Using Ultrasound to Confirm Endotracheal Tube Position in the Intensive Care Unit
Rahul Khosla1, Cara Kistler2 and Ahmad Alwassia3*
1Department of pulmonary and critical care, Veteran Affairs Medical Center, USA
2Department of pulmonary and critical care, Charlotte Medical Clinic, USA
Submission: September 20, 2016; Published: October 06, 2016
*Corresponding author: Ahmad Alwassia, 2300 Eye Street, Washington, DC 20037, department of pulmonary and critical care Veteran Affairs Medical Center, George Washington University Hospital, Irving street, Washington, DC 20422, USA, Tel:3058904672 Email:alwassia5@gmail.com
How to cite this article: Rahul K, Cara K, Ahmad A. Using Ultrasound to Confirm Endotracheal Tube Position in the Intensive Care Unit. J Anest & Inten Care Med. 2016; 1(2) : 555560. DOI: 10.19080/JAICM.2016.01.555560
Abstract
Aim: To determine the accuracy of ultrasound in confirming endotracheal tube placement compared with standard techniques in the intensive care unit.
Subject and Methods:: This was a prospectively designed study. Eligible patients were 18 years or older, that were admitted to the medical intensive care unit, that required endotracheal intubation due to their underlying clinical condition. An immediate post intubation Ultrasound examination was performed by an intensivist, who was not involved in clinical management of the patient and was blinded to the result of the standard confirmatory methods of endotracheal tube placement. The clinician performing the intubation was blinded to the results of the ultrasound examination findings.
Results:: According to the standard method used to confirm proper endotracheal tube position, which includes clinical assessment by chest and epigastric auscultation, and a colometric end tidal CO2 connected to the endotracheal tube, all twenty patients had a correctly placed endotracheal tube; however, the post-intubation chest radiograph showed a right main stem intubation in one patient that was missed by the standard method of confirmation. Ultrasound examination confirmed the proper placement of the endotracheal tube in 19 patients, and was also able to detect the right main stem intubation in that one patient. Based on the results of our study, the diagnostic accuracy of the ultrasound method in confirming proper endotracheal tube position was 100% (20/20) and that of the standard method 95% (19/20).
Conclusion: This study demonstrates that US imaging has a high diagnostic accuracy to immediately confirm proper ETT placement post-intubation in an intensive care unit.
Keywords: Ultrasound (US); Endotracheal tube (ETT) position; Intensive care; End tidal CO2; Chest radiograph
Abbreviations: US: Ultrasound; ETT: Endotracheal Tube; ICU: Intensive Care Unit; AHA: American Heart Association
Introduction
It is important to confirm proper placement of the endotracheal tube (ETT) as there is significant morbidity and mortality associated with inadvertent esophageal intubation [1-3]. Endotracheal intubation is a frequently performed procedure in an intensive care unit (ICU) and an intensivist has to be adept at performing intubation and confirming ETT position [4]. An ideal technique to confirm the position of ETT is one that provides verification of tracheal location of the ETT at a level above the carina to ensure bilateral ventilation. The 2010 American Heart Association (AHA) guidelines for adult advanced life support (ACLS) recommend the use of both clinical assessment and confirmation devices to verify ETT placement [3].
Visualizing chest expansion, auscultating bilateral lung fields and epigastrium, along with continuous waveform capnography is considered the most reliable method of confirming correct ETT placement. Besides waveform capnography there are other confirmatory devices, such as, no waveform exhaled carbon dioxide detectors, esophageal detector devices, and transthoracic impedance detectors. Direct visualization of the glottis and passing the ETT under direct vision is considered the gold standard, but in many patients with difficult airways, it may not be possible to visualize the glottis [5].
