Pain Management After Elective Shoulder Surgery: A Randomized Quantitative Study Comparing Hydromorphone With Piritramide
Boesmueller S1, Gerstorfer I1, Steiner M1, Prossinger H2*, Fialka C1 and Steltzer H1, 3
1AUVA Meidling, Austria
2Department for Evolutionary Anthropology, University of Vienna, Austria
3Sigmund Freud University, Austria
Submission: September 25, 2019; Published: October 11, 2019
*Corresponding author: Hermann Prossinger, Department for Evolutionary Anthropology, Faculty of Life Sciences, University of Vienna, Vienna, Austria
How to cite this article: Boesmueller S, Gerstorfer I, Steiner M, Prossinger H, Fialka C, Steltzer H. Pain Management After Elective Shoulder Surgery: A Randomized Quantitative Study Comparing Hydromorphone With Piritramide. J Anest & Inten Care Med. 2019; 9(4): 555768. DOI: 10.19080/JAICM.2019.09.555768. DOI: 10.19080/JAICM.2019.09.555768
Abstract
Background: Postoperative pain management plays an important role in elective shoulder surgery. Several methods have been investigated so far. The aim of this randomized quantitative study is to compare two frequently used postoperative pain regimes (hydromorphone versus piritramide) regarding onset and duration after the effectiveness of the single-shot interscalene block has diminished.
Methods: All patients who underwent elective shoulder surgery at our institution agreed to participate in this study. Upon admission patients were assigned membership to group A (hydromorphone) or group B (piritramide) according to the patient number (which ensured randomization). Pain assessment was performed using the numeric rating scale (NRS). For statistical analyses the techniques of maximum likelihood (ML) estimation were used.
Results: Of the 48 patients aged 18–89 years included in this study, 25 were in group A and 23 in group B. Of these 48, 21 in each group registered pain levels above threshold at least once. Shoulder surgery was performed 45 times in an arthroscopic and 3 times in an open technique. Occurrence of highest pain levels was less likely for patients receiving hydromorphone.
Conclusion: The analgesic activity of the two drugs significantly differs. Both opioids were found to be effective for pain treatment after elective shoulder surgery, although with a different pharmacokinetic. Piritramide acted faster, whereas hydromorphone acted over a longer duration-the latter similar to sustained-delivery medication
Keywords: Hydromorphone Piritramide Elective shoulder surgery Pain management Mixture distribution Maximum likelihood Beta distribution
Introduction
Elective shoulder surgery is common in orthopedic and trauma departments and postoperative pain management is crucial in order to achieve a high rate of patient satisfaction. Patients, upon being asked about their concerns regarding their planned hospitalization, most frequently voice their fear of postoperative pain. Consequently, preoperative clarification (by the medical team) and agreement (by the patient) to option choices of postoperative pain management is of paramount importance. There is general consensus that the postoperative pain after elective shoulder surgery can be depressed for up to 12 hours by administering a single-shot interscalene brachial plexus block [1,2]. However, after the effect of the block wears off, patients are in need of some form of further pain management. A study investigating pain levels after day-case shoulder surgery reported that analgesia at home is often inadequate after the interscalene block wears off [3]. As a consequence, several techniques, among them nerve blocks, sub-acromial infusions or cryotherapy, have been investigated [4,5]. All these are accompanied by a wide range of complications such as infection, block failure, catheter leakage or pneumothorax [6-8]. Some oral medications like gabapentin and nonsteroidal anti-inflammatory drugs are occasionally accompanied by adverse side effects like somnolence, peptic ulcer disease, platelet dysfunction, renal impairment, and delayed tendon-to-bone healing [9-11]. Although arthroscopic techniques in shoulder surgery offer the possibility of allowing patients to be released on the day of surgery, this is not standard procedure atour institution. Patients are hospitalized at least one night, as it is well documented that the first 24 hours after shoulder surgery are the most painful [12]. We use the following postoperative pain regimens most frequently: either hydromorphone (administered orally) or piritramide (applied subcutaneously). The aim of this study is to compare these two regimens regarding onset and duration of postoperative pain relief. We show that suitable logistics and treatment with baseline medication is efficient; and, more importantly, perhaps, how well pain can be managed in this way. To wit: this randomized study compares hydromorphone with piritramide in the postoperative pain management regimen after elective shoulder surgery.
