Tourniquet Pain after Ultrasound-Guided Axillary Blockade
Maria P Sebastian1*, Aitziber Etxebarria1, Pilar Perez1, Zurinñ Lauzirika1, Ane Anton-adislao2 and Rafael Martinez-Bourio1
1Department of Anesthesiology, Resuscitation, and Pain Management, Hospital Galdakao-Usansolo, Spain
2Unit of research, OSI Barrualde-Galdakao, and network of research in health services in chronic diseases (REDISSEC in Spanish), Spain
Submission: May 16, 2017; Published: September 18, 2017
*Corresponding author: MP Sebastian, MD, From the Department of Anesthesiology, Resuscitation, and Pain Management, Hospital Galdakao- Usansolo, Vizcaya, Spain, Email: sebastianmariapaz@gmail.com
How to cite this article: Maria P S, Aitziber E, Pilar P, Zuriņe L, Ane A, Rafael M. Tourniquet Pain after Ultrasound-Guided Axillary Blockade. J Anest & Inten Care Med. 2017; 3(5) : 555624. DOI: 10.19080/JAICM.2017.03.555624
Abstract
Objective: To analyse tourniquet pain after ultrasound guided axillary block (AXB) as the sole anesthetic technique with no injection of local anaesthetic into the subcutaneous tissue of the posterior half of the axilla to prevent tourniquet pain.
Material/patients and methods: 84 patients older than 18 years ASA I-IV undergoing surgery at hand, wrist, forearm and elbow under ultrasound guided AXB requiring upper arm tourniquet, we studied prospectively. Exclusion criteria included refusal to participate, communication problems, pre-existing neuropathy, coagulopathy or allergy to local anaesthetics. Tourniquet pain was assessed according to visual analogue scale (VAS) every 15 minutes. We also analysed differences in tourniquet pain between sedated and non-sedated patients.
Main results: VAS was 0 during ischemia in 83 patients. One patient reported tourniquet pain. This was mild (VAS = 3) and reported during the first 15 minutes of ischemia. VAS dropped to 0 from then on. The median ischemia time was 62 minutes (IQR 45-86) and the median surgery time was 60 minutes (IQR 40-89.5). Intraoperative sedation was administered to 48.8% of patients. Sedated and non-sedated groups were similar. No statistical differences were found regarding tourniquet pain between both groups (p< 0.05).
Conclusion: Ultrasound guided AXB is sufficient to provide anaesthesia for tourniquet even during prolonged ischemia. However, to ensure prevention of tourniquet discomfort a multiple injection technique that include musculocutaneous blockade should be preferred.
Keywords: Tourniquet pain; Axillary block; Ultrasound-guided peripheral nerve block; Upper limb surgery; Sedation
Background
Regional anaesthesia holds potential advantages when compared to general anaesthesia. Particularly, brachial plexus blockade has demonstrated superior analgesia, reduction of opioid-related side effects and opioid consumption during the first 24 hours after surgery [1]. The axillary blockade (AXB) provides anaesthesia for upper extremity surgery of the elbow, forearm, wrist, and hand [2,3]. It has been shown as effective as supraclavicular (SCB) and infraclavicular (ICB) blocks [4] but its distal location from pleura and phrenic nerve eliminates some of the risks related to those more proximal approaches [5,6].
Ultrasound guidance allows direct observation of nerves, surrounding structures and local anaesthetic (LA) spread. Its use decreases complications and onset time [7,8], improves quality [8] and reduces the volume of LA required [9]. Due to the superficial location of the brachial plexus in the axilla, ultrasound guided AXB provides excellent visibility of both nerves and needle.
