Luo J, Min S (2017) Postoperative pain management in the postanesthesia care unit: an update. J Pain Res 10: 2687-2698.






























