Incidental Hydatid Cyst Masquerading the Diagnosis Of Catastrophic Anti-Phospholipid Syndrome (CAPS)
Syed nabeel muzaffer, Kasimahanti Rajesh* and Afzal Azim
Department of Critical care medicine, Sanjay Gandhi Post Graduate Institute of Medical Sciences, India
Submission: September 22, 2017; Published: November 21, 2017
*Corresponding author: Rajesh Kasimahanti, Department of Critical Care Medicine, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India, Pin: 226014; Email: rajeshkasimahanti@gmail.com
How to cite this article: Syed nabeel m, Kasimahanti R, Afzal A. Incidental Hydatid Cyst Masquerading the Diagnosis Of Catastrophic Anti-Phospholipid Syndrome (CAPS). J Anest & Inten Care Med. 2017; 4(2) : 555635. DOI:10.19080/JAICM.2017.04.555635
Abstract
A young male patient was referred to our hospital with a diagnosis of cerebral hydatid cyst with recurrent seizures and respiratory failure. Seizures were attributed to hydatid cyst diagnosed on CT Head. After admission and initial stabilisation the sensorium did not improve. Subsequently, he developed hypotension and acute kidney injury requiring vasopressor support and renal replacement therapy. MRI brain was done which showed a large infarct in left middle cerebral artery (MCA) territory. To introspect about etiologies behind the infarct, thrombophilic workup was sent in which anticardiolipin antibodies were elevated suggesting a possibility of underlying catastrophic APLA syndrome (CAPS).
Abbreviations: MCA: Middle Cerebral Artery; CAPS: Catastrophic Apla Syndrome; APS: Antiphospholipid syndrome; DVT: Deep Vein Thrombosis; MI: Myocardial Infarction; PE: Pulmonary Embolism; TIE: Transient Ischemic Attack; IV: Intra Venous; MAP: Mean Arterial Pressure; TLC: Total Leukocyte Count; AKI: Acute Kidney Injury; BUN: Blood Urea Nitrogen; Acl: Anti-Cardiolipin; TEG: Thromboelastography; aPL-Abs: Anti Phospholipid Antibodies; β2 GP1: β2 glycoprotein 1; PT: Prothrombin; SIRS: Systemic Inflammatory Response Syndrome; IVIG: Intravenous Immunoglobulin; MOF: Multi-Organ Failure; CNS: Central Nervous System; MA: Maximum Amplitude; CI: Coagulation Index
Keywords: Infarct; Anti Cardiolipin Antibodies; Catastrophic APLA syndrome (CAPS); Multi-organ failure (MOF)
Introduction
Antiphospholipid syndrome (APS) is a systemic disease that presents with recurrent venous and/or arterial thrombosis, recurrent fetal losses associated with moderate thrombocytopenia and positive anti-phospholipid antibodies (aPL-abs). When multi-organ failures set in rapidly and dominate the clinical course of APS, this condition is termed as catastrophic antiphospholipid syndrome (CAPS) [1]. The gamut of clinical presentation is wide and in descending order of frequency includes deep vein thrombosis of lower limbs (DVT), stroke, superficial vein thrombosis, pulmonary embolism (PE), transient ischemic attack (TIE) and myocardial infarction (MI). Fetal manifestations include early and late fetal loss and premature birth [2]. We report a case of CAPS in which the diagnosis was delayed due to co-existing hydatid cyst. A written and informed consent was taken from the patient’s relative.
