Internal Laryngocele Managed with LASER-Assisted Microlaryngoscopic Excision
Riya Thakral1, Abhinav Srivastav2, Anshul Chatrath3*, Vishwani Khanna4, Sanjeev Awasthi5, Vivek Kumar Pathak6 and Luv Gupta7
1Junior Resident, Department of ENT and Head and Neck, School Medical Sciences and Research, Sharda University Greater Noida, India
2Assistant Professor, Department of ENT and Head and Neck, School Medical Sciences and Research, Sharda University Greater Noida, India
3Assistant Professor, World college of Medical Sciences and Research and Hospital, India
4Senior Resident, Department of ENT and Head and Neck, School Medical Sciences and Research, Sharda University Greater Noida, India
5Professor, Department of ENT and Head and Neck, School Medical Sciences and Research, Sharda University Greater Noida, India
6Associate Professor, Department of ENT and Head and Neck, School Medical Sciences and Research, Sharda University Greater Noida, India
7Intern, Department of ENT and Head and Neck, School Medical Sciences and Research, Sharda University Greater Noida, India
Submission: July 26, 2024; Published: August 08, 2024
*Corresponding author: Anshul Chatrath, Assistant Professor, World college of medical sciences and research and hospital, Jhajjar, Haryana, India
How to cite this article: Riya Thakral, Abhinav Srivastav, Anshul Chatrath*, Vishwani Khanna, Sanjeev Awasthi, et al. Anatomical Variations on NCCT Nose and Paranasal Sinuses and their Relation with Symptoms of the Patients - A Retrospective Analysis. Glob J Oto, 2024; 27 (1): 556201. DOI: 10.19080/GJO.2024.27.556201
Abstract
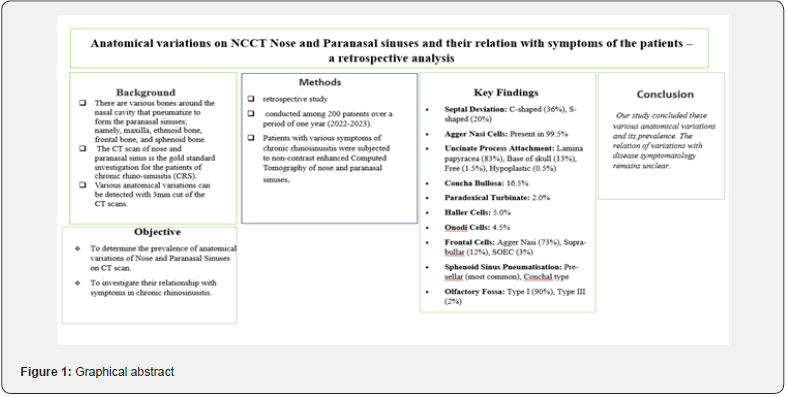
Background: There are various bones around the nasal cavity that pneumatize to form the paranasal sinuses; namely, maxilla, ethmoid bone, frontal bone, and sphenoid bone. The CT scan of nose and paranasal sinus is the gold standard investigation for the patients of chronic rhino-sinusitis (CRS).
Objective: This study was conducted with aim to determine the prevalence anatomical variation of Nose and Paranasal Sinuses on CT-scan and their relation with symptoms.
Methods: A retrospective study was conducted among 200 patients over a period of one year (2022-2023). Patients with various symptoms of chronic rhinosinusitis were subjected to non-contrast enhanced Computed Tomography of nose and paranasal sinuses.
