Remifentanil-Induced Respiratory Failure in PACU after a Brainstem Tumor Debulking: Acute Diagnostic Dilemma
Laura Duling, Annette Rebel, Jonathan Bain, Jeremy Dority*
University of Kentucky College of Medicine, USA
Submission: March 10, 2017; Published: September 15, 2017
*Corresponding author: Jeremy Dority MD, University of Kentucky College of Medicine, Chandler Medical Center N-202, 800 Rose Street, Lexington, KY 40536-0293; USA, Email: jsdori2@uky.edu
How to cite this article: Laura D, Annette R, Jonathan B, Jeremy D. Remifentanil-Induced Respiratory Failure in PACU after a Brainstem Tumor Debulking: Acute Diagnostic Dilemma. J Anest & Inten Care Med. 2017; 3(5) : 555623. DOI: 10.19080/JAICM.2017.03.555623
Abstract
A 66 year old man developed sudden apnea and unresponsiveness after a large cerebellopontine angle tumor debulking. Based on the findings of a focused neurologic exam, the patient was emergently mask ventilated with subsequent return of spontaneous ventilation minutes later and recovery without further complications. Remifentanil bolus from residual infusion in an IV line was suspected due to rapid return to baseline and acute neurologic findings. We review remifentanil and highlight a challenging diagnostic dilemma in an acutely apneic patient after major neurosurgery.
Keywords: Remifentanil; Neuroanesthesia; Post-op respiratory failure; Neurologic Emergencies
Key Messages
a. A focused neurologic exam can affect emergent management.
b. A high index of suspicion and staff education are necessary for those involved in the care of patients receiving remifentanil.
Introduction
Remifentanil is a potent, ultra short-acting μ-opioid receptor agonist with a rapid onset of action in 30-60 seconds, peak analgesic and respiratory effects within 2.5 minutes (min), and rapid clearance (T1/2 = 3 min) [1]. It is commonly used as part of a balanced anesthetic in many anesthesia practices as well as in the intensive care unit. Its use is particularly prominent in neuroanesthesia, where precise hemodynamic control is as important as a crisp, quick emergence of anesthesia to facilitate neurologic evaluation. Respiratory depression is a common severe adverse effect of opioids that may be most prevalent with remifentanil [2].
Case History
A 66 year old man with a large acoustic neuroma presented for cerebellopontine (CP) angle tumor resection (Figure 1). Neuromonitoring of cranial nerves IX, X, XI, XII, somatosensory evoked potentials and motor evoked potentials was used during the case, while the patient received an intravenous anesthetic consisting of propofol 100mcg/kg/min and remifentanil at 0.3mcg/kg/min. Neuromuscular blockade was not used for the case. The surgery progressed without complication, and thepatient was stable throughout. The case lasted 7.5 hours, and propofol and remifentanil were discontinued 60min and 15min prior to conclusion of case, respectively. The patient was able to spontaneously ventilate, protrude tongue, and demonstrate intact cranial nerves IX and X with gag reflex prior to extubation.

In the PACU, the patient was awake and following commands. Shortly after administration of flush through a secondary peripheral IV, the patient acutely closed his eyes, becoming unresponsive and apneic. Rapid physical exam to check for increased intracranial pressure given the setting of recent intracranial surgery demonstrated the patient's pupils were actually pinpoint. The patient was then mask-ventilated until spontaneous ventilation returned several minutes later. Pinpoint pupils and rapid recovery makes a remifentanil bolus from residual infusion in the second IV line the most likely etiology. Patient recovered without further difficulty and was discharged home 3 days later.
Discussion
Remifentanil review
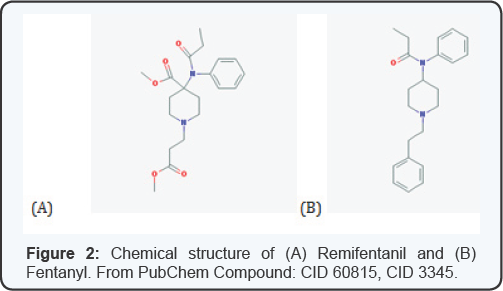
Remifentanil is a potent selective μ-opioid agonist. Its major distinction from other fentanyl analogues is its rapid onset and short duration of action with a terminal elimination half-life of 3-10 min, usually negating the need for Naloxone reversal [3]. The rapid onset of action is directly related to the rapid blood brain equilibration time of 1-2 minutes, while the short duration of action is a result of its unique structure of ester linkages making it susceptible to hydrolysis by blood and non-specific esterases (Figure 2). This rapid extra-hepatic metabolism makes its pharmacokinetics reproducible and dependable. Time to spontaneous movement, following commands, and extubation are all shorter than when compared with other opioids such as fentanyl and morphine. These pharmacokinetic and pharmacodynamic characteristics make remifentanil a nearly ideal analgesic in the operating room. However, due to its short duration of action, patients receiving remifentanil frequently require rescue analgesia in the postoperative period for pain management [4].
Remifentanil is rapidly metabolized regardless of the duration of infusion and is used commonly in clinical situations requiring a rapid offset with the benefit of minimal side effects such as respiratory depression [5]. While the risk for respiratory depression still exists, the ability to rapidly titrate the drug based on response allows for an overall lower rate when compared to most other opioids. In neuroanesthetic cases, it is commonly used in conjunction with propofolas part of a total intravenous anesthetic. It is easily titratable, facilitates stable hemodynamics, and minimally affects neuro-monitoring. Perhaps most importantly, this total intravenous anesthesia combination can allow for rapid emergence and the ability to perform post-operative examination for neurological status shortly after conclusion of the case [2].
