The Effect of Magnesium Sulphate Pre-Treatment on Rocuronium Priming in Achieving Rapid Onset of Intubating Conditions
Nirmal Sheshagiri*, Khalid Zahir, Lokesh Reddy, Salman Mohammad Kutty, Surjya Kanta Mohanty and Supriya Preman
Department of Anesthesia and Critical Care, Narayana Hrudayalaya Institute of Medical Sciences, India
Submission: March 03, 2018; Published: April1 20, 2018
*Corresponding author: Nirmal Sheshagiri, Department of Anesthesia & Critical Care, Mazumdar Shaw Medical Center, Narayana Hrudayalaya Institute of Medical Sciences, Bommasandra Industrial Area, Bangalore-560099, Karnataka, India, Tel: 0091998634670, 00918023514422; Email: nirmalsheshagiri@gmail.com
How to cite this article: Nirmal S, Khalid Z, Lokesh R, Salman M K, Surjya K M,et.al. The Effect of Magnesium Sulphate Pre-Treatment on Rocuronium Priming in Achieving Rapid Onset of Intubating Conditions. J Anest & Inten Care Med. 2018; 6(4): 555693. DOI: 10.19080/JAICM.2018.06.555693
Abstract
Aims: We investigated whether the onset of neuromuscular blockade was shortened by a combination of Magnesium pre-treatment and Rocuronium priming, compared with Rocuronium priming used alone.
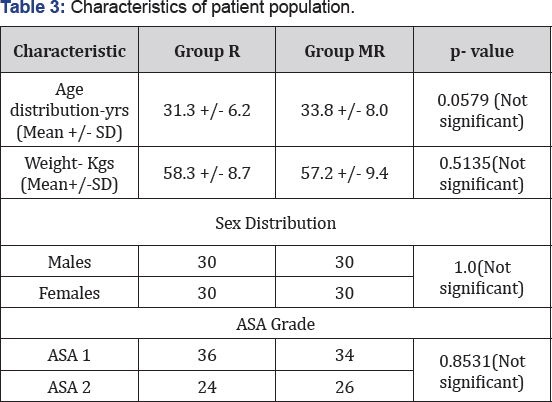
Settings and Design: The study was designed as a prospective randomised double blind controlled study.
Methods and Material: A hundred and twenty patients who were scheduled to undergo elective surgical procedures under general anaesthesia were randomized into Group R(n=60)wherein they were given 0.06mg/kg of Rocuronium (priming dose) three minutes before a further dose of 0.54mg/kg (intubating dose) of Rocuronium and Group MR (n=60) wherein they were given an infusion of 50 mg/kg Magnesium sulphate ten minutes before the administration of the priming dose and subsequently the intubating dose of Rocuronium. In both the groups, the train-of-four (TOF) responses to stimuli of the facial nerve at the corrugator superciliary muscle were measured at intervals of 12 seconds. Trachea was intubated when the TOF stimulus showed loss of the last twitch (T1). The time to onset of neuromuscular blockade was the primary outcome. Time to intubation and tracheal intubating conditions were also measured.
Statistical analysis used: Student's 't' test was used to test the significance of difference between quantitative variables and Fisher's chi square test for qualitative variables
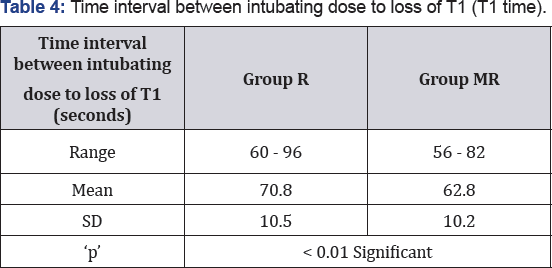
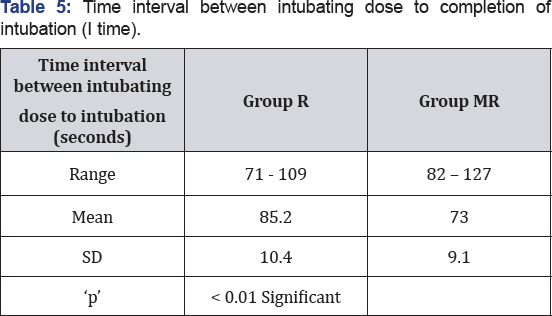
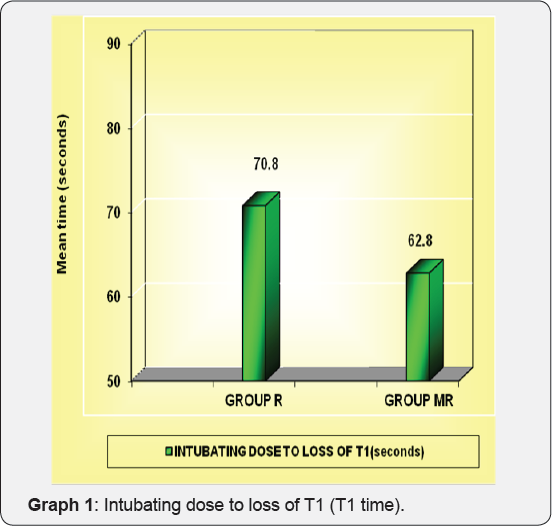
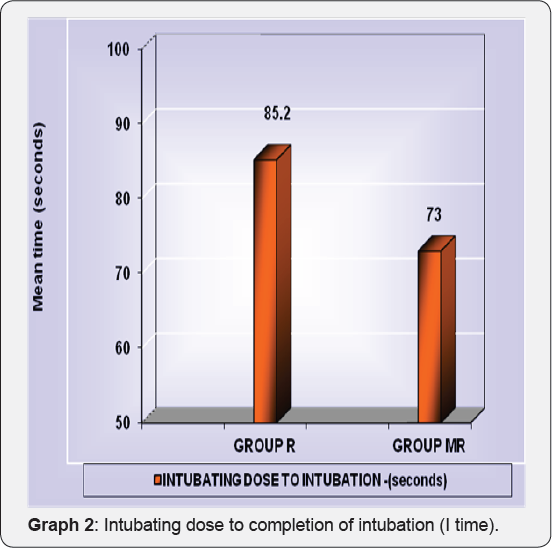
Results: The Magnesium and Rocuronium Priming group (group MR) had a significantly shorter onset time in Mean±SD of 62.8±10.20 sec when compared to the onset time in Mean±SD (seconds) in Rocuronium Priming group (group R), which was 70.80±10.50. (p < 0.01).This resulted in a significantly earlier completion of intubation as the mean time to intubation in Group "R” was 85.2 +/- 10.4 seconds and in group "MR” was 73.0 +/- 9.1 seconds. (P < 0.01).