The intercostobrachial nerve (T2) is not part of the brachial plexus. It communicates with the medial brachial cutaneous nerve (C8-T1) providing innervation to the skin of the axilla and the medial and posterior aspect of the arm. The block of these nerves to prevent tourniquet pain is widely extended and has been traditionally recommended using an injection of LA into the subcutaneous tissue of the posterior half of the axilla ("semicircular subcutaneous anaesthesia" or "ring block") [1014]. However, its importance in reducing tourniquet pain has never been established and is questioned [2,15,16]. The aim of this study was to assess tourniquet pain after ultrasound guided AXB as the sole anaesthetic technique. Due to the fact that intraoperative sedation could underestimate tourniquet pain, further analyses comparing tourniquet pain in sedated and nonsedated patients were also carried out.
Material and Methods
A prospective observational study of tourniquet pain on patients who received an ultrasound guided AXB was conducted over a four month period (January- May 2013) at Galdakao- Usansolo Hospital. The study was classified as service evaluation and no ethical approval was needed as required no alteration to the routine standard of care, there was no therapeutic or equipment intervention, and no planned change to anaesthetic technique. Written consent from patients was obtained. Inclusion criteria were patients undergoing surgery at or below the elbow under ultrasound guided AXB requiring upper arm tourniquet, age >18 years and ASA (American Society of Anaesthesiologists) status I-IV. Exclusion criteria were refusal to be included, communication problems or inability to cooperate, pre-existing neuropathy, coagulopathy or allergy to LA.
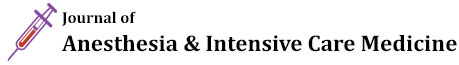
After patient arrival to theatre an intravenous catheter was placed in the upper limb contralateral to the surgical site and ASA standard monitoring were applied. Ultrasound guided AXB were performed by either consultants with expertise in regional anaesthesia or residents supervised by those consultant. A portable ultrasound machine (Sonosite M-Turbo®) and high frequency linear probe was used. Administration of premedication or intraoperative sedation was left to the discretion of the treating anaesthesiologist. The ultrasound probe was applied in the axilla to obtain a short-axis view of the axillary artery. The four terminal nerves (median, ulnar, radial and musculocutaneous nerve) were sought out and their identity confirmed by scanning distally along the arm following the characteristic course that each nerve takes. A 22 gauge needle (Braun Stimuplex D) was used to surround each individual nerve with LA after skin infiltration with lidocaine 1% (Figure 1). The AXB approach (in plane or out of plane) and the type and amount of LA was decided by the anaesthetist who performed the block.
AA: Axillary Artery; RN: Radial Nerve; UN: Ulnar Nerve; MN: Median Nerve; MsN: Musculocutaneous nerve; Conjoint tendon of the latissimus dorsi and teres major
Once the block was finished, a pneumatic tourniquet was applied to all patients on the mid-upper arm over a single wrap of cotton wool padding. The limb was exsanguinated using an Esmarch bandage and the tourniquet cuff inflated between 250- 300mmHg.
The variables collected included age, gender, weigh, ASA status, type of surgery, premedication administered, type and amount of local anaesthetic used to surround each nerve, time between the end of the block and the tourniquet inflation, pressure of the tourniquet, ischemia and surgery time, intraoperative sedation and tourniquet pain. The primary objective was to analyse tourniquet pain assessed according to a 0-10cm visual analogue scale (VAS), whereby '0' represents no pain and '10' represents the worst imaginable pain. Tourniquet pain was measured directly after the tourniquet was inflated and thereafter every 15 minutes (min) until the tourniquet was deflated. VAS evaluations were conducted by the same person who performed the block. As a second objective we analysed differences in tourniquet pain between intraoperative sedated and non-sedated patients.
Statistical analysis
Descriptive analysis of socio-demographic and clinical variables was made by using frequencies and percentages for categorical variables and means and standard deviations for continuous variables. The exception being variables with a high level of deviation. These were represented by median and interquartile range. The differences between sedated and non-sedated patient were evaluated using the Chi-square test (or Fisher exact test when expected values<5) for categorical variables and non-parametric Wilcoxon test for continuous variables. All effects were considered significant at p<0.05. All statistical analyses were performed using SAS for Windows statistical software, version 9.2 (SAS Institute, Inc., Carey, NC).