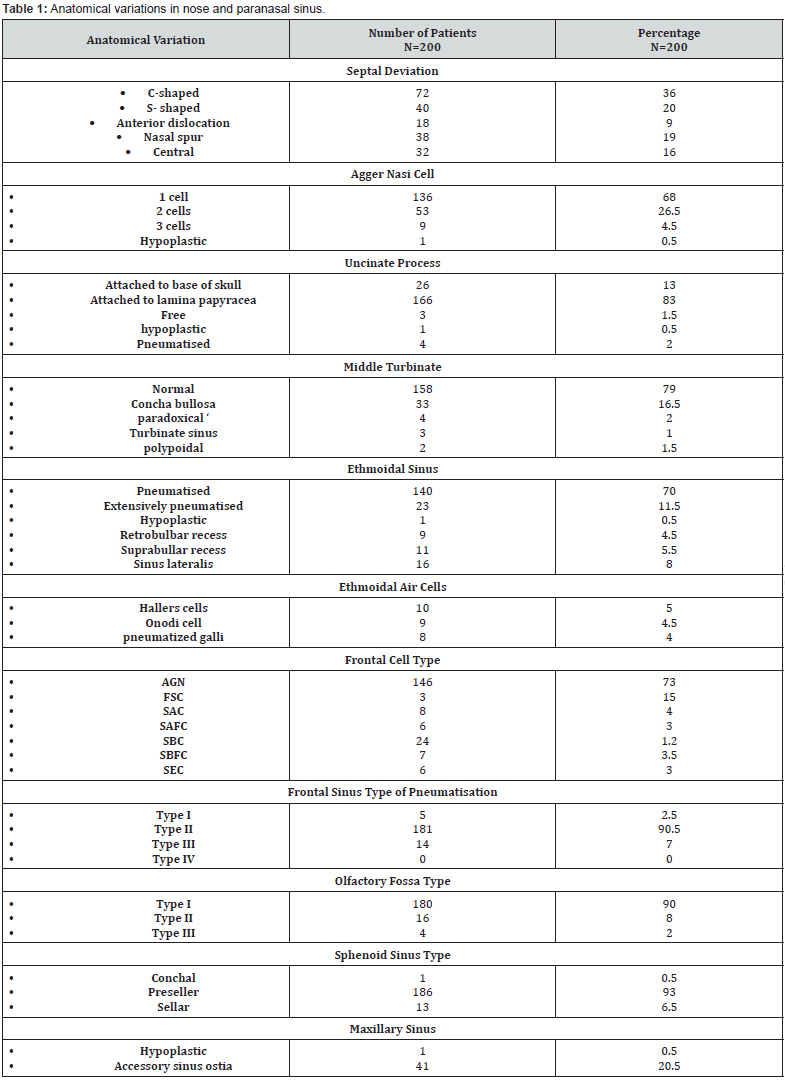
Results: In our study 56% patients had septal deviation with most common C shaped deviation followed by S shaped deviation. 99.5% patients have agger nasi cells. The attachment of uncinate process was to the lamina papyracea in 83.0%, followed by the base of skull in 13.0%. The least common types were free uncinate process in 1.5%. The prevalence of concha bullosa was found 16.5%. However, paradoxical turbinate was present in 2.0% subjects. The incidence of Haller cells was found to be 5.0% and Onodi cells were found in 4.5%. The type of frontal cell was Agger Nasi followed by a Supra-bullar. In Sphenoid sinus, commonest type was pre-sellar type of pneumatization.
Conclusion: Our study concluded these various anatomical variations and its prevalence. The relation of variations with disease symptomatology remains unclear.
Keywords: Uncinate; LAMINA papyracea; Concha bullosa; Sphenoid sinus; Haller cells
Graphical Abstract: (Figure 1)
Introduction
There are various bones around the nasal cavity that pneumatize to form the paranasal sinuses; namely, maxilla, ethmoid bone, frontal bone, and sphenoid bone. Persistent inflammation of the sinus or nasal channels lasting longer than 12 weeks at a time is known as chronic rhino-sinusitis (CRS). More than one episode of sinusitis per year is considered as recurrent sinusitis [1]. The CT scan of nose and paranasal sinus is the gold standard investigation for the patients of CRS. Various anatomical variations can be detected with 3mm cut of the CT scans. This occurs due to varying degree of pneumatization [2]. These anatomical variations may play an important role in disease pathogenesis and failure of medical treatment. In pre-operative planning it is crucial to understand and have knowledge of the various anatomical variations. This will help to create a road map for surgery to prevent injury to adjacent vital tissues like the brain, orbit, optic nerve, carotid artery, etc.
This study was conducted with Aim:
i. To determine the prevalence anatomical variation of Nose and Paranasal Sinuses on CT-scan
ii. To determine relation of symptoms with anatomical variation in nose and paranasal sinuses.