Material and Methods
Ethics requirements
In the pre-anesthesia outpatient clinic, patients were asked if they wanted to participate in this study. Those who agreed signed an informed consent. First, a preliminary evaluation of chronic pain was performed, then detailed instructions how to use the numeric rating scale (NRS) were supplied. In this study, no patients refused to participate. The study was conducted in strict adherence to a protocol approved by the local ethics committee (Ethics Board Approval Number UKH/2012-77), as well as the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
Patients
A total of 48 patients (33 males and 15 females) with an age range 18–89 years (the re-normalized ages are Betadistributed) underwent elective shoulder surgery at our Trauma Center and were included in this study. All surgeries were performed by the same surgeon who is specialized in shoulder surgery. One anesthetist performed all anesthesia and a different one the postoperative pain management. Upon admission, patients were allocated to the two groups according to their patient number: those with an even number were allocated to the hydromorphone group (group A), while the other ones were allocated to the piritramide group (group B) for postoperative pain treatment. Because patient numbers are assigned upon acceptance to the hospital, irrespective of their treatment, this ensures adequate randomization. Inclusion criteria were as follows: patients (a) undergoing elective shoulder surgery with a single-shot interscalene plexus brachialis block in addition to general anesthesia,
(b) aged 18–99 years, and
(c) being capable of giving an informed consent to participation in this studyExclusion criteria were: patients
(a) aged below 18 years,
(b) with decompensated liver, heart or renal insufficiency,
(c) with any kind of lung disease
(d) with a chronic pain syndrome, or
(e) with a previous pain medication with more than three drugs over more than three months. All patients transferred to another hospital as well as patients who refused informed consent were excluded from this study.
Clinical methods
Before surgery, no patient was administered any premedication. An ultrasound-guided single-shot interscalene brachial plexus block with 20ml ropivacain 7.5% combined with 1vial (2ml) of dexamethasone was administered. During surgery, patients received total intravenous anesthesia consisting of an induction dose with propofol (10mg/kg) and a maintenance dose of 6mg/kg. Pain treatment was performed using fentanyl adapted to body mass (2-20μg/kg). After surgery, patients were transferred to a recovery room. There, the effects of the interscalene block on peripheral motor function, sensitivity and circulation were documented. Also documented were: NRS, side effects of general anesthesia (such as postoperative nausea and vomiting), any neurological complications and any other pain medication, if administered. After two hours in the recovery room, patients were transferred to the ward, where pain assessment according to NRS was elicited and vitality parameters were recorded. In addition, a second evaluation of the interscalene block regarding motor function, sensitivity and blood circulation took place. Patients were asked to communicate their pain level on a point scale (0- 10; 0.5-point resolution) to the hospital staff every 6hours (at midnight, 6am, noon, and 6pm) for four days (from noon of Day 0 to midnight of Day 3-resulting in 15 entries). Occasionally, patients did not communicate pain levels, either because they felt no pain or they were asleep. We set such pain level entries to 0 (i.e. missing for these analyses). Patients did not communicate pain levels in the morning of Day 0 (time of operation).
Statistical methods
Analysis of possible male/female differences in physical parameters We used maximum likelihood (ML) estimation (a) to find the ML distribution and (b) used Wilks Λ [13,14] to find the probability that the female sample and the male sample have been drawn from the same population (with, per definition, the same distribution). Further details about ML are elaborated in the Appendix. A careful analysis of the populations of the physical parameters from which the samples are drawn is necessary, so as to avoid possible confounding factors, if indeed the male/female and/or hydromorphone/piritramide populations are statistically different. As we show below, the populations are significantly homogeneous with respect to sex. We do not categorize patients by gender, because the admission office did not query prospective patients as to their gender identity; only their (biological) sex was entered in the admission record. Analysis of registered pain levels We selected all registered pain levels above a threshold (pain level NRS >1.5). Because the pain levels are bounded from belowby 0 and above by 10, we rescaled pain levels to the interval 0-1 and estimated the ML distribution for the pain levels, including the possibility that the distribution is a mixture distribution. As shown below, the by far most likely distribution of pain levels above threshold for each group is a mixture distribution-a sum of two Beta distributions. In each group, we determined the transition pain level; i.e. the pain level at which the likelihoods of each of the Beta distributions are equal. The log-likelihood of the ML mixture distribution of all pain levels combined was also calculated. We used Wilks Λ [13] (proportional to the logarithm of the likelihood ratios) to determine the probability that the sample of pain levels treated with hydromorphone were drawn from the same distribution as the sample of pain levels treated with piritramide. Analysis of pain levels by time slot We used the transition pain level found with the mixture distributions for pain levels of patients receiving hydromorphone and those receiving piritramide to determine when patients registered pain levels higher than the transition pain level.