Conclusions: The combination of Magnesium sulphate pretreatment and Rocuronium priming accelerated the onset of neuromuscular blockade, improved rapid-sequence intubating conditions and resulted in earlier endotracheal intubation when compared with Rocuronium priming used alone.
Keywords: Rocuronium priming; Magnesium sulphate; Train of four; Neuromuscular blockade; Corrugator superciliary
Introduction
Emergency intubations are not a rarity in anaesthesia, emergency medicine and critical care practice. Intubation is performed as fast as possible to avoid complications due to hypoxic damage and aspiration of gastric contents. In many instances administration of neuromuscular blocking agents becomes essential. A suitable neuromuscular agent for such circumstances has been a topic of debate and continues to be.
Succinylcholine was considered the gold standard neuromuscular blocking agent in rapid sequence intubation, but because of its side effects such as hyperkalemia, muscle pain, increase in intraocular, intragastric and intracranial pressures, bradycardia with repeated use and its potential to cause malignant hyperthermia and prolonged apnea in susceptible individuals, the search is on for alternatives which have a comparable intubation time without these side effects [1,2]. The non depolarizing muscle relaxants, Vecuronium and Atracurium were also used to assess their effects [3]. With the recommended intubating doses of these compounds, suitable conditions for tracheal intubation developed after 2-3 minutes, significantly later than Succinylcholine [4].
It has been postulated that the rapid onset of action is almost only produced by a non-depolarizing neuromuscular blocking agent of relatively low potency. Two drugs that produced effects comparable to Succinylcholine were Rocuronium and Mivacurium. Many studies reported that Mivacurium did not produce satisfactory intubating conditions in spite of its rapid onset of action. Studies on Rocuronium revealed that as the dosage of the intubating dose increased, the duration of action also increased proportionately. The adverse effects of Rocuronium, like residual blockade was dose related [5].
Rocuronium bromide is an amino-steroid non-depolarizing neuromuscular blocking agent. In majority of the patients, clinically acceptable intubating conditions are obtained within 60-90 seconds after a 0.6 mg/kg dose of Rocuronium [5] with a clinical duration of action of 30-40 minutes. Magorian et al. [6] suggested that 0.9-1.2mg/kg Rocuronium may be an alternative to Succinylcholine where rapid intubation is required. This dosage which is used in order to achieve an onset of action closer to Succinylcholine correspondingly increases the clinical duration of action, which is not desirable for short and medium duration procedures. For this reason, various alternative methods were studied which would allow us to accelerate the onset of neuromuscular blockade with a standard intubating dose of Rocuronium.
