Effect of Intraoperative Anesthetic Management on Patient Outcomes for Surgical Revascularization for Moyamoya Disease: A 7-year Retrospective Study
George WW1*, Rabail C2, Chunyan C3, Greesha SP4, William J5, Shilpa D2, Alia L2, Carlos AA2, Robert CW2, Navneet KG2, Naveen MK2 and Lara F2
1Department of Anesthesiology and Neurosurgery, University of Texas Health Science Center, USA
2Department of Anesthesiology, University of Texas Health Science Center, USA
3Clinical and Translational Sciences, University of Texas Health Science Center, USA
4Trainee, Department of Anesthesiology, University of Texas Health Science Center, USA
5McGovern Medical School, University of Texas Health Science Center, USA
Submission: March 17, 2017; Published: August 28, 2017
*Corresponding author: George W. Williams, MD, FCCP, Department of Anesthesiology and Neurosurgery, University of Texas Health Science Center, 6431 Fannin Street, MSB 5.020, Houston, Texas USA 77030-1501, USA, Tel: (713)500-6680; Fax: (713)500-0528; Email: George W. Williams@uthtmc.edu
How to cite this article: George WW, Rabail C, Chunyan C, Greesha SP, William J, et al. Effect of Intraoperative Anesthetic Management on Patient Outcomes for Surgical Revascularization for Moyamoya Disease: A 7-year Retrospective Study. J Anest & Inten Care Med. 2017; 3(4) : 555617. DOI: 10.19080/JAICM.2017.03.555617
Abstract
Study objective: The anesthetic management of a patient with MMD presents a challenge to the anesthesiologist as it may affect the prevalence of further complications of the disease. We hypothesize that anesthetic management significantly affects the long term neurological outcome in patients with MMD and an ideal anesthetic will reduce the length of stay.
Study design: Retrospective cohort study
Patients: We performed a retrospective review of 32 patients with MMD who underwent craniotomy and surgical revascularization. The data was divided into two equal case cohorts based on two equal time periods. Measurements: Data was collected on usage of anesthetic agents such as fentanyl, propofol, remifentanil, isoflurane, sevoflurane and desflurane. Patient length of stay and adverse events that were associated with each case were also noted.
Results: Remifentanil use increased significantly over the two periods. In contrast, patients that received desflurane had a significantly shorter mean length of stay when compared to patients who did not receive desflurane. Interestingly, there was a decrease in the mean length of stay between the first and second periods of 3.9 and 3.3 days respectively, albeit statistically insignificant.
Conclusion: Use of desflurane in Moyamoya patients undergoing revascularization was associated with a decrease length of stay, while the use of sevoflurane was associated with an increased length of stay. Use of remifentanil has expanded in recent years, which may be attributable to its shorter duration of action and ability to maintain hemodynamic during the induction, maintenance, and emergence of anesthesia with rapid postoperative recovery.
Keywords: Moyamoya disease; Neurosurgical revascularization; Sevoflurane; Remifentanil; Length of stay
Introduction
Moyamoya disease (MMD) is a rare idiopathic cerebrovascular condition characterized by progressive stenosis of the supraclinoid internal carotid arteries, either unilaterally or bilaterally [1,2]. MMD is an autosomal dominant hereditary disorder with a mutation of q25.3 on chromosome 17. It has a prevalence of 3.16 and incidence of 0.35 cases per 100,000 people, with a female-to-male ratio of 1.8:1 [3-5]. MMD is more frequently seen in the Asian population but has been described sporadically in other parts of the world.6 Prior studies show that MMD can be associated with other diseases including thyrotoxicosis, sickle cell anemia, Down's syndrome, coarctation of the aorta, and hypertension, all of which warrant consideration due to implications for anesthetic management [6].
In MMD, there is angiographic evidence of progressive stenosis or occlusion of the terminal portions of the internal carotid arteries and the proximal part of the anterior and middle cerebral arteries; the posterior cerebral arteries are less frequently involved. The formation of reticular anastomoses and collaterals between the internal and external carotid arteries gives the image of a "puff of smoke" on angiogram[2,7]. In pediatric patients with MMD, the first symptom is often a stroke or transient ischemic attack (TIA), muscular weakness, paralysis, or seizures.1 In Caucasian patients, MMD is seen most commonly in adults and usually presents with either headaches or stroke (ischemic or hemorrhagic). 1 Hemodynamic changes are significant throughout the preoperative period, and MMD patients require intensive care management. Hypertension can potentially cause intracranial hemorrhage, and hypotension or hyperventilation can result in cerebral ischemia [8,9]. Proper knowledge of the path physiology and institution of optimal preoperative measures improves intra operative variables as well as long-term patient outcomes [6].