Clinical experience
Rapid bolus of remifentanil can result in potentially life threatening respiratory depression, hemodynamic changes, or muscle rigidity. Respiratory depression has been documented in case reports after bolus in laboring patients with patient controlled analgesia [6] as well as in non-obstetric patients receiving remifentanil [7]. This appears to be even more pronounced and observed at lower doses in patients greater than 60 years old. Even infusions as low as 0.05mcg/kg/min have been reported to cause changes in ventilatory drive in healthy volunteers. Muscle rigidity, likewise, is a concerning complication of opioids that can lead to decreased ventilation and compliance resulting in hypoxia and hypercapnia. It is suggested that difficult ventilation may be primarily due to vocal cord closure. Remifentanil, however, primarily affects respiratory drive by activating opioid receptors on the respiratory neurons in the brainstem. By depressing the respiratory drive, the arterial carbon dioxide not only increases but increases in oxygen consumption and intracranial pressure are to be expected [8]. Muscle rigidity however can be prevented with pretreatment or concurrent administration of neuromuscular blockade [9].
Apnea
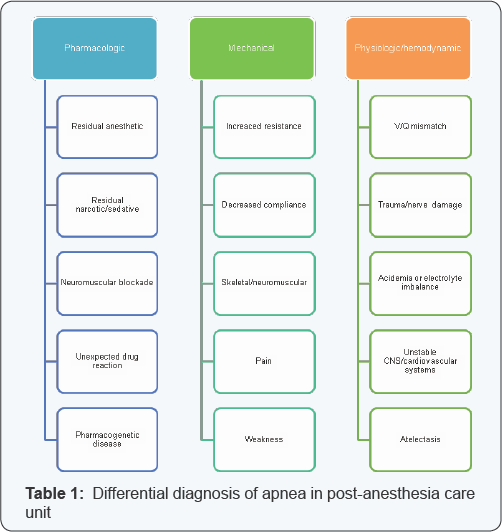
Our case brings up the challenge and importance of differentiating causes of sudden apnea and mental status change in the immediate post-operative period. The differential for postoperative respiratory failure is large and includes pharmacologic, hemodynamic and mechanical causes (Table 1). In addition to those listed, the patient's comorbidities may be one of the most fundamental things to consider. In the setting of recent intracranial surgery, both opioid overdose and intracranial pathology and dysfunction such as increasing intracranial pressure and seizures are important considerations. Cerebellopontine angle procedures are technically challenging and carry significant risk for postoperative bleeding, increasing intracranial pressure, venous insufficiency and cranial nerve palsy. Physical exam, including neurological exam, may be the most useful and potentially life-saving in this case.
Prevention
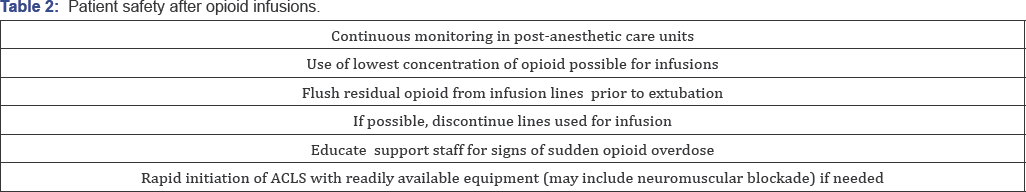
Prevention is a keystone of patient care, and the use of more dilute concentrations of remifentanil and initiating rapid resuscitation with possible muscle relaxation have been identified as ways to decrease the chance of similar events from occurring (Table 2). Remifentanil is a very useful opioid in a variety of settings for controlling autonomic responses during procedures and allowing for rapid recovery [2,5]. However, its dangers as a bolus should be known to healthcare providers and ancillary staff so appropriate identification and supportive care can be initiated as soon as a problem is identified.
Acknowledgement
Special thanks to Damian Pickering for assistance with manuscript preparation.
References
- Babenco HD, Conard PF, Gross JB (2000) The pharmacodynamic effect of a remifentanil bolus on ventilatory control. Anesthesiology 92(2): 393-398.
- Dahan A, Aarts L, Smith TW (2010) Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology 112(1): 226-238.
- Gesztesi Z, Mootz BL, White PF (1999) The use of a remifentanil infusion for hemodynamic control during intracranial surgery. Anesth Analg 89(5): 1282-1287.
- Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, et al. (2007) Remifentanil for general anaesthesia: a systematic review.This work is licensed under Creative Commons Attribution 4.0 License D0I:10.19080/JAICM.2017.03.555623Anaesthesia 62(12): 1266-1280.
- Hogue CW, Bowdle TA, O'Leary C, Duncalf D, Miguel R, et al. (1996) A multicenter evaluation of total intravenous anesthesia with remifentanil and propofol for elective inpatient surgery. Anesth Analg 83(2): 279-285.
- Bonner JC, McClymont W (2012) Respiratory arrest in an obstetric patient using remifentanil patient-controlled analgesia. Anaesthesia 67(5): 538-540.
- Shaikh N, Hanssens Y, Louon A (2011) Remifentanil apnea: Case report and review of the literature. J Anaesthesiol Clin Pharmacol 27(4): 553555.
- Fukuda K. Opioids (2005) In: Miller (ed.), Miller's Anesthesia 781.
- Nakada J, Nishira M, Hosoda R, , Funaki K, Takahashi S, et al. (2009) Priming with rocuronium or vecuronium prevents remifentanil- mediated muscle rigidity and difficult ventilation. J Anesth 23(3): 323328.






