The priming principle has been described by Foldes et al. [7] it consists of administrating a small dose of neuromuscular blocking agent 3-6 minutes prior to induction, allowing sufficient time for relaxant to reach the receptors and then administering a second larger dose to facilitate rapid intubation after induction. The priming principle can be applied to Rocuronium with an intubating dose of 0.6 mg/kg [5]. A priming dose of 0.06 mg/kg [8] (10% of intubating dose) & priming interval of 3 minutes 9 can be used in order to achieve a onset of action closer to Succinylcholine (54 seconds) [9,10].
Another modality is the use of Magnesium which inhibits presynaptic acetylcholine release at the motor end plate and acts as a minor calcium antagonist on the muscle itself. As a result, magnesium has been reported to potentiate the effect of non-depolarizing muscle relaxants and could shorten their onset time [11]. The present study is undertaken to evaluate the effect of magnesium pretreatment on the priming principle with Rocuronium in achieving rapid onset of intubating conditions and evaluation of conditions obtained during the same.
Aims and Objectives
Primary Objective
Comparison of the efficacy of magnesium pretreatment in conjunction with priming principle using Rocuronium in reducing the onset time of intubation.
Secondary Objective
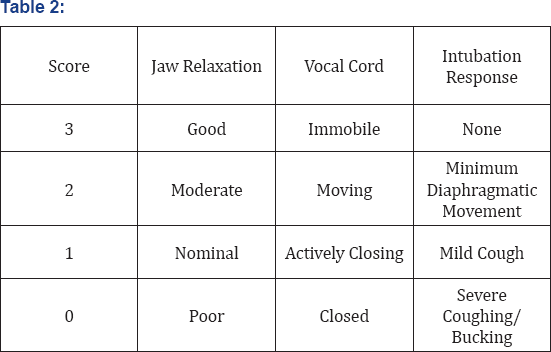
a. To assess the intubating conditions using Cooper's scoring system
b. To document and evaluate the adverse effects (if any) ensuing as a result of the study.
Materials and Methods
After obtaining the approval of the Institutional Review Board and the Ethical Committee, this prospective double blind randomized controlled study was conducted.
Source of data
Patients of ASA classification land 2, scheduled to undergo elective surgery under general anaesthesia in the tertiary care referral institute. Only patients who fulfilled the inclusion and exclusion criteria and were willing to participate in the study by giving an informed consent were a part of the study group.
Study Population
Study population consisted of ASA 1 and 2 patients scheduled to undergo elective surgery under general anaesthesia.
Study Design
This study was designed as a prospective, randomized, double blind, controlled Study.
Sample Size
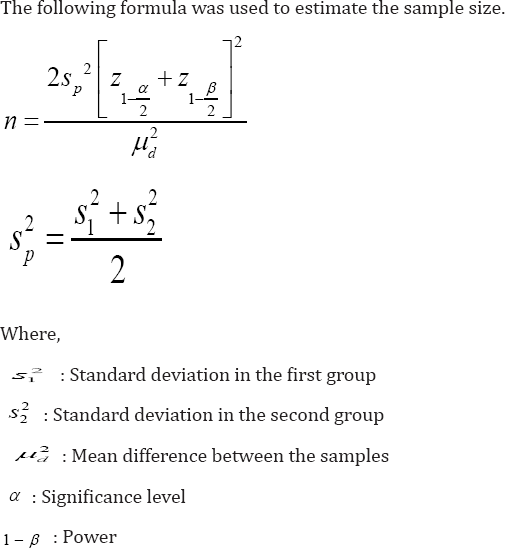
Sample size was estimated using N-MASTER software version 1. From literature review in a study "Rapid tracheal intubation with Vecuronium: The Priming Principle" by Sylvia Schwarz, Wiffed Mas et al, 21 it was found that the onset of neuromuscular block by using Vecuronium was 156 ±12 seconds (mean ± standard error of mean) and using Vecuronium priming it was 61 ± 3 seconds (mean ± standard error of mean). For the present study , 60 subjects in each group was required to get similar results with a precision of 95% confidence, 80% power and expecting 5 seconds difference as clinically significant.
Inclusion criteria
a. ASA Grade I and Grade II patients.
b. Age 18 yrs - 60 yrs.
c. Mallampatti Grade I and Grade II.
Exclusion criteria
a. Refusal of consent
b. Known or anticipated difficult airway.
c. Emergency surgeries.
d. Pregnant patients.
e. Patients with a BMI of 29 or more.
f. Patients with significant hepatic, renal, metabolic, neuro-muscular disorders.
g. Patients receiving drugs that influence neuro-muscular functions (Aminoglycosides, Polymyxin A & B, Colistin, Clindamycin, Lincomycin)
h. Those with allergy to Rocuronium.