The principles of safe anesthesia such as norm tension, normocarbia, adequate oxygenation, normothermia, and normovolemia apply to patients with MMD.9 During craniotomy procedures, certain deviations from these principles are indicated (i.e. hyperventilation and mannitol diuresis for brain volume reduction) but can be safely performed with careful monitoring [10]. Anesthetic management of patients with MMD focuses on maintaining adequate cerebral blood flow, normalization of intracranial pressure, and avoidance of both cerebral vasoconstriction and vasodilatation [11]. The anesthetic management of a patient with MMD presents a challenge to the anesthesiologist as it may affect the prevalence of further complications of the disease. We hypothesize that anesthetic management significantly affects the long-term neurological outcome in patients with MMD and an ideal anesthetic plan will reduce the patient's overall length of stay. Given the growing body of literature describing the safe and efficacious operative treatment of MMD, anesthesiologists are likely to encounter more of such patients in the future and hence, need to be aware of the surgical techniques and the impact of the anesthetic management on patient outcomes.
Materials and Methods
We performed a retrospective review of all MMD cases from 01/01/2009 to 12/31/2015 at Memorial Hermann Hospital, Texas Medical Center in which intra operative management involved a craniotomy and surgical revascularization. Due to the rarity of MMD, it was statistically not possible to analyze the data by year. Therefore, the data was divided into two equal case cohorts: the first 16 revascularization cases were included in the 01/01/2009 to 02/18/2013 date range and the second 16 cases were included in the 02/19/2013 to 12/31/2015 date range.
Adult patients with operative interventions occurring both emergently (e.g. after neurologic deterioration in a patient with MMD) and semi-electively (e.g. before anticipated neurologic deterioration in a patient with evidence of MMD) were included. Excluded from the analysis, were patients with a previous disabling neurological disease or the presence of a terminal illness that may have affected postoperative mortality.
Data was primarily collected on the usage of several anesthetic agents such as fentanyl, propofol, remifentanil, isoflurane, sevoflurane and desflurane. An anesthetic was considered pertinent if it was used throughout the duration of the revascularization procedure and was not considered pertinent if it was only administered at the beginning or end of the procedure. Patient length of stay and any adverse events that were associated with each case were also noted.
Results
We analyzed 32 cases of Moyamoya revascularization surgery over a period of 6 years from 01/01/2009 to 12/31/2015. Table 1 shows the comparison of anesthetic agents and gasses used between the two periods. The use of fentanyl, propofol, isoflurane, desflurane and sevoflurane between the two periods did not vary significantly. However, the use of remifentanil increased significantly from 18.8% (n=3) to 93.8% (n=15) over the two periods (p < 0.0001).
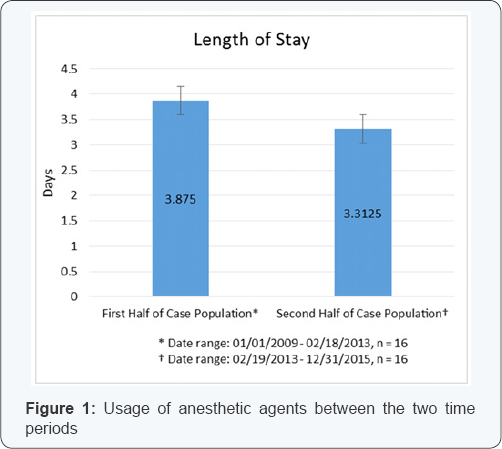
Similar increased use was observed for desflurane. During the first period, 87.5% of the patients received desflurane. However, 100% of the patients received desflurane during the second period. Figure 1 gives a graphical representation of the changing trends of use of all anesthetic agents. Interestingly, there was a decrease in the mean length of stay between the first and second periods of 3.9 and 3.3 days respectively, albeit it was statistically insignificant (p = 0.1642) (Table 1 & Figure 2).