Methodology
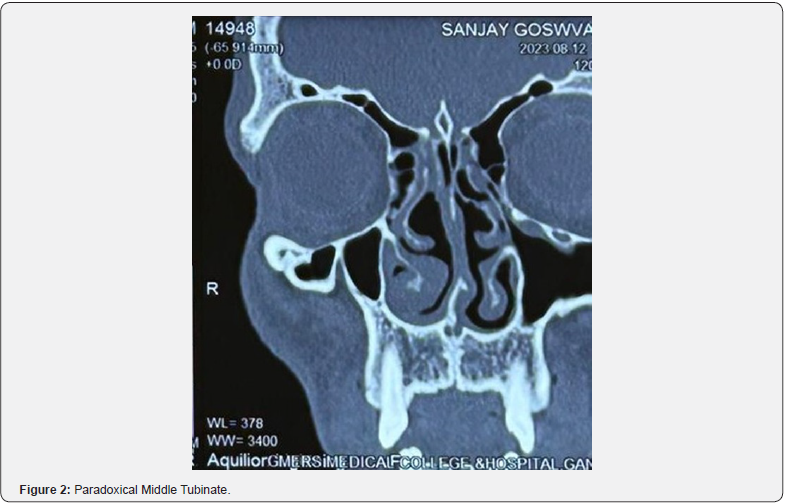
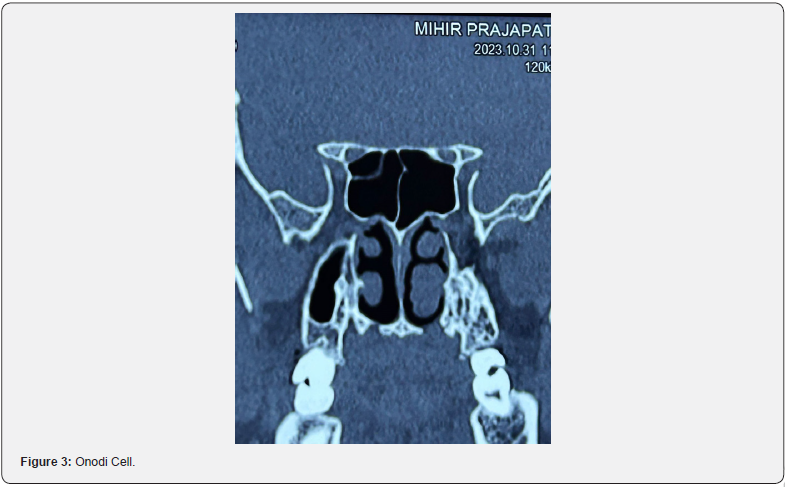
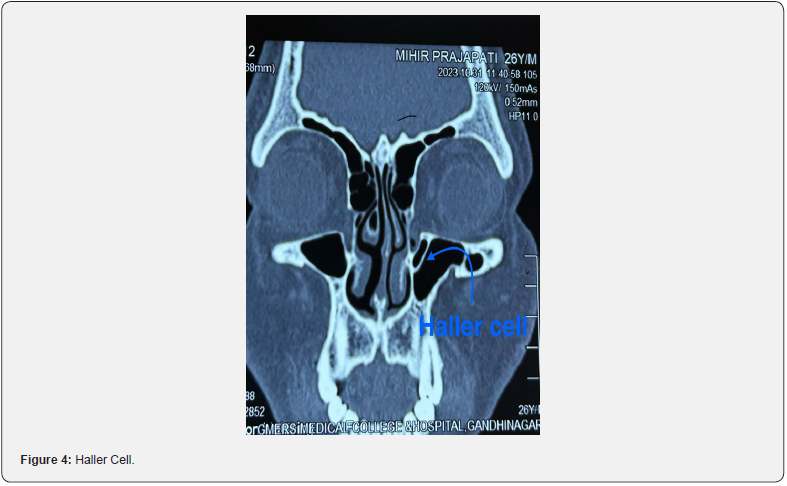
A retrospective study was conducted amongst 200 patients over a period of one year (2022-2023) at Sharda hospital Greater Noida . Patients with various symptoms of chronic rhinosinusitis were subjected to non-contrast enhanced Computed Tomography of nose and paranasal sinuses. Anatomic variations of the sinonasal cavities were assessed in the CT images, and prevalence of each was noted. The study included patients with age ≥ 18 having chronic rhinosinusitis and patient having chronic rhinosinusitis with or without polyposis who were advised NCCT nose and PNS after thorough examination. Patients having any previous nasal surgery or trauma, who did not consent for the study and patients less than 18 years were excluded from the study (Figure 2-4).
Results
In our study population of 200 subjects, majority of patients were in the age group of 26-35 years with mean age 34.15±12.67 years. There was male dominance, 58.5%. In our study, patients showed varying symptoms, most common were nasal obstruction (88%), sneezing (85%), rhinorrhoea (85.5%), poor sleep (78%) and headache (60%). On clinical examination, majority of the patients showed bilateral hypertrophy of inferior turbinate, 86%. On anterior rhinoscopy, 65 patients had nasal polyps (32.5%). Various anatomical variations on NCCT are shown in (Table 1). The relation of variations with disease pathology remains unclear.
Discussion
In humans, there are four pairs of sinuses. These are named after the bones which they pneumatize. They are: The maxillary sinus, ethmoid sinus, frontal sinus and sphenoid sinuses. Sinusitis is an inflammatory process involving the mucus membrane of the paranasal sinuses and/or the bone. computed tomography plays important role to know anatomical variations of nose and PNS and the extent of disease [2]. The aetio-pathology of sinusitis can be influenced by a multitude of clinically relevant alterations in the nose and paranasal sinuses. Since they are found in many people, sinonasal anatomic variants are more common than unusual [1]. These variations require CT scans for diagnosis to avoid any complication during endoscopic sinus surgery and various skull base surgeries.