Randomization
The patients who were registered received a unique identification number. These numbers were used for the randomization process. Patients who qualified for randomization were randomly assigned to the rocuronium priming group (Group R) or the rocuronium priming and magnesium pretreatment (Group RM). Randomization occurred after the screening procedure and eligibility confirmation.
Methodology
Rocuronium is available as 10 mg/ml vial. Magnesium Sulphate is available as 500mg/ml ampoule.
The intubating dose of Rocuronium used is 0.6 mg/kg of lean body weight.
Neuromuscular monitor
Fischer and Paykel Innervator 242 Patients were divided into rocuronium priming Group "R” and rocuronium priming and magnesium pretreatment group "MR” by using a computer generated random number table.
Blinding procedure
The patient and the investigators were both blinded to the study. An anaesthesiologist who was not directly involved in the study, prepared the drugs according to the protocol and allocated them to the study group as determined by the computer generated random number table. Another anesthesiologist who was not directly involved in the study received the prepared drug set and administered the same to the patient as per the protocol. He operated the TOF monitor and tabulated the required data thereafter. Intubation was performed by an experienced anesthesiologist who was also not involved in the study and was unaware of the group to which the patient belongs.
Preoperative checkup and premedication
A routine preoperative examination was done either the day prior to or well in advance of the day of surgery. Oral premedication was given to the subjects. On the night prior to the surgery tablet Alprazolam (0.5 mg) was given and tablet Pantoprazole (40 mg) was given at 6 am on the day of surgery. Informed consent was obtained after explaining the procedure to the patients.
Preparation
Prior to wheeling the patient inside the operation theatre; the anaesthesia machine, laryngoscope with Macintosh blade of appropriate size, working suction apparatus and the drug tray were checked. Difficult airway trolley consisting of appropriate size face masks, McCoy laryngoscope blade, bougie, laryngeal mask airway (LMA) of appropriate sizes, oropharyngeal / nasopharyngeal airway etc. were kept ready. Fibreoptic bronchoscopy was kept on standby for any unanticipated difficult airway. ASA difficult airway algorithm was to be followed in the case of any unanticipated difficult airway.
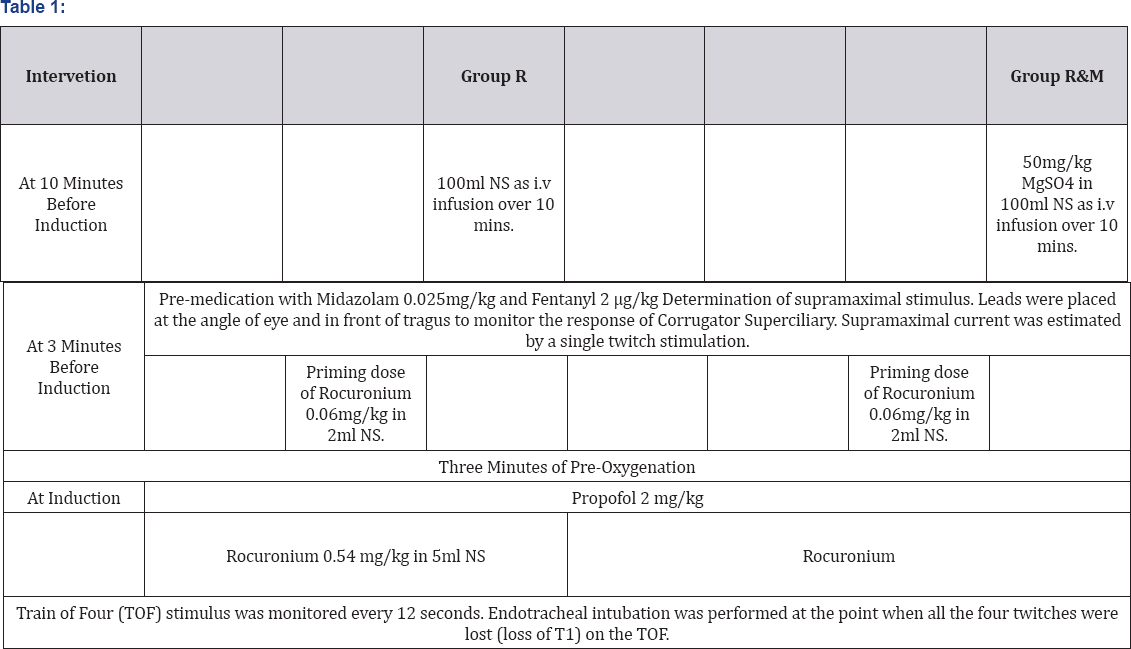
Induction and monitoring
On arrival in the OR, standard ASA monitoring including electrocardiogram (ECG), non-invasive blood pressure (NIBP), end tidal carbon dioxide (EtCO2) and pulse oximetry (SpO2) were attached. An appropriate size i.v cannula was secured and an infusion of 100ml NS placebo/study drug was infused over 10 minutes according to the study arm to which the patient was allotted (Table 1).