Results
Parameters (range, ML value, ±34.1%CI, 𝔼) of age, mass, height and BMI of male and female patients are shown in Table 2. In 31 patients the right side and in 17 patients the left side was affected. Shoulder surgery was performed 45 times in an arthroscopic and 3 times in an open technique. Five patients had undergone previous shoulder surgery on the affected side: one proximal humeral fracture that had been previously plated and converted into a reverse total shoulder arthroplasty, two arthroscopic bankart repairs with consecutive shoulder stiffness that underwent arthroscopic arthrolysis, one previous supraspinatus tendon repair undergoing subscapularis repair and synovectomy, and one failed rotator cuff repair that was treated with arthroscopic superior capsular repair. Using the American Society of Anesthesiologists (ASA) categories, patients were grouped as follows: ASA1 16 patients, ASA2 25 patients, and ASA3 7 patients (Table 1).
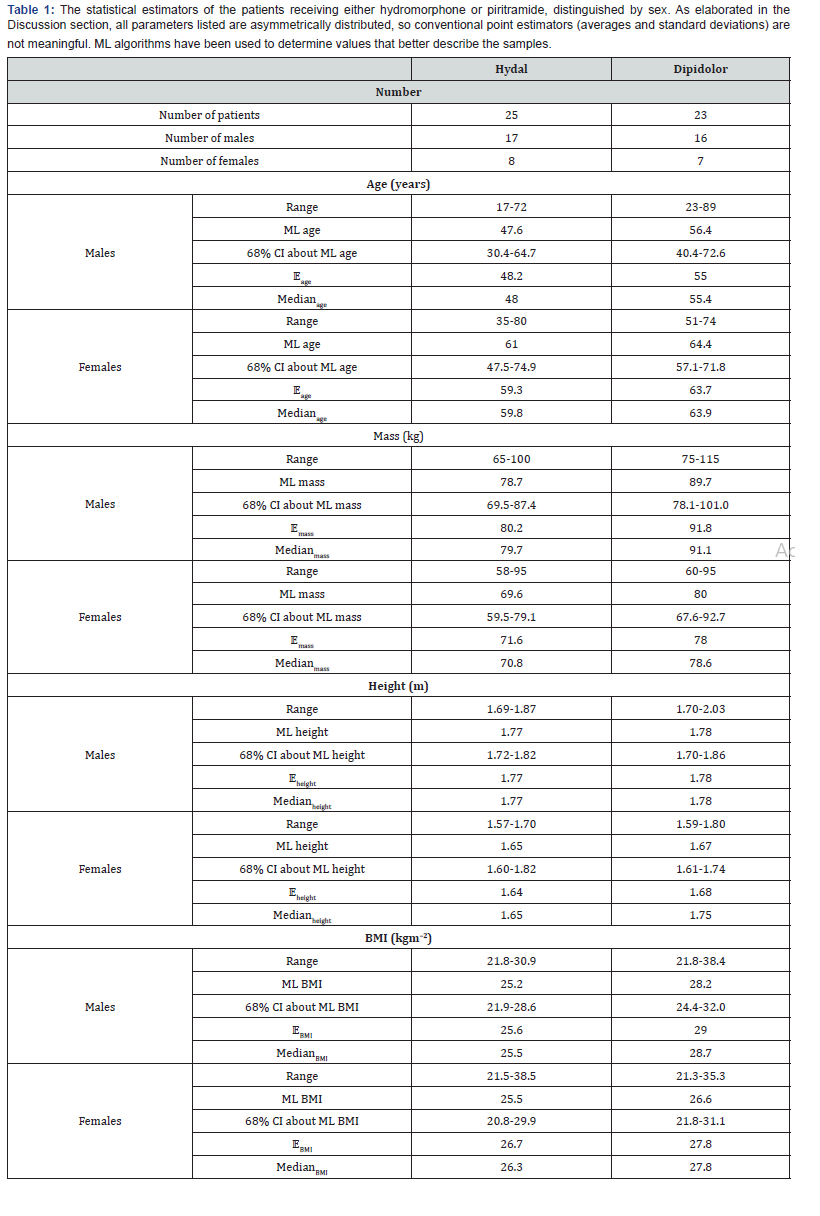
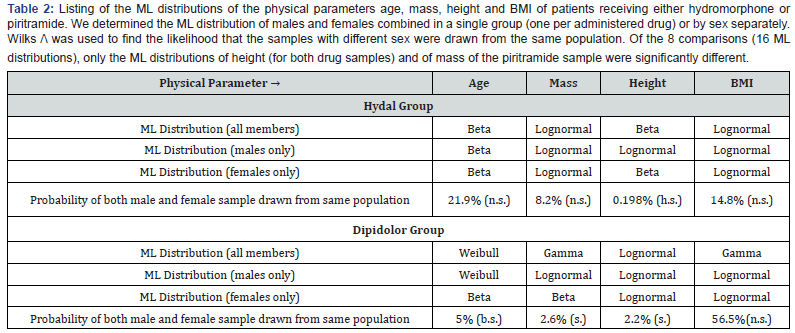
Comparisons of patient groups
The results of using Wilks’ Λ [14] to determine the probability that male and female samples were drawn from the same distribution show that only the heights for both groups of patients and the mass of the piritramide patients have been drawn from different populations (at 5 % significance level). Mass and BMI of hydromorphone patients and height of piritramide patients are log-normally distributed in all three cases (males and females combined, males separately and females separately). All other physical parameters have several ML distributions. Table 2 shows that, in effect, both groups are homogeneous with respect to sexual differences, except for height. We conclude, therefore, that we need not differentiate the effectiveness of the administered drugs by sex (given this sample size-further elaborations are in the Discussion section).