Results
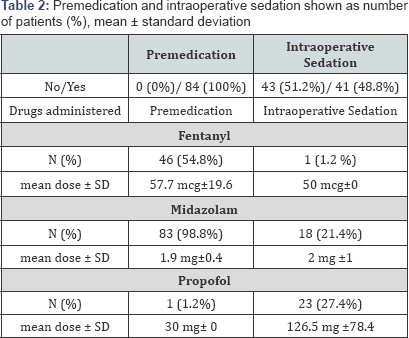
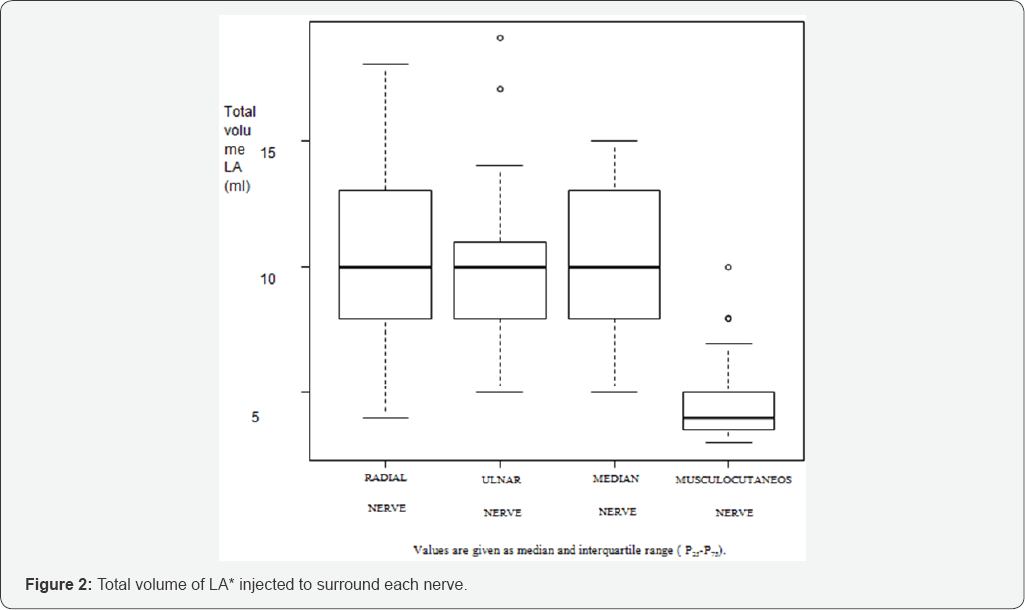
Over the four month period 84 patients were recruited.Patient characteristics and type of surgery are summarized in Table 1. All patients received premedication prior to the block. Intraoperative sedation was administered to 48.8% of patients. Sedatives used to sedate patients during surgery were propofol and midazolam but one patient received 50 mcg of fentanyl (Table 2). Mepivacaine 1.5% were the LA of choice to surround the four nerves in all patients. Occasionally Ropivacaine 0.2% or Levobupicaine 0.25% were added to provide longer analgesia. The mean total volume of LA used was 34.37±5.37 ml (Figure 2).


The median time since the block was finished until the cuff was inflated was 10min (IQR 5-15). The median surgery time was 60 min (IQR 40-89.5) and the median ischemia time was 62min (IQR 45-86) (Table 3).
Among 84 patients included, 83 scored tourniquet pain as VAS = 0cm during the time tourniquet was inflated. One of these patients complained about pain in the surgery field without pain on the tourniquet site after 180min of surgery and had to undergo general anaesthesia. In this case, a 30min reperfusion period was used after 135min of ischemia and the total ischemia time with the patient awake was 150 min. One patient reported tourniquet pain. In this patient VAS was 3 cm when the cuff was inflated and in the following 15 minutes. He was administered 50mg of fentanyl and 20mg of propofol respectively. Since then VAS reminded 0cm until the tourniquet was deflated 31 minutes later. No more sedatives were administered.