Hemodynamic parameters like heart rate, systolic and diastolic blood pressure were recorded at baseline during pre-oxygenation and one, three, five and ten minutes after induction. Trachea was intubated using a suitable size endotracheal tube. Anaesthesia was maintained with Isoflurane 1% in oxygen and air. Additional Fentanyl boluses of 1μg/kg were given as per requirement.
If difficult intubation was encountered, ASA difficult airway algorithm was to be followed and help was called for. A laryngeal mask airway, McCoy blade and/or a bougie was to be used as per the discrepancy of the anesthesiologist. If despite this, endotracheal intubation could not be performed; fibreoptic bronchoscopy was to be used to secure the airway and achieve endotracheal intubation. That subject was to be excluded from the study. Continuity of standard care was ensured.
The following parameters were recorded
a. Time to loss of T1 (loss of all four reflexes in TOF) from the intubating dose (T1 Time)
b. Time of completion of Intubation (I time)
c. Cormack Lehane Scoring
d. Cooper et al. [20] Scoring (Table 2)
e. Any adverse effects such as those listed below were noted.
i. Visual disturbances.
ii. Difficulty in controlling eyelids.
iii. Difficulty in moving fingers.
iv. Difficulty in breathing.
v. Difficulty in holding neck up.
f. Flushing, Generalised weakness.
Statistical Methods
The two groups were compared for
a. Differences or similarities in demographic parameters.
b. Differences in intubating conditions in terms of time required to completion of intubation (time to confirmation with capnography after intubation) and ease of intubation between the two groups.
c. Differences in terms of adverse events with and without a priming dose.
Statistical Tools
The information collected regarding all the selected cases were recorded in a Master Chart. Data analysis was done using the Epidemiological Information Package (EPI 2010) software. Using this software, range, frequencies, percentages, means, standard deviations, chi square and 'p' values were calculated. Student's 't test was used to test the significance of difference between quantitative variables and Fisher's chi square test for qualitative variables. A 'p' value less than 0.05 was taken to denote significant relationship.
Significant figures
+ Suggestive significance (P value: 0.05<P<0.10)
* Moderately significant (P value: 0.01<P ≤ 0.05)
** Strongly significant (P value: P≤0.01)
Results


Discussion
Onset time of intubation
Studies by Griffith et al. [9] & Rao et al. [13] established that priming principle applied to Rocuronium decreased the onset time by 42% and 46 % respectively. Kim MH et al. [2] further established that using Magnesium pre-treatment in conjunction with priming further decreased onset time by 26%. In our study, the onset time was 70.8 +/- 10.5 seconds with priming (Group R) and 62.8 +/- 10.2 seconds with priming and magnesium pretreatment (Group MR). Therefore, the time to onset of action was accelerated by 14.3% by using magnesium pretreatment in conjunction with rocuronium priming. This reduction in onset of action is statistically significant and certainly important when rapid onset of action is desired in case of rapid sequence induction and intubation. This resulted in the earlier completion of intubation, as reflected by the Intubation time (I time) which was 85.2 +/- 10.4 seconds with priming (Group R) and 73.0 +/- 9.1 with priming and magnesium pretreatment ( Group MR). The conditions of intubation as per the Cooper et al. [20] scoring were almost similar at the time of intubation in both the groups. Priming principle reduces the onset time of action of Rocuronium. This reduction in onset of action precludes the use of higher doses of Rocuronium for intubation as this can unnecessarily increase the duration of action of Rocuronium which is not desirable in many instances.
Facilitated neuromuscular blockade with Magnesium involves the following mechanisms [17]:
a. Decreased pre-junctional release of acetylcholine via the inhibition of voltage dependent calcium channels
b. Reduced sensitivity of the end plate to acetylcholine
c. Attenuation of direct excitability of muscle fibers,
presumably by altering the electrical threshold of the muscle membrane.The specific sites or stages at which neuromuscular transmission is impaired seem to differ between Magnesium and priming. Therefore, the number of phases of neuromuscular transmission that are inhibited presumably increase with the combination of Magnesium and priming, which may cause the synergistic acceleration of the effects of Rocuronium [18-21].
Most of the studies prove that there is reduction in onset of action of Rocuronium using the priming principle but there is no similar consensus among the studies regarding how much it reduces the time of onset, Naguib et al. [19] found the onset to be at 73 seconds, Griffith et al. [9] found it to be at 34 +/- 6 seconds, Rao et al. [13] found it to be at 50.67 +/- 7.39 seconds. The amount of reduction in onset time of action is different as per different studies. It can’t be stated that priming reduces the onset by a definite amount of time. The best possible way to determine the onset of action by using priming technique is by using peripheral nerve monitoring technique. The different onset of time of action can be explained on the basis of some factors which are not consistent among all these studies, such as;
a. Sample size variation.
b. Site of neuromuscular monitoring.
c. Technique of neuromuscular monitoring used in the study.
d. Amount of priming dose used.
e. Priming interval used in the study.