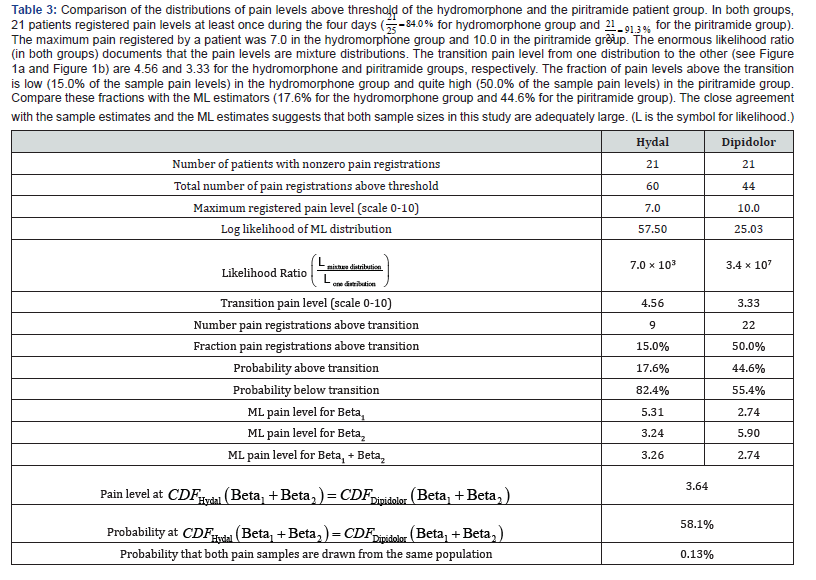
Distributions of registered pain levels
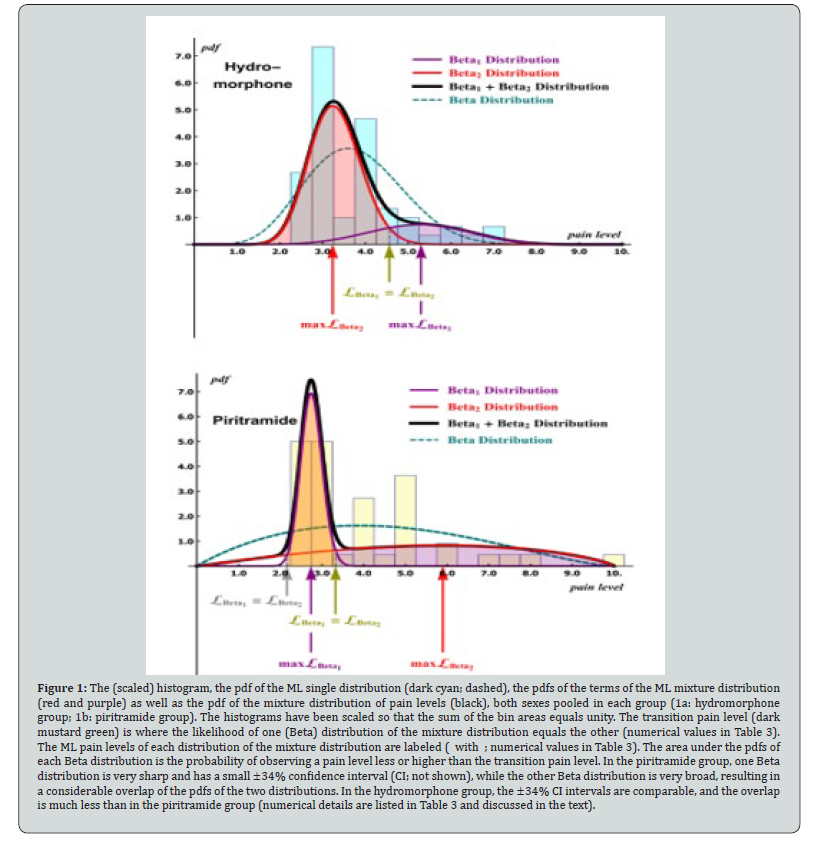
The transition pain level, where the likelihood of the Beta1 distribution equals the likelihood of the Beta2 distribution is 4.56 for the hydromorphone group and 3.33 for the piritramide group (Table 3). We observed that the distribution with ML pain levels below transition is much sharper (implying hardly any spread in pain level registrations) in the piritramide group than in the hydromorphone group. Figure 1 shows the ML distribution of pain levels above threshold for the hydromorphone group and the piritramide group. In both, the ML distribution is a mixture distribution; each is a sum of two Beta distributions. The likelihood ratios (70 thousand and 34 million for the hydromorphone and the piritramide groups, respectively; Table 3) emphasize the need to use ML analyses (rather than compare sample averages, say). In both groups, we observed that the assumption of one single (as opposed to a mixture) distribution is unsupportable. Hence, estimating the expectation value 𝔼 by calculating the sample average would lead to fallacious conclusions.