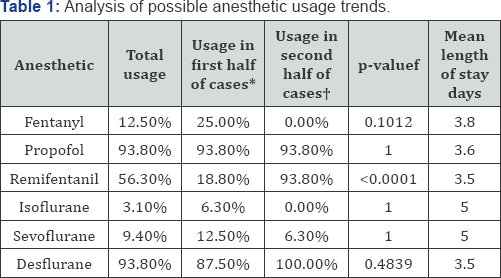
*Date range: 01/01/2009 - 02/18/2013, n =16; †Date range: 02/19/2013 - 12/31/2015, n =16; f Obtained by extended Fisher's exact test
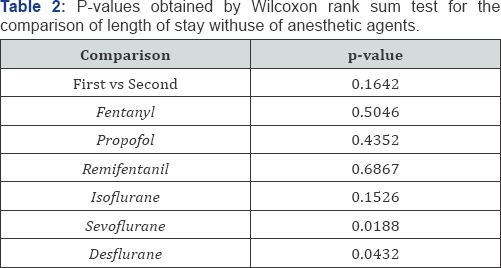
When comparing the length of stay with use of different anesthetic agents (Table 2), the use of fentanyl, propofol, remifentanil and isoflurane (p values 0.5046, 0.4352, 0.6867 and 0.1526 respectively) did not affect the average length of stay (Table 2). However, the use of sevoflurane and desflurane did correlate with differences in the length of stay (p values 0.0188 and 0.0432 respectively) (Table 2). Patients that received sevoflurane had a mean length of stay of 5 days, while the ones that did not receive sevoflurane had a mean length of stay of 3.4 days (p = 0.0188). In contrast, patients that received desflurane had a significantly shorter mean length of stay of 3.5 days when compared to patients that did not receive desflurane, who had an average length of stay of 5 days (p = 0.0432)
Discussion
Moyamoya disease is a rare neurovascular disorder that requires special anesthetic management during revascularization. Given the chronic nature of cerebral ischemia and the debilitating course of MMD, various cerebral revascularization procedures have been proposed to augment collateral cerebral blood flow. Although several noninvasive diagnostic techniques have been developed, medical treatment has been challenging, and the anesthetic management is still evolving [12].
This retrospective study analyzed the anesthetic management of 32 patients suffering from Moyamoya disease that underwent revascularization procedures over a six year period. Neurosurgery requires balanced anesthesia utilizing volatile or intravenous anesthetic agents coupled with good analgesics. Volatile anesthetic agents cause cerebral vasodilatation which may result in cerebral steal syndrome [14]. The use of propofol may suppress cerebral metabolism and cause a decrease in cerebral blood flow [15, 16]. The cerebral effects of opioids which may result in a modest reduction in the cerebral metabolic rate and intracranial pressure are dependent on systemic hemodynamic, concomitant use of other anesthetic agents, and underlying co morbidities. However, opioids are potent analgesics and are beneficial in stabilizing the hemodynamic. Therefore, they are not contraindicated for patients with cerebral diseases and compromised intracranial compliance [17].
In our study, we observed the trends in the usage of various anesthetic agents over a six year period along with the duration of hospital stay. The use of anesthetic agents and gasses like fentanyl, propofol, isoflurane, desflurane and sevoflurane between the two periods did not vary significantly. However, the use of remifentanil increased substantially during the second half of the period that was reviewed. Balakrishnan et al. [18] observed that remifentanil was found to provide stable hemodynamic during induction, maintenance, and emergence when compared with fentanyl.18 Another interesting observation was decreased use of isoflurane when used concomitantly with remifentanil. Twersky et al. [19] reported lower systolic and diastolic blood pressures and heart rates in patients that were administered remifentanil as compared to fentanyl. These hemodynamic variants may explain the growing popularity of remifentanil [19].
We also observed that the length of hospital stay in patients that were administered desflurane was significantly shorter in the second period. On the other hand, patients in the second period that received sevoflurane had an increased length of stay. A study by Magni et al. [20] showed that patients who received desflurane had shorter extubation and recovery times as compared with those who received sevoflurane. This may explain the distribution of the length of stay observed in this study.
One of the major limitations of this study is the limited sample size which can be attributed to the rarity of the disease. Additionally, we were unable to analyze postoperative complications and outcomes due to limited access to patient outcomes data. However, our study raises interesting questions regarding the effect of anesthetic agents and their effect on patient outcomes and suggests the need for additional studies to analyze the relationship between anesthetic management and perioperative outcomes along with long-term morbidity and mortality in this vulnerable population.