Griffith et al. [9] & Rao et al. [13] used Adductor pollicis muscle (Ulnar nerve) whereas in this study Corrugator supercilliary (Facial nerve) is used. Lee et al. [22] compared Adductor pollicis, Orbicularis oculi and Corrugator supercilii as indicators of adequacy of muscle relaxation for tracheal intubation and found that after administration of Rocuronium, twitch monitoring at the Orbicularis Oculi allows a faster intubation but is associated with a higher incidence of inadequate intubating conditions. Excellent intubating conditions are observed most frequently with Adductor Pollicis monitoring but with the longest delay before intubation is attempted. In our study, it was observed that monitoring of train of four response at the Corrugator Supercilii allows intubation earlier than that when train of four response at Adductor Pollicis was monitored; with no cincidence of inadequate intubating conditions. Griffith et al. [9] used single twitch method as the technique for determining the adequate time for intubation whereas all other studies have used the train of four methods. Sample size in the study conducted by Griffith et al. [9] was only 42 whereas in the study conducted by Rao et al. [13] it was 60, this study has a sample size of 120. Increase in sample size increases the precision of result.
There is a reduction in onset of time of action which can vary with the amount of drug used as priming dose and the priming interval. Higher amount of drug used as priming dose can decrease the onset time of action but it increases the incidence of adverse events related to priming. Longer priming interval also decreases the onset time of action but has the disadvantage of unnecesarily increasing the overall induction time which is undesirable when faster induction and intubation is required. Very few studies have compared the priming time required. Jose A et al. [23] found that the priming interval of 4 min allowed the fastest onset compared with 2 minutes & 6 minutes priming interval. Yavascaoglu B et al. [10] concluded that priming with a 3 minutes priming interval was effective when rapid tracheal intubation with Rocuronium was necessary. The differences in priming interval also add to the variations observed in the onset of time of action.
In another study by Czarnetzki C et al. [21], it was concluded that giving 60mg/kg Magnesium sulphate 15 min before propofol anaesthesia reduces the onset time of Rocuronium by about 35%. In our study, the Magnesium pretreatment group reduced the onset time of Rocuronium priming group by 14%. However, the point to be noted is that the onset time was already accelerated by the priming principle. Also, the dose of Magnesium used of 50mg/ kg and the pretreatment time of 10mins was substantially lower in our study. In our study, Application of the priming principle in both the groups resulted in lower onset times consistent with the aforementioned studies. In both the groups, the total dose of Rocuronium used for intubation was limited to 0.6mg/kg circumventing the complications of a larger dose. However, the use of Magnesium pretreatment in conjunction with priming provided a significant means to further accelerate the onset of action to the extent of mimicking Rapid Sequence Intubation conditions. Studies are being performed using different neuromuscular blocking agents such as Vecuronium as priming dose with the bolus intubating dose of Rocuronium to find out whether such techniques reduces the onset time of action further.
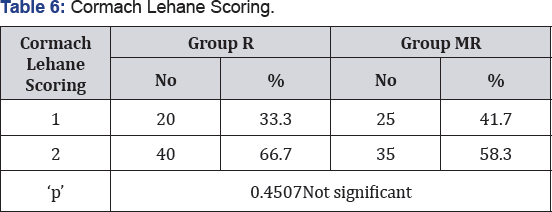
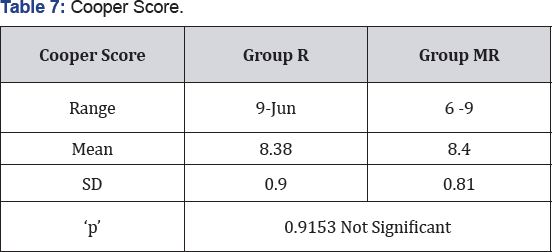
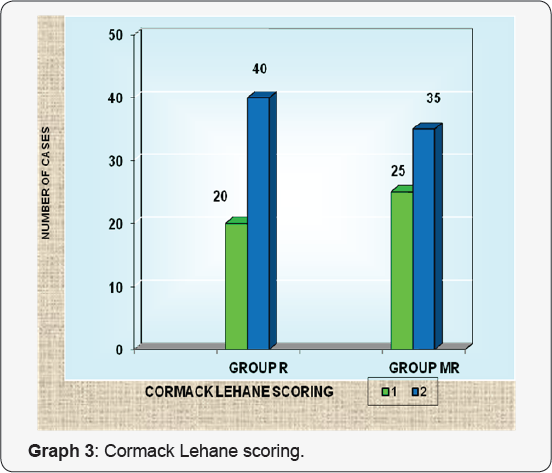
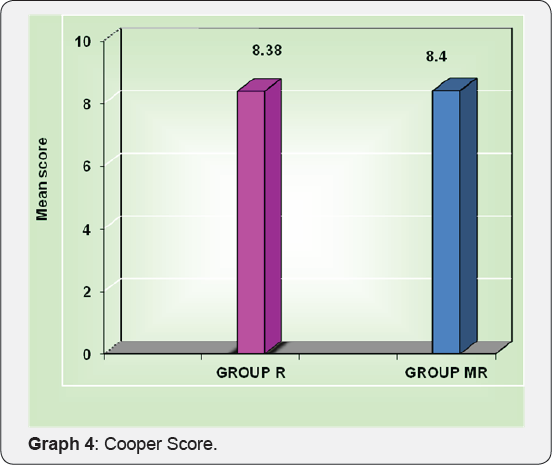
Intubating Condition