Pain levels and analgesic effect
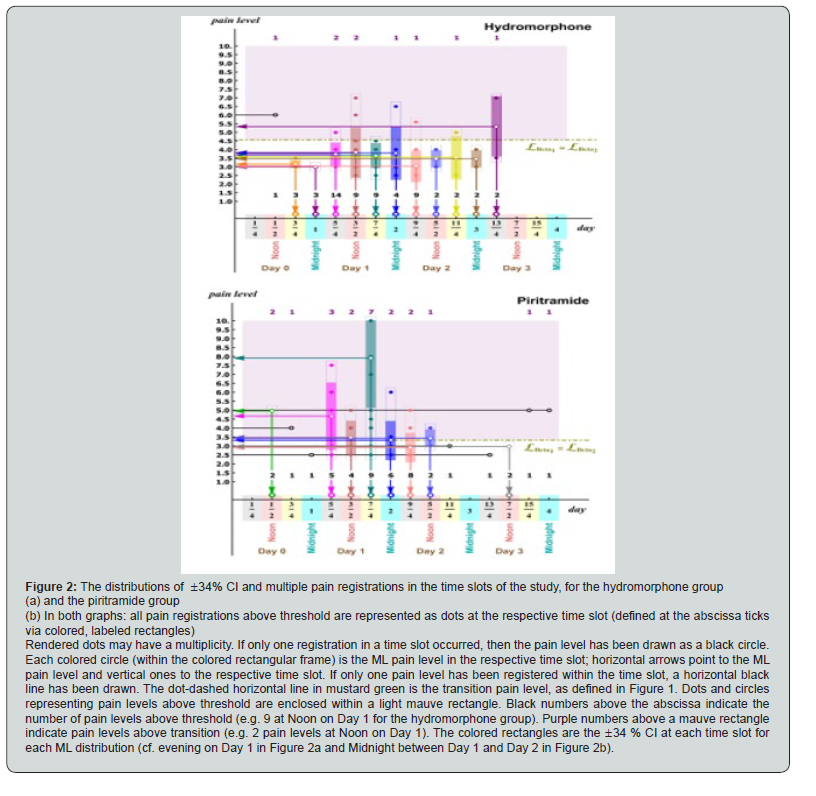
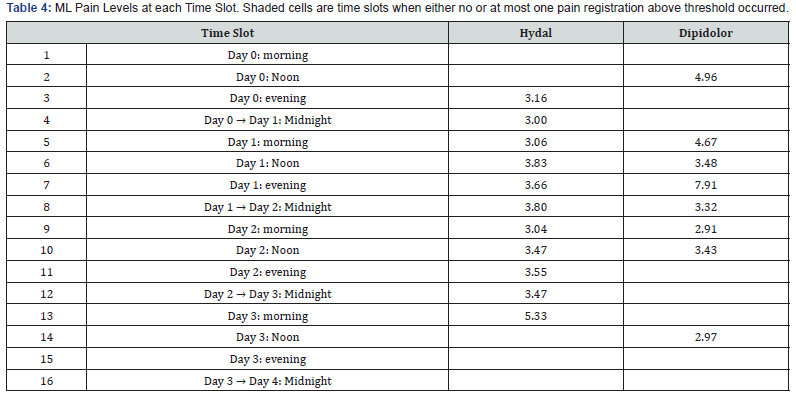
Hydromorphone group (group A; Figure 2a): very few pain registrations are above transition (nine only; 15.0 %; Table 3) and only once is there one single pain registration (at Noon on Day 0). The ML pain levels cluster in the interval 3.0–4.0; only one ML pain level and one single pain registration are above transition. There are no pain registrations above threshold at time slots 14- 16 indicating that patients receiving hydromorphone registered no pain after Noon on Day 3.