Despite all the numerous techniques described to confirm proper ETT placement, none of the methods are absolutely reliable, or readily available in many ICU’s [3,6]. Waveform capnography is unreliable in patients with low pulmonary blood flow, airway obstruction, low cardiac output states, and epinephrine use [6]. A routine practice in most ICU’s is to obtain post-intubation chest radiography to confirm the location of ETT above the carina [7]. Chest radiographs take time to be performed and are not very helpful for immediately confirming a proper position of the ETT.
With the rise in use of point-of-care ultrasound to assess patients in ICU’s, ultrasound machines are readily available in most ICU’s [8,9]. Sonographic confirmation of correct ETT position has been described in adults, with either direct visualization of the tracheal tube [10-14], indirect signs of ventilation, such as bilateral pleural sliding [15] and diaphragm motion [16-19] or both [20]. An ultrasound (US) examination can be performed immediately and rapidly after intubation, with great accuracy to confirm ETT position [21].
We conducted a pilot study with a goal to determine the feasibility of US to confirm ETT position immediately post intubation, prior to the chest radiograph. The study design was approved by the institutional review board (IRB), and a waiver for informed consent was obtained as an emergency situation made it infeasible to obtain the same.
Material and Methods
This was a prospective, double blinded, and single center pilot study conducted at our Medical Intensive Care Unit. Eligible patients were 18 years or older intubated emergently in the ICU due to their underlying clinical condition. Exclusion criteria included patients with subcutaneous emphysema, pneumothorax, a history of pneumonectomy and pleurodesis. US imaging for pleural sliding is not technically feasible in these patients, as the US waves tend to reflect strongly wherever air meets tissue secondary to high acoustic impedance.
An anesthesiologist or an intensivist performed the intubation and confirmed the proper position of the ETT using the standard method. All patients were sedated and paralyzed for intubation. The standard method in our ICU to assess proper ETT location immediately post-intubation includes the use of clinical assessment and a colometric end tidal CO2 (ETCO2) detecting device (Easy Cap II, Nellcor Inc., Hayward, CA). The ETCO2 detector connects to the end of the ETT and a persistent color change from purple to yellow after five breath cycles is accepted as a verification of correct placement of ETT. A chest radiograph is then performed and interpreted by the clinician who intubated the patient to confirm ETT’s location above the carina. An immediate post intubation US examination was performed by an intensivist, who was not involved in clinical management of the patient and was blinded to the result of the standard confirmatory methods of ETT placement, and the clinician performing the intubation was blinded to the US examination findings.
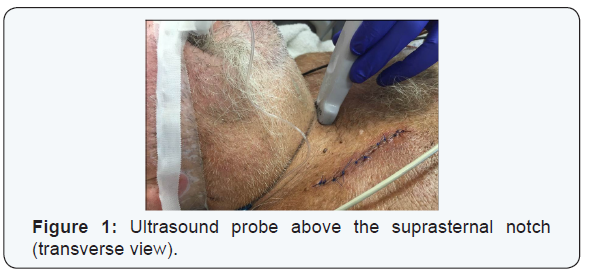
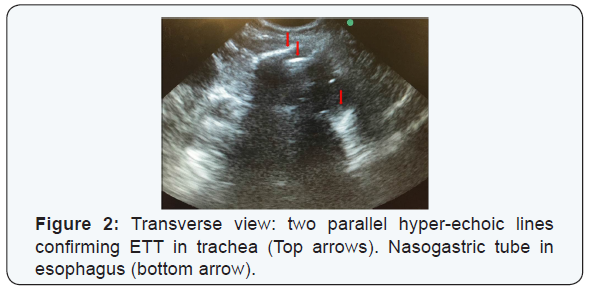
US images were obtained using MicroMaxx (Sonosite Inc., Bothell, WA) machine with a 5-8 MHz curved array transducer. The examination was performed at a level just above the suprasternal notch in transverse and longitudinal views (Figure 1). A confirmation of a tracheal presence of ETT was interpreted as [1] the presence of two parallel hyper-echoic lines in the transverse or longitudinal images (Figure 2&3) [2] a non-intubated or empty esophagus. By moving the probe laterally it can be confirmed whether the esophagus is empty or distended by the ETT, as an ETT in the esophagus gives a similar image as when in the trachea. Presence of hyper-echoic lines laterally to the trachea, but absent in the trachea, confirmed an esophageal intubation indicate that the ETT is outside the trachea [22].