Case Description
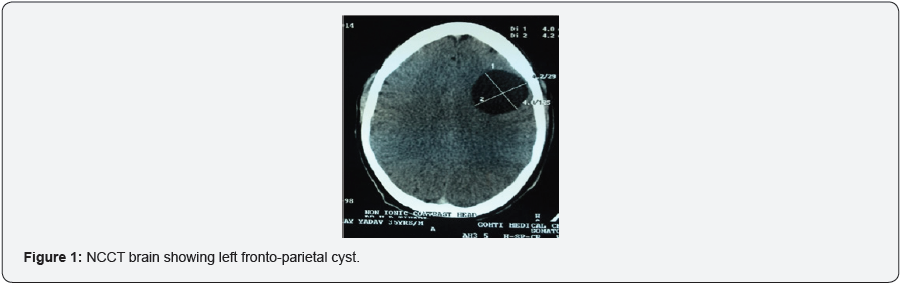
35 years old male, farmer by occupation, with no comorbidities and addiction, presented to a local hospital with history of low grade fever for two days and recurrent seizures for one day. Due to poor sensorium (GCS < 8), he was immediately intubated and mechanically ventilated. NCCT brain was done (Figure 1) on day 3 of illness which was inconclusive except for a left fronto-parietal hydatid cyst. Within next 24 hours, he developed hypotension requiring intravenous (IV) vasoactive drug support (noradrenaline infusion upto 0.05-0.1 micrograms/ kg/min) to maintain mean arterial pressure (MAP) ≥ 65mmHg. Subsequently, he sustained acute kidney injury (AKI) with marked derangement in renal functions (serum creatinine = 6 mg/dl and blood urea nitrogen (BUN) = 120 mg/dl) and worsening metabolic acidemia. He was referred to our hospital for further management with a provisional diagnosis of acute febrile illness with left fronto-parietal hydatid cyst with status epilepticus with AKI.

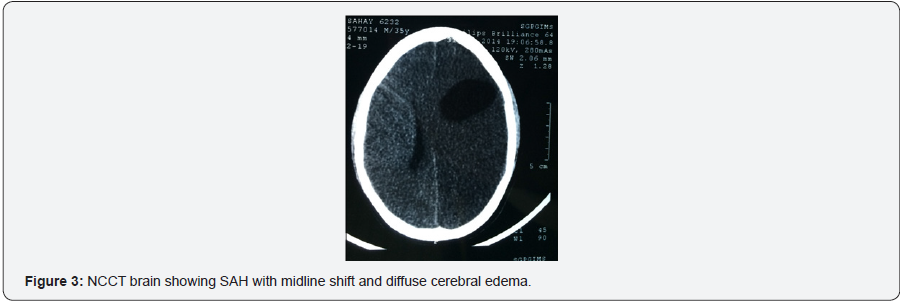
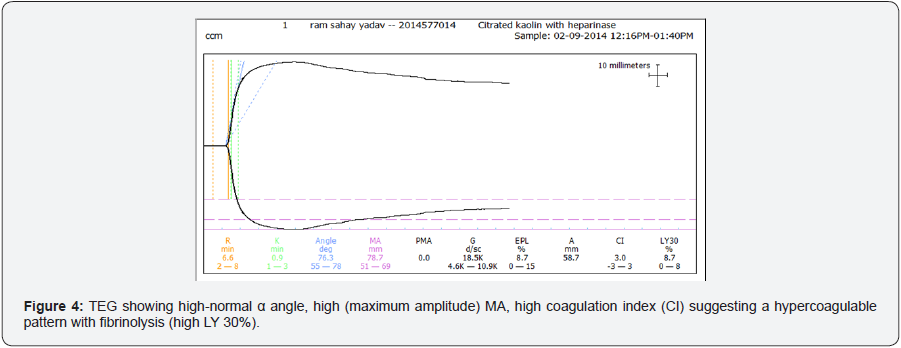
On admission, he was deeply sedated, pupils were equal in size (2.5 mm) and normally reacting to light, tone and reflexes were depressed. No lateralizing signs were present. Investigations on admission were Hb = 9g/dl, total leukocyte count (TLC) = 15,000/mm3, BUN = 153mg/dl, serum creatinine = 9 mg/dl, INR = 1.1, platelets = 86,000/mm3. After initial stabilisation, MRI brain was done (Figure 2) for confirmation of diagnosis which showed a large left-sided MCA infarct. Cerebral protection strategy was implemented. Considering the clinical presentation thrombophilic screen was sent to explore the etiologies of infarct in a young patient with no other risk factors. Anti-phospholipid antibodies (aPL-abs) turned out to be significantly positive (IgM anti-cardiolipin (aCL) antibodies= 54.5MPL/ml (reference value = 3-18 MPL/ml) raising a possibility of CAPS. Carotid doppler done bedside was normal. Thromboelastography (TEG) was done which showed a hypercoagulable pattern. Anticoagulation with corticosteroids was started immediately. However the patient developed septic shock and succumbed to his illness in next 72 hours of ICU stay.