Piritramide group (group B; Figure 2b): 50 % of pain levels are above threshold (22; Table 3). Single pain registrations above threshold occurred six times: at time slots 3, 4, 11, 13, 15, and 16 (and two of these at time slots 3, 15 and 16 were above transition). There is no clustering of ML pain levels; five are above threshold. Multiple pain registrations above threshold cluster in the time slots 5–10 and a further clustering at time slot 14 (Noon on Day 3, where the ML is slightly below transition). Only in time slot 12 (Midnight between Day 2 and Day 3) did no patient receiving piritramide register a pain level above threshold. Twice, at time slots 2 and 13 (Noon on Day 0 and Day 3) were registered pain levels above threshold equal (namely: two at pain level 5.0 and 3.0 respectively). The probability that the pain levels of the hydromorphone group and the piritramide group have been drawn from the same population is 0.13% inferring that the pain levels above threshold registered by the patients in the two groups are significantly differently distributed and therefore the analgesic activity of the two drugs significantly differs. A very large fraction of pain levels registered by the piritramide group spikes at less than 3.0, but there is a considerably ‘fat’ tail beyond pain level 3.5 (Figure 3). The pdf-curve for the pain levels of the hydromorphone group is much broader about the maximum (around pain level 3.3), but the tail decreases to zero much more rapidly. For the value shown as an example in the graph in Figure 3 (ξcut), the probability of having registered pain levels less than this value is 58.9 % for the piritramide group and 78.5 % for the hydromorphone group. This implies that it is much less probable that higher pain levels will be registered by the hydromorphone patients.
Complications and adverse effects
We observed no complications attributable to the single-shot interscalene block. No patients had any side effects such as nausea or vomiting, constipation, somnolence, sedation, or vertigo after application of either hydromorphone or piritramide (Figure 4).

Discussion
To our knowledge, this is the first evaluation in a clinical setting that compares the effect of hydromorphone with that of piritramide as a postoperative analgesic in elective shoulder surgery while independent of the surgical intervention performed. Orthopedic surgery is known to be considerably more painful than other interventions due to the mobilization of soft tissue and tendons [15,16]. As measured by opioid consumptionshoulder surgery has, arguably, the highest pain levels in upper extremity surgery [17] and the rate of re-admission because of persistent postoperative pain is high [18]. Patient satisfaction after any surgical intervention is to a large extent dependent on postoperative pain treatment. There exist several clinical studies investigating different pain management medications and techniques after shoulder surgery [4,5]. We took advantage of the fact that we do not routinely perform shoulder surgery as an outpatient procedure in our institution; we could therefore conduct a randomized quantitative study comparing two postoperative pain treatment regimens. The literature ascribes opioids a tremendously bad reputation: not only because of the well-known risk of their potential dependency but also because of other adverse effects [17]. Moreover, whenever drugs are prescribed without asking the patient for his/her pain levels and prospective needs, the considerable amount of leftover pain medication offers the risk for abuse [17,19]. We suspect that orthopedic surgeons contribute to over-prescription in order to avoid re-admission because of the risk of persistent pain [19,20]. In an evaluation of opioid use after upper extremity surgical procedures [17], the average intake duration was 3.1 days, which is consistent with our study results (as pain levels reached a value below threshold within 3 days in both groups). Patients in this study received opioids only while under observation during their stay, with a baseline medication twice a day and a possible further demand medication whenever pain exceeded NRS 5.0. We have already pointed out that patients need an effective postoperative pain treatment as long as pain triggers are acute. After this phase, opioids should be withdrawn as soon as possible in order to not only prevent any abuse [21] but also to decrease the risk of addiction. Patients in this study were released from hospital without availability of opioid medication but with provisions for conventional analgesics, when needed.
