Catastrophic Cryoglobulinemic Vasculitis with Symmetrical Proximal Limb Gangrene - A Rare Case Report
Kasimahanti Rajesh*, Syed nabeel muzaffer and Afzal Azim
Department of Critical care medicine, Sanjay Gandhi Post Graduate Institute of Medical Sciences, India
Submission: September 22, 2017; Published: November 27, 2017
*Corresponding author: Rajesh Kasimahanti, Department of Critical care medicine, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Pin: 226014, India, Email: rajeshkasimahanti@gmail.com
How to cite this article: Kasimahanti R, Syed n m, Afzal A. Catastrophic Cryoglobulinemic Vasculitis with Symmetrical Proximal Limb Gangrene - A Rare Case Report . J Anest & Inten Care Med. 2017; 4(3) : 555641. DOI: 10.19080/JAICM.2017.04.555641
Abstract
A young male referred to our hospital with symptoms of febrile illness with development of extensive gangrenous changes in the limbs and extensive purpura of all the limbs. He was found positive for anti hepatitis C antibody. To introspect about etiologies behind the symmetric peripheral gangrene (SPG), work up for cryoglobulins done which was found to be positive. This was suggestive for possibility of catastrophic cryoglobulinemic vasculitis, secondary to hepatitis C with multi organ involvement. He received pulse therapy of steroid and plasmapheresis. During further stay in intensive care unit he developed wet gangrenous changes over all the four limbs with septic shock and underwent bilateral above knee amputation.
Abbreviations: SPG: Symmetric Peripheral Gangrene; TEG: Thrombo Elastography; BUN: Blood Urea Nitrogen; HCV: Hepatitis C Virus
Keywords: Symmetrical peripheral gangrene; Cryoglobulinemic vasculitis; Hepatitis C; Multi organ failure
Introduction
Cryoglobulins are immune complexes that may induce a systemic vasculitis involving mainly the skin, joints, peripheral nervous system and kidneys. They may give rise to distinct clinical manifestations varying from a hyper viscosity syndrome to vasculitic manifestations, which may present with gangrene. Symmetrical peripheral gangrene (SPG) is a rare but well documented clinical syndrome characterised by symmetrical acrocyanosis leading to gangrene of more than two sites [1,2]. Presence of SPG with cryoglobulins is relatively rare and usually involves the digits [3,4]. Involvement of proximal limbs and extensive skin involvement is a much rarer presentation and according to our knowledge till now no cases have been reported. Here we report a rare case of hepatitis C related cryoglobulinemia which presented with rapidly progressing symmetrical peripheral gangrene.
Case Description
A previously healthy 32 year old male patient presented to us with a history of fever and malaise for one week and development of non itchy maculopapular rash over the anterior part of chest and abdomen on fourth day of illness with development of blackish discoloration of tips of all digits with predominant involvement of toes. The discoloration progressed up to wrist joint in upper limbs and beyond knee joint in lower limbs bilaterally over 6 hours after initial detection. He developed acute respiratory failure requiring mechanical ventilation within next few hours. Over a period of 24 hours acrocyanosis with pregangrenous change of limbs worsened further with development of extensive purpura of both lower limbs extending up to lower abdomen and back. During this course, he did not receive any beta blocker, vasopressors, any alternative medications or recreational drugs. There was no history of altered sensorium, seizures. No past history suggestive of autoimmune disease.
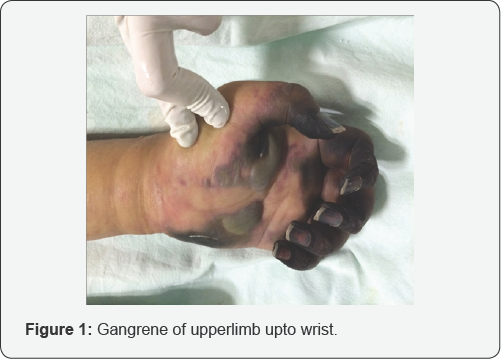
On examination he had palpable feeble distal pulses bilaterally. Blood pressure was 150/90 with MAP≥100. There were a diffuse maculopapular erythematous rashes on his chest and upper limbs. He was pale and icteric. There was no palpable lymphadenopathy. Examination of the limbs confirmed gangrene involving the upper limbs upto the wrists and the lower limbs upto the mid thighs bilaterally. He was received in a sedated state, moved all 4 limbs to painful stimuli and both plantars were flexor. There was no neck rigidity. Chest and abdomen examination were normal. A differential diagnosis of DIC due to infectious cause secondary to acute tropical illness, thromobotic thrombocytopenic purpura/haemolytic uremic syndrome, catastrophic antiphospholipid antibody syndrome were considered and investigated. He was started on broad spectrum antibiotics, heparin infusion for pregangrenous changes along with dobutamine infusion.