Discussion
In APS, auto-antibodies are found which are directed against proteins bound to anionic phospholipids and are responsible for the genesis of a thrombotic background. They are known as antiphospholipid antibodies (aPL-Abs) and include antibodies directed against β2 glycoprotein 1 (β2 GP1), prothrombin (PT), protein C complex, annexin A5 and proteins of the coagulation cascade and fibrinolytic system [3,4]. The prevalence of these antibodies ranges from 1-10 % in general population and is upto 30% in those presenting with thrombosis. When multi-organ failures set in rapidly and dominate the clinical course of APS along with features of systemic inflammatory response syndrome (SIRS), this condition is termed as CAPS. CAPS are seen in <1% cases of APS and is the most severe form of APS. Unlike APS, where large vessel occlusions dominate the clinical picture, small vessel occlusive disease is predominant in CAPS.
The common precipitating or triggering factors that are implicated in pathogenesis of CAPS in descending order of frequency are idiopathic, infections, trauma, neoplasia and obstetric or surgical procedures. In the case series described by Asherson [6] renal involvement was present in 78%, followed by lung (66%), central nervous system (CNS) (56%), skin and heart (50%), gastrointestinal (38%), and adrenal gland (26%) involvement [6]. Management of CAPS is challenging and there are two vital aspects in its management [7]. Any underlying infection in patients with APS should be treated with antibiotics and standard anti-coagulation therapy and high-dose corticosteroids should be considered in every patient presenting with CAPS. Early addition of plasma exchange and/or intravenous immunoglobulin (IVIG) should be considered in patients who do not respond promptly to anticoagulants and corticosteroids.
The mortality of CAPS remains high (> 50%) despite all available contemporary therapies. In this patient, the incidental finding of left-sided hydatid cyst had obscured the co-existing MCA infarct so he could not receive an early and appropriate management for the infarct. So, the disease process might have progressed leading to the catastrophic presentation. On further work up, ApL-abs turned out to be positive. Our patient succumbed to his illness within 72 hours of admission, so antibody levels could not be repeated. Therefore, a high index of suspicion for CAPS should be kept in mind while managing young patients with stroke and multi organ failure.
References
- Donadini MP, Crowther M (2010) Antiphospholipid Syndrome: A Challenging Hypercoagulable State with Systemic Manifestations. Hematol Oncol Clin N Am 24(4): 669-676.
- Cervera R, Piette JC, Font J, Khamashta MA, Shoenfeld Y, et al. (2002) Antiphospholipid syndrome: clinical and immunological manifestations and patterns of disease expression in a cohort of 1000 patients. Arthritis Rheum 46(4): 1019-1027.
- Miyaki S, Lockshn MD, Atsumi T, Branch DW, Brey RL (2006) International consensus statement on an update of the classification criteria for definite antiphospholid syndrome (APS). J Thromb Haemost 4(2): 295-306.
- Westney GE, Harris EN (2002) Catastrophic antiphospholipid syndrome in the intensive care unit. Crit Care Clin 18(4): 805-817.
- Cervera R, Asherson RA, Font J (2006) Catastrophic antiphospholipid syndrome. Rheum Dis Clin N Am 32: 575-590
- Asherson RA, Cervera R, Piette JC, Font J, Lie JT, Burcoglu (1998) Catastrophic antiphospholipid syndrome: Clinical and laboratory features of 50 patients. Medicine (Baltimore) 77(3): 195-207
- Asherson RA (2005) Multiorgan failure and antiphospholipid antibodies: the catastrophic antiphospholipid (Asherson’s) syndrome. Immunobiology 210(10): 727-733.






