We found that pain levels above threshold are drawn from populations with mixture distributions as the most likely distributions. As shown in Figure 1a and 1b, there are two modes and therefore estimating 𝔼 using the data set averages to perform comparisons would be fallacious. We found that there is no unique distribution for the random variables age, mass, height and BMI, neither for males nor for females, nor for patient group (hydromorphone or piritramide). The probability that males and females are drawn from different populations is very rarely small (only in 3 of the 8 cases), so we may assume that, with respect to sex, patients in each group are adequately homogeneous. All analyses presented here are based on this inference of homogeneity. We have tested whether the populations of pain levels above threshold could be a sum of three distributions. The likelihood in the case of three distributions is somewhat higher than for two distributions, but the increase in the number of degrees of freedom from 5 (one amplitude, two parameters per Beta distribution) to 8 indicates that, via AICc (Akaike’s Information Criterion [22], corrected for finite sample size [23]) we would then be including statistical noise in our model. Painlevels above threshold occur over a longer time period when patients use piritramide, and the range of pain levels is also larger. However, in the case of piritramide, one Beta distribution of the pain levels infers that it is more likely that pain levels experienced are lower than those experienced by the other group at these low pain levels. Higher pain levels (distributed by the second Beta distribution) are experienced with a higher probability for the piritramide group. We do not propose a rigorous mathematical model that can explain why the registered pain levels are the superposition of two Beta distributions. We do, however, observe that in the hydromorphone group, the two Beta distributions have much less overlap (Figure 1). In both the hydromorphone and the piritramide groups, one Beta distribution is peaked with a small ±34% CI about the mode. This seems to indicate that it is improbable for patients (of either group) to register very high pain levels (‘excruciating’ pain). This phenomenon infers that patients did not register (and therefore, presumably, experience) very high pain levels if hydromorphone had been administered. Conversely, however, hydromorphone patients did experience slightly higher ML pain levels (4.26 for hydromorphone versus 3.33 for piritramide). Perhaps hydromorphone does not suppress reasonable (yet nonetheless painful) pain levels as strongly as does piritramide, but manages to prevent excruciating pain from occurring with as high a probability as does piritramide [30].
The results of statistical analysis presented in Figure 2 infer a further difference between the effects of hydromorphone versus those of piritramide. The ML values in the hydromorphone group cluster in the pain level interval 3.0-4.0, and there is no clustering along the time axis since the operation from evening of Day 1 until shortly after the end of Day 2 (roughly 60 hours). The registered pain levels (and the ML values) of the piritramide group, on the other hand, are much more scattered: the clustering occurs for only five ML values (as opposed to ten for the hydromorphone group) and most ML values are clustered in time: from 6 am of Day 0 to Noon of Day 2 (roughly 36 hours). Time estimates cannot be rigorously obtained, however, because of the large (6-hour) time intervals between registrations. If a patient were to register every six hours (and none did), then the time resolution would be 1/15 (7%); compare this with the pain level resolution 0.5/10 (5%). Although both resolutions may seem comparable, we observed that there are many more pain level registrations over the pain level interval 2.0-10.0 than over the time interval 0.125-4.125. A further clustering observation: in hydromorphone group, many pain levels were registered in many time slots, up to fourteen at 6 am on Day 1; thus many ML values could be calculated; in the piritramide group, the pain levels were close to uniformly spread (with nine registrations in one single time slot- 6pm on Day 1-being by far the highest). This would infer that pain levels do not ‘disappear’ as quickly in the piritramide group; there are no pain registrations (0 %) below NRS 1.5 in time slots 14-16 in the hydromorphone group, while there are ‘still’ 4 (11 %) in the piritramide group (Figure 2b and Table 4).
Conclusion
Despite some limitations (rather but not very small sample size; surgical interventions with varying pain levels; numerical pain level assessments communicated by patients being highly subjective), we were able to show that both opioids are effective for pain treatment after elective shoulder surgery. Differences were seen in pharmacokinetics, because piritramide acted faster with, subsequently, a more rapid decrease and hydromorphone acted more slowly but with a more extended release. Precautions regarding the prescription of oral opioids are a prerequisite. As is to be expected for pain levels being so non-normally distributed, both in time and over the population(s) of pain levels, no simple verdict (of the kind: “One of the analgesics is superior to the other.”) can be presented. The presence of mixture distributions cautions against any other study finding such a simple verdict. The time series analysis showed that piritramide acted faster, whereas hydromorphone had a longer duration of effectiveness similar to sustained-delivery medication.
References
- Singelyn FJ, Lhotel L, Fabre B (2004) Pain relief after arthroscopic shoulder surgery: a comparison of intra-articular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg 99(2): 589-592.
- Trompeter A, Camilleri G, Narang K, Hauf W, Venn R (2010) Analgesia requirements after interscalene block for shoulder arthroscopy: the 5 days following surgery. Arch Orthop Trauma Surg 130(3): 417-421.
- Wilson AT, Nicholson E, Burton L, Wild C (2004) Analgesia for day-case shoulder surgery. Br J Anaesth 92(3): 414-415.
- Uquillas CA, Capogna BM, Rossy WH, Mahure SA, Rokito AS (2006) Postoperative pain control after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 25(7): 1204-1213.
