Abstract
Neck dissection remains a cornerstone in the surgical treatment of head and neck cancers, particularly for managing cervical lymph node metastasis. Despite its therapeutic value, this procedure carries a notable risk of complications due to the complex anatomy of the neck and proximity to vital structures such as the spinal accessory nerve, internal jugular vein, and thoracic duct. Complications can be immediate or delayed and range from minor issues like hematoma and seroma to more severe outcomes such as chyle leak, nerve palsy, and wound dehiscence.er the initial SARS-CoV-2 infection, such as fatigue, shortness of breath, chest pain, and neurocognitive dysfunctions. Oral symptoms include ulcers, throaNeck dissection remains a cornerstone in the surgical treatment of head and neck cancers, particularly for managing cervical lymph node metastasis. Despite its therapeutic value, this procedure carries a notable risk of complications due to the complex anatomy of the neck and proximity to vital structures such as the spinal accessory nerve, internal jugular vein, and thoracic duct. Complications can be immediate or delayed and range from minor issues like hematoma and seroma to more severe outcomes such as chyle leak, nerve palsy, and wound dehiscence.
Keywords:Neck dissection; Surgical treatment; Head and Neck cancers; Cervical lymph node metastasis
Abbreviations:RND: Radical Neck Dissection; MRND: Modified Radical Neck Dissection; SND: Selective Neck Dissection; IEC: Institutional Ethics Committee
Introduction
Recent studies have reported postoperative complication rates ranging from 20% to 45%, with the most common being wound infection (up to 20.7%), nerve injuries (5-15%), and salivary fistulas (11.7%) [1-4]. Risk factors contributing to these complications include prior radiotherapy, advanced tumor stage, poor nutritional status, and comorbidities such as diabetes and hypertension [5]. The type of neck dissection also influences complication rates; for instance, radical neck dissection tends to have a higher incidence of functional morbidity compared to selective or modified radical procedures. With advances in surgical technique and perioperative care, the incidence and severity of complications have declined. However, their presence continues to impact patient recovery, functional outcomes, and quality of life. A thorough understanding of these risks is essential for clinicians to make informed decisions, provide accurate patient counseling, and implement preventive strategies during the perioperative period.
Methodology
Study design
This is a retrospective cohort study conducted at the Kidwai Memorial Institute of Oncology, Bangalore, involving a total of 289 patients diagnosed with various head and neck cancers. The study period spans from January 2022 to December 2024. The objective was to evaluate the outcomes of neck dissection procedures, identify associated risk factors, and determine the incidence of postoperative complications among patients who underwent neck dissection for head and neck cancers.
Study population
The study included 289 patients who were admitted to the Department of Oral Oncology at the Kidwai Cancer Institute , Bangalore during the study period. Inclusion criteria were as follows:
a) Patients who underwent neck dissection as part of their treatment for head and neck cancers
b) Patients who underwent either primary or post-chemoradiotherapy neck dissection.
c) Patients who had unilateral or bilateral neck dissection.
Data collection
Data was retrospectively retrieved from the medical records of patients who underwent neck dissection during the study period. The following information was collected:
a. Clinical Data: Age, gender, smoking habits, alcohol use, diabetes, and clinical history.
b. Surgical Data: Type of neck dissection (Radical Neck Dissection (RND), Modified Radical Neck Dissection (MRND), Selective Neck Dissection (SND)), details of the primary tumor, surgical time, and concomitant procedures.
c. Pathological Data: Lymph node status (preoperative and postoperative), pathological nodal involvement, and evidence of extracapsular spread.
d. Treatment Data: Chemoradiotherapy history, type of neck dissection performed (RND, MRND, or SND), and timing of surgery post-chemoradiotherapy (12-14 weeks).
e. Postoperative Data: Immediate, early, and late postoperative complications, management of complications, and rehabilitation outcomes.
Neck dissection classification
The neck dissection procedures were classified into three types:
a) Radical Neck Dissection (RND): Removal of all lymph nodes from levels I to V, along with the sternocleidomastoid muscle, internal jugular vein, and spinal accessory nerve.
b) Modified Radical Neck Dissection (MRND): Removal of lymph nodes from levels I to V, with preservation of the sternocleidomastoid muscle, internal jugular vein, and spinal accessory nerve.
c) Selective Neck Dissection (SND): Removal of selected lymph node levels, including levels I-III, IV, or II-IV, depending on the location of the primary tumor.
RND and MRND were performed using a tri-flapped incision, whereas a bi-flapped incision was adopted for SND.