Sedated and non-sedated groups were similar in demographic variables, ASA status, premedication administrated, type of surgery, type and amount of LA used, time of ischemia and surgery and tourniquet pressure. No statistical differences (p< 0.05) were found regarding tourniquet pain between both groups (Table 4).
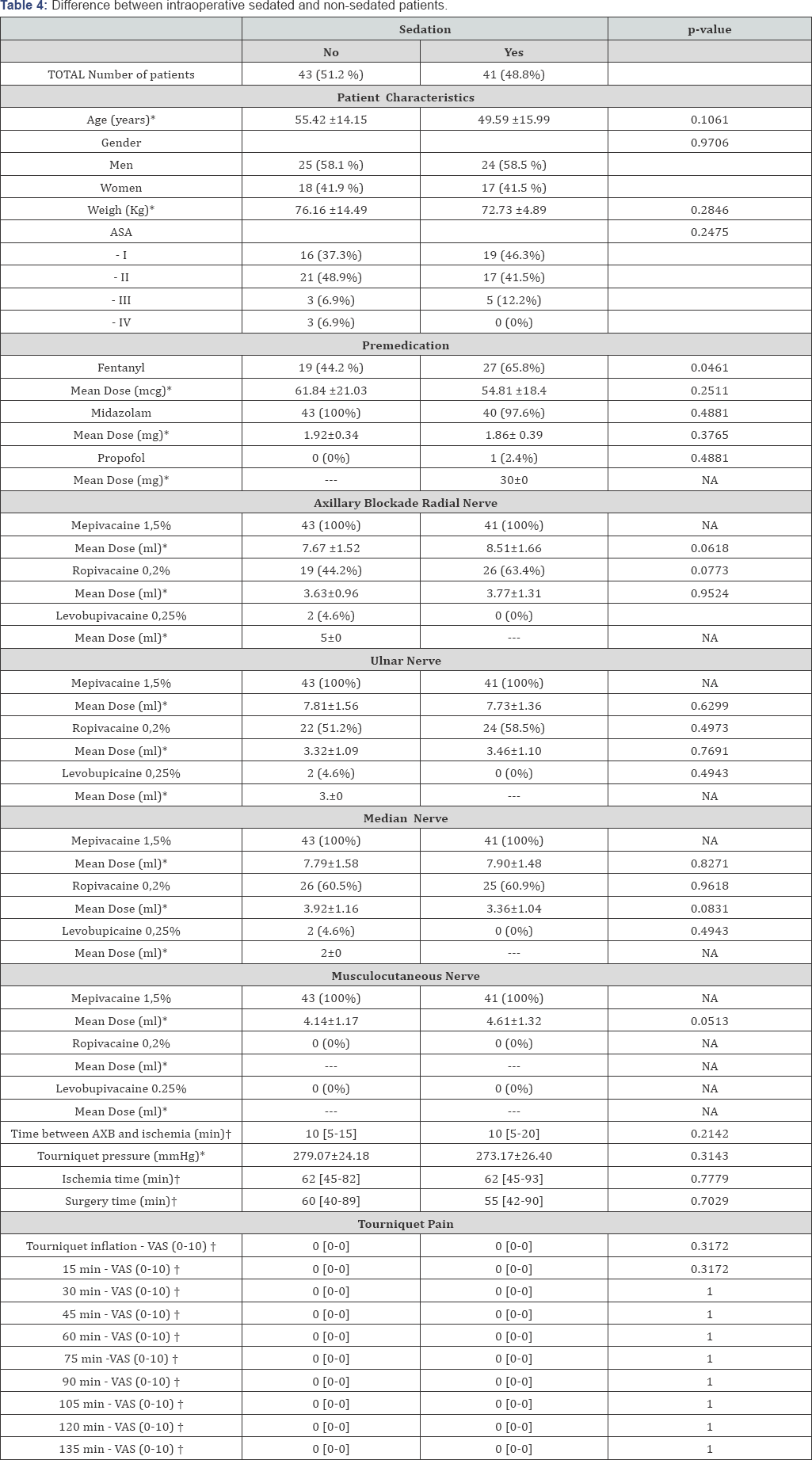
ASA: American Society of Anaesthesiologists; AXB: Axillary Block; VAS: Visual Analogue Scale;
Results shown as number of patients (%). *mean ± standard deviation (SD). †Median [Interquartile range = p25-p75]. NA = Not applicable. --- = Unknown.