Conclusion
Use of desflurane in Moyamoya patients undergoing revascularization was associated with a decrease length of stay, while the use of sevoflurane was associated with an increased length of stay. Use of remifentanil has expanded in recent years, which may be attributable to its shorter duration of action and ability to maintain hemodynamic during the induction, maintenance, and emergence of anesthesia with rapid postoperative recovery.
References
- Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360(12): 1226-1237.
- Suzuki J, Takaku A (1969) cerebrovascular "moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20(3): 288-299.
- Mineharu Y, Takenaka K, Yamakawa H, Inoue K, Ikeda H, et al. (2006) Inheritance pattern of familial moyamoya disease: autosomal dominant mode and genomic imprinting. J Neurol Neurosurg Psychiatry 77(9): 1025-1029.
- Mineharu Y, Liu W, Inoue K, Ikeda H, Takenaka K, et al. (2008) Autosomal dominant moyamoya disease maps to chromosome 17q25.3. Neurology Jun 70(24 Pt 2): 2357-2363.
- Wakai K, Tamakoshi A, Ikezaki K, Fukui M, Kawamura T, et al. (1997) Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey. Clin Neurol Neurosurg 99(suppl2): S1-S5.
- Dutta B, Dehran M, Sinha R (2011) Anaesthetic management of a parturient with moyamoya disease. Singapore Med J 52(6): e108-110.
- RC Bacon, PA Razis (1994) The effect of propofol sedation in pregnancy on neonatal condition. Anaesthesia 49(12): 1058-1060.
- Sharma SK, Wallace DH, Sidaiwi JE, Gambling DR (1994) Obstetric anaesthesia and moyamoya disease. Can J Anaesth 41(8): 756-757.
- B Venkatesh, Taggart PC (1994) Anaesthetic management of a patient with Moyamoya disease for Caesarean section. Can J Anaesth 41(1): 79-80.
- Chong CT, Manninen PH (2011) Anesthesia for cerebral revascularization for adult moyamoya syndrome associated with sickle cell disease. J Clin Neurosci 18(12): 1709-1712.
- Petty LA (1993] Anesthetic management of a patient with moyamoya disease: a case report. AANA J 6l(3): 277-28l.
- Parray T, Martin TW, Siddiqui S (2Oll) Moyamoya disease: a review of the disease and the anesthetic management. J Neurosurg Anesthesiol 23(2]: 100-109.
- Pandey P, Steinberg GK (2Oll) Neurosurgical advances in the treatment of moyamoya disease. Stroke 42(ll): 33O4-33lO.
- Sato K, Shirane R, Kato M (1999] Effect of inhalation anesthesia on cerebral circulation in Moyamoya disease. J Neurosurg Anesthesiol ll(l): 25-3O.
- Adachi K, Yasamoto Y, Kameyama E, Hirotoshi S, Takashi H, et al. (2OO5) Early postoperative complications with Moyamoya disease. A comparison of inhaled anesthesia with total intravenous anesthesia (TIVA). Masui 54(6): 653-657.
- Ilkhchoi Y, Panikkath PV, Martin H (2Ol4) Moyamoya disease, revascularization surgery and anesthetic considerations. BMJ Case Rep.
- Schregel W, Weyerer W, Cunitz G (1994] Opioids cerebral circulation and intracranial pressure. Anaesthethist 43(7): 42l-43O.
- Balakrishnan G, Raudzens P, Samra S, Song K, Boening JA, et al. (2OOO) A comparison of remifentanil and fentanyl in Patients undergoing surgery for intracranial mass lesions. Anesth Analg 91(1]: 163-169.
- Twersky RS, Jamerson B, Warner D, Fleisher LA, Hogue S, et al. (2001] Hemodynamics and Emergence Profile of Remifentanil versus Fentanyl Prospectively Compared in a Large Population of Surgical Patients. J Clin Anesth l3(6): 4O7-4l6.
- Magni G, Rosa IL, Melilo G, Savio A, Rosa G, et al. (2009] A Comparison between Sevoflurane and Desflurane Anesthesia in Patients Undergoing Craniotomy for Supratentorial Intracranial Surgery. Anesth Analg 109(2]: 567-571.






