Inclusion criteria for neck dissection
The inclusion criteria for neck dissection included:
I. Neck dissection performed alongside excision of the primary tumor.
II. Neck dissection as a primary procedure in cases of unknown primary tumors.
III. Neck dissection following chemoradiotherapy, with surgery performed 12-14 weeks post-treatment.
IV. Unilateral neck dissection.
Postoperative complications
Postoperative complications were categorized into three groups based on their onset:
a. Intraoperative Complications occurring during the surgery.
b. Early Onset: Complications occurring or detected within 24 hours after surgery.
c. Late Onset: Complications occurring or detected between 24 to 7 days post-surgery.
Statistical Analysis
Data were entered into a spreadsheet and analyzed using SPSS Statistics for Windows (version 25.0). Descriptive statistics were used to summarize patient demographics, clinical characteristics, and surgical outcomes. The analysis also focused on identifying risk factors associated with postoperative complications, such as age, gender, smoking, alcohol use, diabetes, lymph node status, and the type of neck dissection performed.
Ethical Considerations
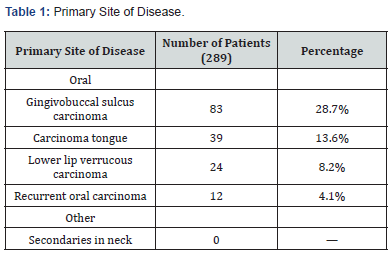
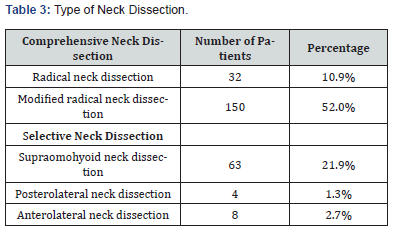
Ethical clearance was obtained from the Institutional Ethics Committee (IEC) of Kidwai Memorial Institute of Oncology. All patient data were anonymized to ensure confidentiality (Table 1-3). A total of 289 patients underwent neck dissection for various head and neck pathologies. The most common primary site of disease had been the oral cavity. Gingivobuccal sulcus carcinoma was the predominant lesion, identified in 83 patients (28.7%). Carcinoma of the tongue was the second most frequent diagnosis, observed in 39 patients (13.6%), followed by lower lip verrucous carcinoma in 24 patients (8.2%) and recurrent oral carcinoma in 12 patients (4.1%). No cases of secondaries in the neck were documented in this cohort. Comprehensive neck dissections had been performed in the majority of patients. Modified radical neck dissection was the most commonly performed procedure, undertaken in 150 patients (52.0%), while radical neck dissection was carried out in 32 patients (10.9%). Among selective neck dissections, the supraomohyoid approach was the most frequently used, performed in 63 patients (21.9%).
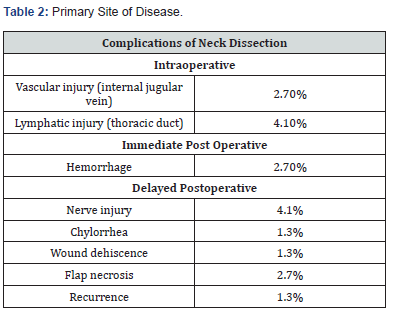
Anterolateral and posterolateral neck dissections were less frequently performed, accounting for 8 (2.7%) and 4 (1.3%) patients, respectively. A range of intraoperative and postoperative complications had been recorded. Intraoperatively, vascular injury involving the internal jugular vein occurred in 8 patients (2.7%), while thoracic duct lymphatic injury was noted in 12 patients (4.1%). Immediate postoperative complications included hemorrhage in 8 patients (2.7%). Delayed postoperative complications included nerve injury in 12 patients (4.1%), chylorrhea and wound dehiscence in 4 patients (1.3%) each, and flap necrosis in 8 patients (2.7%). Tumor recurrence during follow-up was identified in 4 patients, representing 1.3% of the cohort.
Discussion
The present study analyzed 289 patients who underwent neck dissection for various head and neck pathologies, with oral cavity cancers, particularly gingivobuccal sulcus carcinoma, being the most prevalent. This is consistent with the regional burden of oral malignancies in South Asia, where betel quid and tobacco use are major risk factors [1]. Modified radical neck dissection (MRND) emerged as the most frequently performed procedure in this cohort, accounting for over half the cases (52%). This aligns with the standard surgical approach for clinically positive neck disease in oral cancers while preserving non-lymphatic structures to reduce morbidity [4]. Selective neck dissections, primarily of the supraomohyoid type, were appropriately utilized in early-stage cancers and N0 necks, consistent with current oncologic guidelines.