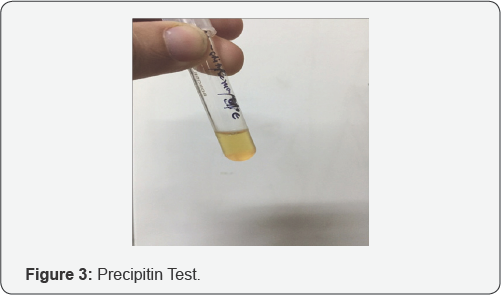
Doppler study showed decreased flow in bilateral popliteal, dorsalis pedis, and radial arteries. 2D echocardiography was normal without any signs of infective endocarditis. Initial Haemoglobin 7gm%, leucocytes count 13000, platelets count 75000. Serum creatinine was 2.8mg/dl with BUN 68, urine proteins were 3+ and granular casts were 2+. Total bilirubin was 6.6, direct bilirubin was 4.1, SGOT and SGPT were 201U/ml and 88U/ml, INR was 1.4, and serum albumin levels were 2.5mg/dl. Peripheral smears showed normocytic normochromic anaemia with schistocytes < 1%. DIC work up showed fibrinogen levels 177mg/dl, D dimers were positive, TEG was normal and serum LDH was 1026 U/L.C3 level was 112mg/dl(60-120),C4 level was 17.3mg/dl (15-25). IgM level was 140mg/dl (60-280), IgG antibody was 1200mg/dl(800-1800). Rheumatoid factor, direct and indirect coombs test were negative. Test for cryoglobulin levels were positive, antinuclear antibody levels and anticardiolipin antibodies were negative. Anti Hepatitis C IgM antibodies were positive and tests for other viruses were negative. Initial paired blood cultures and endotracheal aspirate cultures were negative.
Tropical fever work up was negative. Based on the clinical picture with lab evidence of positive cryoglobulins and association of HCV, we made the diagnosis of HCV related mixed cryoglobulinemia with organ involvement in the form of glomerulonephritis, vasculitis in the form of purpura and symmetric peripheral gangrene of limbs. Initially he was started on pulse therapy of methyl prednisolone for 3 days and then tapered gradually. He was also started on therapeutic plasma exchange for 3 cycles. Over the period of therapy he developed wet gangrenous changes and taken for bilateral above knee amputation. Following the surgery he was continued with plasma exchange along with broad spectrum antibiotics. Despite of best possible efforts he could not be salvaged due to severe worsening septic shock with multi organ dysfunction. (Figures 1-3).

Discussion
Cryoglobulins are the immunoglobulins that precipitate reversibly to cold. Three types of cryoglobulins are identified based on the composition. Essential mixed cryoglobulinemia (type II and III) is a rare disease and it is associated with HCV in 90% of cases [6]. Out of all patients with HCV related disease, 12 to 56% of patients show positive test for cryoglobulin. Out of all patients with positive test for cryoglobulins only 2-15% of patients develop vasculitis features [6]. So presence of symptomatic vasculitis in HCV related disease is a relatively rare phenomenon. Among type II and III, cutaneous involvement in form of purpura is seen in 25% of the symptomatic cases where as renal, neurological and articular involvements occur in 21-38% of the symptomatic patients [6].
Digital ischemia and gangrene comprise only 2% of cases with skin involvement [6]. Cryoprecipitate test with cryocrit >5% clinches the diagnosis and it will be further supported by abnormal immunoglobulin assay in serum electrophoresis. De vita et al. [8] criteria includes determination of cryoglobulins in serum atleast twice in 12 week period and satisfaction of questionnaire item, clinical item and laboratory item. This has a sensitivity of 88.5% (84.3% - 92.8%) and specificity of 93.6% (83.5% - 97.7%) [5,8]. Current literature for life threatening cryoglobulinemic vasculitis shows a mortality rate of 63% - 80% with multi organ involvement. 2 - 5% of patients presents with rapidly progressing, life threatening vasculitis and they require aggressive management in the form of plasma exchange along with steroid supplementation and rituximab [9]. Anti viral therapy in these patients will be started after patient's stabilization. The understanding of the HCV related cryoglobulinemic vasculitis has increased in the last few decades with use of anti viral and anti neoplastic agents. Authors conclude that HCV related cryoglobulinemia can present with acute, rapidly progressing, catastrophic multi organ failure with proximal limb gangrene.
References
- McGouran RC, Emmerson GA (1977) Symmetrical peripheral gangrene. Br Heart J 39(5): 569-572.
- Davis MD, Dy KM, Nelson S (2007) Presentation and outcome of purpura fulminans associated with peripheral gangrene in 12 patients at Mayo Clinic. J Am Acad Dermatol 57(6): 944-956.
- Abdel-Gadir A, Patel K, Dubrey SW (2010) Cryoglobulinaemia induced digital gangrene in a case of hepatitis C. BMJ Case Rep 20: 2010.
- Mironiuc A, Comes L, Constantinescu I, Mironiuc C, Bontea D (2008) Cryoglobulinemic vasculitis with multiple digital necrosis in viral hepatitis. Rom J Intern Med 46(1): 91-95.
- Damoiseaux J (2014) The diagnosis and classification of the cryoglobulinemic syndrome. Autoimmun Rev 13(4-5):359-362.
- Trejo O, Ramos Casals M, Garcia Carrasco M, Yague J, Jimenez S, et al (2001) Cryoglobulinemia: Study of etiologic factors and clinical and immunologic features in 443 patients from a single center. Medicine (Baltimore) 80(4): 252-262.
- Krishnaram AS, Geetha T, Pratheepa, Saigal A (2013) Primary cryoglobulinemia with cutaneous features. Indian J Dermatol Venereol Leprol 79(3): 427-430.
- De Vita S, Soldano F, Isola M, Monti G, Gabrielli A, et al. (2011) Preliminary classification criteria for the cryoglobulinaemic vasculitis. Ann Rheum Dis 70: 1183-1190.
- Dammacco F, Sansonno D (2013) Therapy for hepatitis C virus related cryoglobulinemic vasculitis. N Engl J Med 369(11): 1035-1045.






