Discussion
Tourniquets are commonly used in upper limb procedures to improve visualisation, reduce bleeding and expedite surgical procedures. Despite its advantages, tourniquet might associate injury that usually involves nerve or other soft tissues and is often complicated by the development of tourniquet pain [17]. Contrary to the old belief that a dermal component represents one of the major causes of tourniquet-related pain, ischemia and compression have been identified as the main sources of noxious stimuli during the maintenance of tourniquet inflation [18-21]. Due to these findings, there is progressively more belief that during AXB a tourniquet is well tolerable without requiring additional dermal anaesthesia [15,16]. Similarly, popliteal blockade is sufficient for tourniquet on the caff with no need of femoral or saphenous block [22]. It is important to highlight the importance of achieving a "complete" AXB [23]. Pain associated to tourniquet has been showed to be significantly reduced when a multiple injection AXB technique is used [24]. S. Sia et al. [25] comparing a triple injection AXB technique (blockade of median, musculocutaneous and radial nerves) and a "selective" approach in which only the nerves involved in surgery were blocked, reported a significant increase of patient requesting intraoperative administration of fentanyl for tourniquet pain in the "selective" group.
Despite the numerous anatomical variations of the four main nerves at the axilla, median, ulnar and radial nerves they all lie very close to the axillary artery [25]. Due to this proximity, the injection of a determinate amount of LA to block one of them could cause blockage of the others. By contrast, musculocutaneous nerve lies far lateral to the axillary artery, in the fascial plane between biceps brachii and coracobrachialis muscle. It innervates the muscles in the anterior compartment of the arm - the coracobrachialis, biceps brachii and the brachialis. To achieve its block the needle has to be redirected but its blockade is essential to prevent tourniquet pain [26]. We identified the four nerves by scanning distally along the arm and observing the nerve tracing. They were surrounded by LA independently. Among 84 patients, 83 reported "no pain" [27]. Only one patient complained about tourniquet discomfort (VAS= 3cm) during the first 15 minutes but VAS dropped to 0 cm from then on. This is more likely to be attributed to a block in progress than to a real need of additional blocks. Time between block finished and cuff inflation was just 3 min in this patient whereas, Tran DQ, et al. [28] concluded that the mean onset time is 18.9 minutes when using 4 injections AXB and lidocaine 1.5% with epinephrine 5mcg/ml.
The use of sedation in regional anaesthesia has been shown to increase patient satisfaction and can also modify pain perception [28,29]. However, there were no differences in tourniquet pain between intraoperative sedated and nonsedated patients in our study.
Tourniquet pain has been related to the duration of inflation [18]. Five of our patients had ischemia for more than 120min but none of them complained about tourniquet pain. JP Estebe et al. [30], reported a tourniquet pain tolerance of approximately 2030 minutes in volunteers. Tolerance was defined in that study when VAS was > 6cm or when volunteers decided their pain tolerance limit was reached. In daily practice, letting patients reach either points is unacceptable. Patients on the operating table suffering a painful experience could lead to anxiety, patient movement and unsuccessful surgery. Therefore if a tourniquet is required for surgery, associated pain should always be prevented and treated.