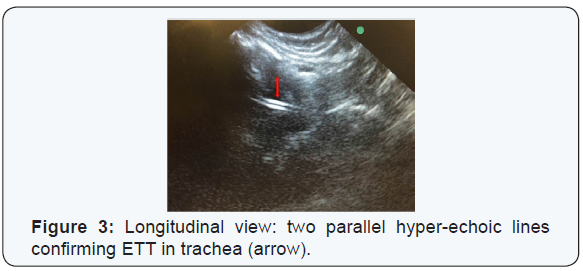
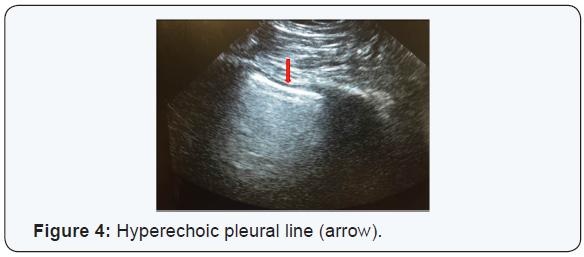
Bilateral presence of pleural sliding on US examination was used as an evidence of ETT location above the carina. To confirm pleural sliding, the probe was placed in the 3rd of the 4th intercostal space bilaterally and the presence of a hyper-echoic line moving with respiration indicates that the lung is being ventilated (Figure 4). All US examinations were performed by the same intensivist trained in the use of point-of-care US in managing ICU patients.
The clinician performing the intubation completed a data collection sheet post-intubation, which recorded the indication for intubation, intubation difficulty scale score (Cormack-Lehane scale) [23], size of the ETT, the confirmatory methods of ETT position and the chest radiograph findings. The intensivist performing the US examination recorded the US findings on a separate data collection sheet, which included the interpretation of the images for tracheal presence and pleural sliding. These two data sheets were then stored in a secure location for later analysis.
The null hypothesis of our study was that there is no difference in the diagnostic accuracy of the standard method and the US method for immediate confirmation on proper ETT position. Fischer’s exact test was used for analysis. Statistical analysis was performed using Graph Pad Prism version 6.04 for Windows (Graph Pad Software, La Jolla California USA).
Results
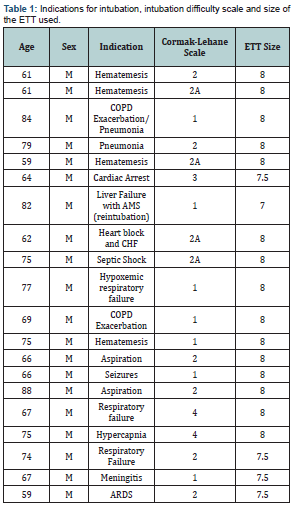
All patients in the study were males with an average age of 70.5 years. The indications for intubation, intubation difficulty scale and the size of the ETT is shown in Table 1. As per the standard method used to confirm ETT position, all twenty patients had a correctly placed ETT, but the post-intubation chest radiograph showed a right main stem intubation in one patient that was missed by the standard method of confirmation. US examination confirmed the proper placement of the ETT in 19 patients and was able to detect the right main stem intubation in that one patient. Hence the diagnostic accuracy of the US method was 100% (20/20) and that of the standard method 95% (19/20), with a p value of 1.0. The sensitivity and ppv of the US method was 100% (CI 79.9 - 100%), and the standard method had a 100% (CI 79.1 - 100%) sensitivity and 95% (CI 73.1 - 99.7%) ppv.