- Warrender W, Syed UAM, Sommer H, Emper W, Ciccotti MG, et al. (2017) Pain management after outpatient shoulder arthroscopy. Am J Sports Med 45(7): 1676-1686.
- Borgeat A, Ekatodramis G, Kalberer F, Benz C (2001) Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology 95(4): 875-880.
- Webb D, Guttmann D, Cawley P, Lubowitz JH (2007) Continuous infusion of a local anesthetic versus interscalene block for postoperative pain control after arthroscopic shoulder surgery. Arthroscopy 23(9): 1006-1011.
- Yamaguchi K, Sethi N, Bauer GS (2002) Postoperative pain control following arthroscopic release of adhesive capsulitis: a short-term retrospective review study of the use of an intra-articular pain catheter. Arthroscopy 18(4): 359-365.
- Bang SR, Yu SK, Kim TH (2010) Can gabapentin help reduce postoperative pain in arthroscopic rotator cuff repair? A prospective, randomized, double-blind study. Arthroscopy 26(9): 106-111.
- Souter AJ, Fredman B, White PF (1994) Controversies in the perioperative use of nonsterodial antiinflammatory drugs. Anesth Analg 79(6): 1178-1190.
- Virchenko O, Skoglund B, Aspenberg P (2004) Parecoxib impairs early tendon repair but improves later remodeling. Am J Sports Med 32(7): 1743-1747.
- Ganapathy S, Amendola A, Lichfield R, Fowler PJ, Ling E (2000) Elastomeric pumps for ambulatory patient controlled regional analgesia. Can J Anaesth 47(9): 897-902.
- Wilks S (1938) The large-sample distribution of the likelihood ratio for testing composite hypotheses. Ann Math Stat 9(1938): 60-62.
- Prossinger H, Bookstein FL (2003) Statistical estimators of frontal sinus cross section ontogeny from very noisy data. J Morphol 257(1): 1-8.
- Chung F, Ritchie E, Su J (1997) Postoperative pain in ambulatory surgery. Anesth Analg 85(4): 808-816.
- McGrath B, Elgendy H, Chung F, Kamming D, Curti B, et al. (2004) Thirty percent of patients have moderate to severe pain 24 hr after ambulatory surgery: a survey of 5,703 patients. Can J Anaesth 51(9): 886-891.
- Kim N, Matzon JL, Abboudi J, Jones C, Kirkpatrick W, et al. (2016) A Prospective Evaluation of Opioid Utilization After Upper-Extremity Surgical Procedures: Identifying Consumption Patterns and Determining Prescribing Guidelines. J Bone Joint Surg Am 98(20): e89.
- Coley KC, Williams BA, DaPos SV, Chen C, Smith R (2002) Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. J Clin Anesth 14(5): 349-353.
- Rodgers J, Cunningham K, Fitzgerald K, Finnerty E (2012) Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am 37(4): 645-650.
- White PF, Kehlet H (2010) Improving postoperative pain management: what are the unresolved issues? Anesthesiology 112(1): 220-225.
- Akaike H (1973) Information theory as an extension of the maximum likelihood principle. 199-213.
- Takeuchi K (1976) Distribution of informational statistics and a criterion for model fitting. Suri Kagaku 153: 12-18.
- Bishop CM (2006) Pattern Recognition and Machine Learning. Springer Science.
- Burnham KP, Anderson DR (2002) Model Selection and Multimodel Inference: A Practical Information-Theoretic Approach. 2nd Edn Springer.
- MacKay DJC (2003) Information Theory, Inference, and Learning Algorithms.
- Crawley MJ (2007) The R Book. John Wiley & Sons.
- Huelsenbeck JP, Crandall KA (1997) Phylogeny estimation and hypothesis testing using maximum likelihood. Ann Rev Ecosys 28: 437-466.
- Stiglitz Y, Gosselin O, Sedaghatian J, Sirveaux F, Molé D (2011) Pain after shoulder arthroscopy: A prospective study on 231 cases. Orthop Traumatol Surg Res 97(3): 260-266.
- Amrhein V, Greenland S, McShane B (2019) Retire statistical significance. Nature 567: 305-307.
- Prossinger H, Hetz H, Acimovic A, Berger R, Mostafa K, et al. (2019) Can Conventional Randomization in Clinical Trials with Small Sample Sizes Be Considered Adequately Random? A Case Study of TBI Patients Sedated with Sevoflurane or Propofol. International Journal of Science, Environment and Technology 8(4): 938-954.






