The overall complication profile observed in this study reflects findings from the broader literature. Intraoperative complications such as vascular injuries, including internal jugular vein trauma (2.7%), and thoracic duct injuries (4.1%) closely mirror incidence rates reported in previous studies, including those by Bhushan & Arun (2019) and Das et al. (2022). Notably, thoracic duct injury, although less common, is a well-documented risk in left-sided neck dissections, particularly at levels IV and V. Postoperative complications included hemorrhage (2.7%), nerve injury (4.1%), and flap necrosis (2.7%). These rates are relatively lower than those reported in other retrospective analyses [1], which found hemorrhage in 14% and nerve injury in 5.4% of cases. The lower complication rates in the current cohort may be attributed to meticulous surgical technique and perioperative care [3]. Nerve injuries, especially involving the marginal mandibular and spinal accessory nerves, remain a significant concern due to their long-term functional impact [3]. In this study, the incidence of nerve injury was 4.1%, which is comparable to the 5.5% marginal mandibular nerve injury rate reported in other literature. Chylorrhea and wound dehiscence each occurred in 1.3% of patients in the current study. While these rates are lower than those in larger series [1], they still pose significant postoperative challenges. Prompt identification and conservative management often suffice, although persistent leaks may necessitate re-intervention.
Interestingly, the tumor recurrence rate during follow-up was just 1.3%. This low recurrence may reflect appropriate case selection, accurate staging, and adherence to comprehensive surgical margins. However, longer-term follow-up is required to validate these outcomes, as recurrence in head and neck cancers often manifests beyond the early postoperative period. Compared to broader databases such as the ACS-NSQIP, which noted significantly higher complication rates in cases involving complex reconstructions [5], this cohort's outcomes suggest favorable surgical and perioperative standards in settings where flap reconstruction is not the predominant method [6-8]. Overall, the study underscores the importance of individualized surgical planning, careful intraoperative technique, and vigilant postoperative monitoring to minimize complications and ensure favorable oncologic outcomes. These findings reinforce conclusions from other regional studies and international literature advocating for a balanced approach that considers oncologic control alongside quality of life [2].
Conclusion
This retrospective analysis highlights the clinical profile, surgical patterns, and complication rates associated with neck dissection in patients with head and neck malignancies. The oral cavity, particularly the gingivobuccal sulcus, emerged as the most common primary site. Modified radical neck dissection was the most frequently employed technique, reflecting its adaptability in balancing oncologic clearance with functional preservation.
Although intraoperative and postoperative complications were present, their incidence remained within acceptable limits and compares favorably with existing literature. Vascular and nerve injuries were among the most commonly encountered complications, underscoring the importance of precise surgical technique and thorough anatomical knowledge. The low recurrence rate observed during follow-up also reflects the effectiveness of the surgical strategies employed. Overall, these findings reaffirm the critical role of standardized surgical planning and execution in achieving optimal outcomes while minimizing morbidity. Ongoing evaluation and refinement of surgical techniques remain essential to further improve patient outcomes in head and neck oncology.
References
- Agrawal SM, Anehosur V (2021) Incidence and clinical analysis of complications of neck dissection. Indian J Otolaryngol Head Neck Surg 74(Suppl 3): 5875-5880.
- Bhushan SN, Arun HN (2019) Complications of neck dissection and their management: retrospective study. J Otorhinolaryngol Allied Sci.
- Kallappa S, Dange P (2020) An analysis of complications of neck dissection in head and neck cancers. Int J Clin Oncol Cancer Res 5(2): 17-21.
- Das D, Ghosh AK, Sardar S, Gayen GC (2022) Complications of neck dissection: our initial experience. Bengal J Otolaryngol Head Neck Surg.
- Pecorari G, Riva G, Albera A (2022) Postoperative infections in head and neck cancer surgery: risk factors for different infection sites. J Clin Med 11(17): 4969.
- Schliephake H, Jänicke M, Ewald C (2010) Postoperative morbidity after different types of selective neck dissection. J Craniomaxillofac Surg 38(1): 37-41.
- Eytan DF, Blackford AL, Eisele DW, Fakhry C (2021) Postoperative complications associated with the choice of reconstruction in head and neck cancer: an outcome analysis of 4,712 patients from the ACS-NSQIP database. JAMA Otolaryngol Head Neck Surg 147(3): 223-230.
- Rosenthal EL, Carroll WR (1995) Postoperative complications in patients with functional neck dissection. Arch Otolaryngol Head Neck Surg 121(10): 1150-1153.





