Discussion
The 2010 AHA guidelines for ACLS recommend the use of clinical assessment and confirmatory devices to verify ETT position [3]. Clinical assessment includes auscultation of the chest and epigastrium and observing chest rise with ventilation, but these methods have been shown to be unreliable [7], and esophageal intubation has been shown to go undetected in 0.4-15% [1,3]. In the event of cardiac arrest, clinical assessment methods require an interruption of chest compressions, which is not, recommended as per the AHA guidelines as it decreases the perfusion time [3]. A chaotic noisy environment during cardiac arrest, or an obese patient can result in inaccurate clinical assessment.
ETCO2 detection with either semi-quantitative or quantitative methods has been shown to be a reliable method for confirming a tracheal position of ETT, with quantitative waveform capnography considered the goal standard method [3,22]. But, these devices, especially waveform quantitative capnography are not routinely available in many ICU’s [24,25]. ETCO2 detection can be severely limited in conditions of low pulmonary blood flow or airway obstruction [6]. In these situations it can result in a false negative finding, which can lead to unnecessary reintubation attempts.
Insertion of an ETT with direct visualization of the glottis and viewing the ETT as it passes through the vocal cords is the gold standard method to confirm a tracheal position of the ETT. But, in patients with difficult airways, one may not be able to visualize the vocal cords, and the tube can get dislodged prior to securing the airway. Also, just relying on direct visualization of the vocal cords can miss a main-stem intubation. Therefore, each method has its limitations and intensivists have to rely on several methods immediately post-intubation to confirm a proper position of the ETT.
US can be a very useful adjunct to the standard methods of confirming proper ETT position. Point-of-care US use has risen significantly in the critical care field over the last decade [8,9], and US machines are now readily available in most ICU’s. There have been several studies describing the utility of US in assessing proper ETT position [5,10-12,14-16,18,24-26]. A prospective study evaluating the accuracy and timeliness of US compared to quantitative waveform capnography showed a 98.2% (CI 93.7- 99.5%) accuracy of the US method and a median operating time of 9 seconds [19]. The same investigators showed that US is a very accurate method to confirm ETT position in patients with in and out of hospital cardio-pulmonary-resuscitation (CPR) [20]. The use of US during CPR has advantages, as its use does not involve interruption of chest compressions, unlike the clinical assessment method. US images are not affected by poor perfusion or airway obstruction, as would the methods used to detect ETCO2, which rely on perfusion for delivery of carbon dioxide to the lungs. In their study there were five patients with tracheal intubation who were falsely determined to have esophageal intubation by waveform capnography resulting from low perfusion state [19]. Intensivists use US routinely to evaluate critically ill patients or those undergoing CPR for potentially reversible causes, and US to assess ETT position can be quickly performed, without interrupting resuscitation.
Studies with US have used different methods to confirm ETT position, which can be divided into direct and indirect methods. Direct methods involve confirming a tracheal location of the ETT by imaging the trachea, either in real-time as the ETT is passing through the vocal cords into the trachea, or after intubation [10,11,13,14]. ETT in the trachea produces two parallel hyper-echoic lines with posterior shadowing. An esophageal intubation, as described by Drescher et al., was best seen in transverse views as a second airway lateral to the trachea [22]. In the study by Werner et al. the esophagus was noticed to be in the left lateral location in 29 of the 33 patients [14]. Relying on the direct method, one can miss a main-stem intubation, which most likely will be seen on a chest radiographs done post-intubation. But, chest radiographs post-intubation take time and it can result in a delayed diagnosis of main-stem intubation, which can be detrimental in patients with severe hypoxemia or pneumothorax on the same side as the tube [27].