Fitzgibbons PG et al. [31] carried out a review regarding safe tourniquet use recommended tourniquet pressure of 250mmHg for less than 150min in the upper extremity. We used tourniquet pressure slightly higher and only one patient exceeded a total ischemia time of 150min, however a reperfusion time was used on this patient. Although higher pressures and longer ischemia times than the ones recommended have not demonstrated increased complication [32], tourniquet-related injury resulting from excessive tourniquet inflation pressure or prolonged ischemic time were not an objective of our study and were not followed up. Some of the limitations of this study included a relatively small number of patients, observational methodology and nonrandomized design. Test of sensory and motor blockade were not recorded, but no incomplete blocks were reported. No blinded observer data was collected. Ultrasound guided AXB alone provides enough anaesthesia to cover tourniquet-related pain even during prolonged ischemia. Use of additional dermal blocks are not required, however a multiple injection AXB technique that ensures musculocutaneous blockade should be performed.
References
- McCartney CJ, Brull R, Chan VW, Katz J, Abbas S, et al. (2004) Early but no long-term benefit of regional compared with general anesthesia for ambulatory hand surgery. Anesthesiology 101(2): 461-467.
- Neal JM, Gerancher JC, Hebl JR, Ilfeld BM, McCartney CJ, et al. (2009) Upper extremity regional anesthesia. Essentials of our current understanding, 2008. Reg Anesth Pain Med 34(2): 134-170.
- Lin E, Cho J, Hadzic A (2013) Peripheral nerve blocks for outpatient surgery: evidence-based indications. Curr Opin Anaesthsiol 26(4): 467-474.
- Tran DQH, Russo G, Munoz L, Zaouter C, Finlayson RJ (2009) A prospective, randomized comparison between ultrasound-guided supraclavicular, infraclaviclar, and axillary brachial plexus blocks. Reg Anesth Pain Med 34(4): 366-371.
- Perlas A, Lobo G, Lo N, Brull R, Chan VW, et al. (2009) Ultrasound- guided supraclavicular block: outcome of 510 consecutive cases. Reg Anesth Pain Med 34(2): 171-176.
- Gauss A, Tugtekin I, Georgieff M, Dinse-Lambracht A, Keipke D, et al. (2014) Incidence of clinically symptomatic pneumothorax in ultrasound-guided infraclavicular and supraclavicular brachial plexus block. Anaesthesia 69(4): 327-336.
- Marhofer P, Schrogendorfer K, Koinig H, Kapral S, Weinstabl C, et al. (1997) Ultrasonographic guidance improves sensory block and onset time of three-in-one blocks. Anaesth Analg 85(4): 854-857.
- Williams SR, Chovinard P, Arcand G, Harris P, Ruel M, et al. (2003) Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg 97(5): 1518-1523.
- Eichenberger U, Stockli S, Marhofer P, Huber G, Willimann P, et al. (2009) Minimal local anesthetic volume for peripheral nerve block: a new ultrasound-guided nerve dimension based method. Reg Anesth Pain Med 34(3): 242-246.
- Kubota Y, Koizumi T, Udagawa A, Kuroki T (2008) Prevention of tourniquet pain by subcutaneous injection into the posterior half of the axilla. J Plast Reconstr Aesthet Surg 61(5): 595-597.
- Tschaikowsky K, Hemmerling T (1998) Comparison of the effect of EMLA and semicircular subcutaneous anaesthesia in the prevention of tourniquet pain during plexus block anaesthesia of the arm. Anaesthesia 53(4): 390-393
- Winnie A (1983) Plexus Anesthesia. Philadelphia: WB Saunders.
- Henderson JJ, Nimmo WS (1983) Practical regional Anaesthesia. Oxford: Backwell Scientic Publications.