In the priming group R, the intubating conditions were excellent in 85% of the subjects and good in the remaining 15%. In the priming and pretreatment group MR, excellent conditions were obtained in 86.7% of the subjects and good intubating condition in the remaining 13.3% of the subjects. It concluded statistically that the conditions of intubation were comparable and favorable. This is in conjunction with studies by McCourt et al. [24] & Singh et al. [25]. The faster onset of action produced by the priming technique did not compromise the quality of neuromuscular blockade and intubating conditions. Intubating condition is primarily determined by the quality of neuromuscular blockade achieved at the time of intubation. However it requires mention that the intravenous induction agent used and the depth of anaesthesia acquired at the time of intubation by the usage of the intravenous induction agents also affects the condition of intubation to a lesser extent.
Adverse events
One ofthe major drawbacks ofpriming dose is the occurrence of adverse effects such as weakness, diplopia, dysphagia, generalized discomfort and breathing difficulties. Magnesium pretreatment could carry side effects such as flushing, pain on injection, generalised weakness etc [18]. Aziz et al. [26] documented the incidence of side effects such as ptosis and difficulty in swallowing on the use of priming with Vecuronium and Rocuronium in young and elderly patients. None ofthe patients in our study had evidence of such adverse effects of priming or magnesium pretreatment. The recommended magnesium doses for pretreatment are much lesser than that used for other therepautic interventions such as preeclampsia. The adverse events of priming can be avoided by limiting the priming dose of Rocuronium to 1/10th of the intubation dose and the priming interval to 3 minutes [10].
Conclusion
In rapid sequence induction and intubation or where anticipated difficulty in intubation exists with contraindications to the use of Succinylcholine, it is recommended that Rocuronium is used as a muscle relaxant at a higher dose of 1.2mg/kg body weight. However, this higher dosage has its drawbacks in the form of increased duration of neuromuscular blockade. As a result, there is a tendency to avoid the usage of Rocuronium owing to this, in centers where Sugammadex, a selective relaxant binding agesnt is not available. This study was designed to evaluate the efficacy of well established pharmacokinetic principles such as priming and magnesium pre-treatment on accelerating the onset of action of Rocuronium administered at a regular dose of 0.6mg/ kg body weight. The results establish that these interventions result in a statistically significant reduction in the onset time of action of Rocuronium and helps in achieving early endotracheal intubation when used in conjunction and mimicks rapid sequence intubation conditions. Rocuronium can be safely used with the priming principle. In addition, use of Magnesium pretreatment further accelerates the time to intubation. These interventions seem quite effective and safe when performed under monitored environments. Therefore, this should encourage anesthesiologists to use these principles in their practice albeit with a keen eye for potential complications.
References
- Booij LHDJ, Crul JF (1983) A comparison of Vecuronium with the hypothetical ideal neuromuscular blocking drug. Excerpta Medica 11: 3-8.
- Agoston S (1976) Muscle relaxants. In: Dukes MNG, Meyler's side effects of drugs: An encyclopedia of adverse reactions and interactions. Amsterdam, Netherlands, Elseiver pp. 262-303.
- Hans P, Brichant J F, Franzen A, Faleres X, Lamy M (1996) Comparison of neuromuscular block of Atracurium and Rocuronium in adults. Acta Anaesthesiol Belg 47(2): 53-8.
- Wierda JMK, Hommed FDM, Nap HJA, Broek L van den (1995) Time course of action and intubating conditions following Vecuronium, Rocuronium and Mivacurium. Anaesthesia 50(5): 393-396.