Indirect methods utilize presence of lung ventilation, as ascertained with pleural sliding or diaphragm motion, as evidence of correct ETT location [15-18,28]. With ventilation the visceral and parietal pleural surfaces slide against each other, which on US imaging is seen as a hyper-echoic line moving with respiration [9]. Pleural sliding by itself may not be the best method to confirm correct ETT position as pleural sliding maybe absent due to reasons other than an improper ETT location. Prior scarring of the pleura, pneumonectomy, atelectasis etc. can result in absent pleural sliding and can result in a false negative finding of an improperly located ETT. Patients not paralyzed during intubation can have spontaneous breaths, which can result in pleural sliding and an impression of a correctly placed ETT, when it might be in the esophagus. Similarly spontaneous breaths can produce diaphragm motion and can result in a false positive finding of correct ETT position, and in patients with paralyzed diaphragms it will be difficult to interpret findings.
In this study we showed that the US method had a perfect diagnostic accuracy, and that our hypothesis stays, concluding that there is no difference in the diagnostic accuracy between the two methods. The US method should be done sequentially, with tracheal US verifying a tracheal location of ETT followed by evaluation for pleural sliding and/or diaphragm motion bilaterally. Relying on just one method can lead to errors in judgment. We are not recommending that the US method replace, but, rather be used as an adjunct to the standard methods to confirm ETT position. ICU’s without ETCO2 detectors, patients with difficult airways, low perfusion states with likelihood of errors in capnography etc. are some of the situations where the US method can be useful. Immediate detection of a misplaced tube with US would help prevent inadvertent ventilation with AMBU-bag, stomach distention, and possible vomiting and aspiration.
There are several limitations to our study and the results cannot be generalized. The study has a small sample size with a high rate of successful intubations, with no esophageal intubations. A high rate of successful intubation makes it difficult to compare techniques and interpret results. It is a single center study involving a single expert user of the US method, hence the results cannot be generalized to centers lacking the same expertise. The strength of the study is that it was a prospective double blind study, performed on patients in clinical emergencies in the ICU rather than in a controlled environment on cadavers. This study suggests that ultrasound can be used in the immediate post intubation period to quickly confirm the ETT position, while still waiting for the chest radiograph to be performed. In some instances, chest radiograph is not immediately available to confirm ETT position, prolong time to ETT position confirmation maybe problematic in those critically ill tenuous patients in which inappropriate ETT for prolong periods might lead to complications. In summary, US confirmation of ETT position should be used as adjuvant to chest radiograph not as a replacement.
Conclusion
US imaging is an accurate method for immediate confirmation of ETT position in an intensive care unit and can be a useful adjunct to the standard methods of confirmation. In the event that capnography is unavailable, US can be a handy tool to verify ETT position.
References
- Jemmett ME, Kendal KM, Fourre MW, Burton JH (2003) Unrecognized misplacement of endotracheal tubes in a mixed urban to rural emergency medical services setting. Acad Emerg Med 10(9): 961-965.
- Jones JH, Murphy MP, Dickson RL, Somerville GG, Brizendine EJ (2004) Emergency physician-verified out-of-hospital intubation: miss rates by paramedics. Acad Emerg Med 11(6): 707-709.
- Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, et al. (2010) Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122: S729-S767.
- Lapinsky SE (2015) Endotracheal intubation in the ICU. Crit Care 19: 258.
- Pfeiffer P, Bache S, Isbye DL, Rudolph SS, Borglum J (2012) Verification of endotracheal intubation in obese patients - temporal comparison of ultrasound vs. auscultation and capnography. Acta Anaesthesiol Scand 56(5): 571-576.
- Li J (2001) Capnography alone is imperfect for endotracheal tube placement confirmation during emergency intubation. J Emerg Med 20(3): 223-229.
- Rudraraju P, Eisen LA (2009) Confirmation of endotracheal tube position: a narrative review.J Intensive Care Med 24(5): 283-292.
- Deshpande R, Akhtar S, Haddadin AS (2014) Utility of ultrasound in the ICU. Curr Opin Anaesthesiol 27(2): 123-132.
- Lichtenstein DA (2014) Lung ultrasound in the critically ill. Curr Opin Crit Care 20: 315-322
- Abbasi S, Farsi D, Zare MA, Hajimohammadi M, Rezai M, et al. (2015) Direct ultrasound methods: a confirmatory technique for proper endotracheal intubation in the emergency department. Eur J Emerg Med 22(1): 10-16.