- Rousso M, Wexler MR, Weinberg H, Vatashky E, Aronson B (1978) Subcutaneous ring anesthesia in the prevention of tourniquet pain in hand surgery. Hand 10(3): 317-320.
- Johr M, Balogh S (1998) Tourniquet pain during brachial plexus block. Anaesthesia 53(8): 828.
- Ranganath A, Srinivasan KK, Iohom G (2014) Ultrasound guided axillary brachial plexus block. Med Ultrason16(3): 246-251.
- Estebe JP, Davies JM, Richebe P (2011) The pneumatic tourniquet: mechanical, ischaemia-reperfusion and systemic effects. Eur J Anaesthesiol 28(6): 404-411.
- Hagenouw RRPM, Bridenbaugh PO, van Egmond J, Stuebing R (1986) Tourniquet pain: a volunteer study. Anesth Analg 65: 1175-1180.
- Crew JC, Cahall MA (1999) An investigation of the neurophysiologic mechanisms of tourniquet-related pain: changes in spontaneous activity and receptive field size in spinal dorsal horn neurons. Reg Anesth Pain Med 24(2): 102-109.
- Tetzlaff JE, Yoon HJ, Walsh M (1993) Regional anaesthetic technique and the incidence of tourniquet pain. Can J Anaesth 40(7): 591-595.
- Cole F (1952) Tourniquet pain. Anesth Analg 31: 64-65.
- Palacios ME, Rufino J, Santiago FM, Rodri'guez-Banqueri M, Gallego RJ, et al. (2005) Sciatic blockade at the level of the popliteal fossa. Comparison between two approaches. Rev Soc Esp Dolor 12: 264-268.
- Chin KJ, Alakkad H, Cubillos JE (2013) Single, double or multiple- injection techniques for non-ultrasound guided axillary brachial plexus block in adults undergoing surgery of the lower arm. Cochrane Database Syst Rev 8: CD003842.?
- Sia S, Lepri A, Marchi M (2010) Axillary Block by "Selective" Injections at the Nerves involved in Surgery Using a Peripheral Nerve Stimulator A Comparison With a "Standard" Triple-Injection Technique. Reg Anesth Pain Med 35(1): 22-27.
- Silva MG, Sala-Blanch X, Marin R, Espinoza X, Arauz A, et al. (2014) Ultrasound-guided axillary block: Anatomical variations of terminal branches of the brachial plexus in relation to the brachial artery. Rev Esp Anestesiol Reanim 61(1):15-20.
- Soodan A, Ahmad I (2010) Is a selective brachial plexus block at the axilla possible when using a nerve stimulator and large volumes of local anesthetic?. Reg Anesth Pain Med 35(5): 475-476.
- Tran DQ, Pham K, Dugani S, Finlayson RJ (2012) A Prospective, Randomized Comparison Between Double-, Triple-, and Quadruple- Injection Ultrasound-Guided Axillary Brachial Plexus Block. Reg Anesth Pain Med 37(3): 248-253.
- Wu CL, Naqibuddin M, Fleisher LA (2001) Measurement of patient satisfaction as an outcome of regional anesthesia and analgesia: a systematic review. Reg Anesth Pain Med 26(3):196-208.
- Frolich MA, Zhang K, Ness TJ (2013) Effect of sedation on pain perception. Anesthesiology 118(3): 611-621.
- Estebe JP, Le Naoures A, Chemaly L, Ecoffey C (2000) Tourniquet pain in a volunteer study: effect of changes in cuff width and pressure. Anaesthesia 55(1): 21-26.
- Fitzgibbons PG, DiGiovanni C, Hares S, Akelman E (2012) Safe tourniquet use: a review of the evidence. J Am Acad Orthop Surg 20(5): 310-319.
- Drolet BC, Okhah Z, Phillips BZ, Christian BP, Akelman E (2014) Evidence for safe tourniquet use in 500 consecutive upper extremity procedures. Hand 9(4): 494-498.