- Fuchs Buder T, Tassonyi E (1996) Intubating conditions and time course of rocuronium induced neuromuscular block in children. Br J Anaesth 77(3): 335-338.
- Magorian T, Flannery KB, Miller RD (1993) Comparison of rocuronium, succinylcholine, and vecuronium for rapid-sequence induction of anaesthesia in adult patients. Anesthesiology 79(5): 913-918.
- Foldes FF, Nagashima H, Nguyen H, Ohta Y (1990) he clinical pharmacology of Org 9426. Exerpta Medica 171-178.
- Huizinga ACT, Vandenbrom RHG, Wierda JHKH, Hommes FDM, Hennis PJ (1992) Intubating Conditions and onset of neuromuscular block of Rocuronium (Org 9426)a comparison with Suxamethonium. Acta Anaesthesiol Scand 36(5): 463-468.
- Griffith K, Joshi G, Whitman P, Garg S (1997) Priming with rocuronium accelerates the onset of neuromuscular blockade. Journal of clinical anesthesia 9(3): 204-207.
- Yavascaoglu B, Cebelli V, Kelebek N, Uckunkaya N, Kutlay O (2002) Comparison of different priming techniques on the onset time and intubating conditions of rocuronium. Eur J Anaesthesiol 19(7): 517521.
- Sang HK, Keum YS, Ki TJ (2012) Effect of magnesium sulphate pretreatment on onset and recovery characteristics of cisatracurium. Korean Journal Anaesthesiol 62(6): 518-523.
- Kim MH, Oh AY, Jeon YT, Hwang JW, Do SH (2012) A randomised controlled trial comparing rocuronium priming, magnesium pretreatment and a combination of the two methods. Anaesthesia 67(7): 748-754.
- Rao MH, Venkataraman A, Malleswari R (2011) Comparison of intubating conditions between rocuronium with priming and without priming: Randomized and double-blind study. Indian J Anaesth 55(5): 494-498.
- Schmidt J, Irouschek A, Muenster T, Hemmerling T M, Albrecht S (2005) A priming technique accelerates onset of neuromuscular blockade at the laryngeal adductor muscles. Canadian Journal of Anesthesia 52(1): 50-54.
- Dale HH (1914) The action of certain esters and ethers of choline and their relation to muscarine. J Pharmacol 6(2): 147-190.
- Nickalls RW, Nickalls EA (1985) The first reversal of curare. A translation of Pal's original paper, 'Physostigmine, an antidote to curare', 1900. Anaesthesia 40(6): 572-575.
- Czarnowski C, Bailey J, Bal S (2007) Curare and a Canadian connection. Can Fam Physician 53(9): 1531-1532.
- Wu H L, Ye TH, Sun L (2009) Effects of atracurium pretreatment with magnesium on speed of onset, duration, and recovery of neuromuscular blockade. Acta Academiae Medicinae Sinicae 31(1): 73-76.
- Naguib M, Samarkandi AH (2001) The use of low dose Rocuronium to facilitate laryngeal mask airway insertion. Middle East J Anaesthesiol 16(1): 41-54.
- Cooper R, Mirakhur RK, Clarke RSJ, Boules Z (1992) Comparison of intubating conditions after administration of Org 9426 (Rocuronium) and suxamethonium. Br J Anaesth 69(3): 269-273.
- Czarnetzki C, Lysakowski C, Elia N, Tramer MR (2010) Time course of rocuronium-induced neuromuscular block after pre-treatment with magnesium sulphate: a randomized study. Acta Anaesthesiol Scand 54(3): 299-306.
- Lee H, Kim K, Jeong J, Cheong M, Shim J (2009) Comparison of the adductor pollicis, orbicularis oculi, and corrugator supercilii as indicators of adequacy of muscle relaxation for tracheal intubation. Br J Anaesth 102(6): 869-874.
- Jose A, Miller R, Rupp S (1986) Refining the priming principle for vecuronium during rapid sequence intubation of anaesthesia. Anaesthesiology 64(2): 243-247.
- McCourt K, Salmela L, Mirakhur R, Carroll M, Kansanaho M, et al. (1998) Comparison of rocuronium and suxamethonium for use during rapid sequence induction of anaesthesia. Anaesthesiology 53(9): 867-871.
- Singh A, Bhatia P, Tulsiani K (2004) Comparison of onset time, duration of action and intubating conditions achieved with suxamethonium and rocuronium. Indian journal of Anaesthesia 48(2): 129-133.
- Aziz L, Jahangir SM, Chandhary SN, Rahman K, Ohta Y, et al. (1997) The effect of priming with vecuronium and rocuronium on young and elderly patients. Anesth Analg 85: 663-666.






