- Das SK, Choupoo NS, Haldar R, Lahkar A (2015) Transtracheal ultrasound for verification of endotracheal tube placement: a systematic review and meta-analysis. Can J Anaesth 62(4): 413-423.
- Gottlieb M, Bailitz JM, Christian E, Russell FM, Ehrman RR, et al. (2014) Accuracy of a novel ultrasound technique for confirmation of endotracheal intubation by expert and novice emergency physicians. West J Emerg Med 15(7): 834-839.
- Uya A, Spear D, Patel K, Okada P, Sheeran P, et al. (2012) Can novice sonographers accurately locate an endotracheal tube with a saline-filled cuff in a cadaver model? A pilot study. Acad Emerg Med 19(3): 361-364.
- Werner SL, Smith CE, Goldstein JR, Jones RA, Cydulka RK (2007) Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med 49(1): 75-80.
- Mitra S, Kapoor D, Srivastava M, Sandhu H (2013) Real-time ultrasound guided percutaneous dilatational tracheostomy in critically ill patients: A step towards safety! Indian J Crit CareMed 17(6): 367-369.
- Chun R, Kirkpatrick AW, Sirois M, Sargasyn AE, Melton S, et al. (2004) Where’s the tube? Evaluation of hand-held ultrasound in confirming endotracheal tube placement. Prehosp Disaster Med 19(4): 366-369.
- Hosseini JS, Talebian MT, Ghafari MH, Eslami V (2013) Secondary confirmation of endotracheal tube position by diaphragm motion in right subcostal ultrasound view. Int J Crit Illn Inj Sci 3(2): 113-117.
- Sim SS, Lien WC, Chou HC, Chong KM, Liu SH, et al. (2012) Ultrasonographic lung sliding sign in confirming proper endotracheal intubation during emergency intubation. Resuscitation 83(3): 307-312.
- Weaver B, Lyon M, Blaivas M (2006) Confirmation of Endotracheal Tube Placement after Intubation Using the Ultrasound Sliding Lung Sign. Acad Emerg Med 13(3): 239-244.
- Jen-Tang Sun, Shyh-Shyong Sim, Hao-Chang Chou, Kah-Meng Chong, Matthew Huei-Ming Ma, et al. (2014) Ultrasonography for proper endotracheal tube placement confirmation in out-of-hospital cardiac arrest patients: two-center experience. Crit Ultrasound J 6(Suppl 1): A29.
- Chou HC, Tseng WP, Wang CH, Ma MH, Wang HP, et al. (2011) Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation 82(10): 1279-1284.
- Drescher M, Conard F,U., Schamban N (2008) Identification and Description of Esophageal Intubation Using Ultrasound. Academic Emergency Medicine 7(6): 1-4.
- Yentis SM, Lee DJ (1998) Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia 53(11): 1041-1044.
- Petroianu G, Maleck W, Bergler W, Ruefer R (1996) Carbon monoxide and nonquantitative carbon dioxide detection. Prehosp Disaster Med 11(4): 276-279.
- Deiorio NM (2005) Continuous end-tidal carbon dioxide monitoring for confirmation of endotracheal tube placement is neither widely available nor consistently applied by emergency physicians. Emerg Med J 22(7): 490-493.
- Adi O, Chuan TW, Rishya M (2013) A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit Ultrasound J 5(1): 7.
- Blaivas M, Tsung JW (2008) Point-of-care sonographic detection of left endobronchial main stem intubation and obstruction versus endotracheal intubation. J Ultrasound Med 27(5): 785-789.
- Hsieh KS, Lee CL, Lin CC, Huang TC, Lu WH, et al. (2004) Secondary confirmation of endotracheal tube position by ultrasound image. Crit Care Med 32(Suppl 9): S374-377.