Nasal septum
Deviated septum is a prevalent physical abnormality. If present, deviation may lead to lateralisation of middle turbinate leading to narrowing of middle meatus and hypertrophy of contralateral turbinate. This leads to obstruction of normal mucous flow, resulting in subsequent inflammation [3,4]. According to literature, prevalence of septal deviation is widely varied. Due to different morphologies, it ranges from 26-97% [5]. In our study 56% patients had septal deviation with most common C shaped deviation followed by S shaped deviation However, not all patients having a deviated septum had complaints of nasal obstruction, headache, or poor sleep. 9% of our patients had Anterior dislocation in which 8% patients had history of trauma and only 3% complaint of cosmetics deformity.
Agger nasi cells
The anterior most group of ethmoid air cells are the agger nasi. They can typically be bilateral. Usually, they pneumatise toward the region of frontal recess making it narrow which may lead to sinusitis [6]. For identification, coronal and sagittal views of CT scans are considered ideal [3]. In 1967, Messerklinger et al. reported 10-15% specimens having agger nasi cell during dissection [7] whereas according to a study done in Malaysia, agger nasi is highly prevalent (83.0%) [8]. Their reported prevalence ranges from 10% to 98% [9]. In our study, 99.5% of patients have agger nasi cells. 1 patient had hypoplastic agger nasi cell.
Uncinate process
The uncinate process is a key bony structure in the lateral nasal wall. Attachment of uncinate process can be variable, such as attached to lamina papyracea, middle turbinate, or base of skull. Sometimes, the uncinate process maybe free-lying or pneumatised as well. In a study conducted by Basak S., recorded variations of the upper end of uncinate in 25% of the CT sections [10]. Our study revealed the most common attachment to be the lamina papyracea, in 83.0%, followed by the base of skull in 13.0%. The least common types were free uncinate process in 1.5% and hypoplastic uncinate process seen in 0.5% of subjects.
Aeration of uncinate process is known as pneumatised uncinate or an uncinate bulla. Kennedy et al. [11] 1998 study revealed the incidence of this rare variant was 0.4% [11]. Depending on the degree of pneumatisation, there can be significant blockage of the osteo-meatal complex. Along with other variations in anatomy it can intensify the pathogenic impact causing CRS. In our study group, 4 patients (2.0%) showed this rare entity.
Middle turbinate
A concha bullosa is the pneumatisation of the middle concha. Ethmoidal expansion results in pneumatisation of the osseous plate. Its size is mostly variable and can be found on either side or sometimes is bilateral [3]. Patients suffering from chronic rhinosinusitis have the highest reported prevalence, 15- 80% [5]. A large concha bullosa with considerable pneumatisation can cause symptoms of headaches, and/or significant nasal obstruction. In such cases, a surgical correction maybe required. The middle concha’s convexity is normally oriented medially, i.e., towards the septum. However, in a paradoxical turbinate, the convexity is laterally faced [12]. Owing to the deformity and obstruction of airflow, it can be presumed as an additional factor for causing sinusitis [13].
According to Mokhasanavisu et al. [14] concha bullosa was found in 64% and 52% of the populations of South and North India, respectively [14]. Azila A, et al. [8] in their recorded concha bullosa in 40.8% subjects having CRS and in 47.5% of control cases [8]. Amongst the Caucasians concha bullosa and paradoxical turbinate have been recorded as 12-31% and 10-22% respectively [15]. In our study, prevalence of concha bullosa was found 16.5%. However, paradoxical turbinate was present in 2.0% subjects. 90% of patients with concha bullosa had symptoms like headache, nasal obstruction, facial pain, which were relieved after surgical correction.
Ethmoid air cells
Albert von Haller first characterised Haller cells in 1765. They are ethmoid cells above and beside the maxillary sinus ostium growing into the floor of orbit [15]. Their frequency varies astonishingly, from 8% to 57%. The detrimental effect on maxillary sinus airflow is caused by limitation of infundibulum and maxillary ostium. Thus, establishing a link to recurrent maxillary sinusitis, making this variation clinically noteworthy [3].
Furthermore, orbital injuries after ethmoidectomy can be more likely when Haller cells are present [16]. Badia et al. [15] reported the presence of Haller cells in 10-15% Caucasian and 1-9% Chinese group respectively [15]. The Onodi cell (sphenoethmoid air cell), is a posterior ethmoid cell that is closely linked to the optic nerve. It pneumatises far laterally and somewhat superiorly to the sphenoid sinus.
The internal carotid artery and optic nerve are more vulnerable to injury when Onodi cells are present. Thus, identification before surgery is of utmost importance [3,13]. Its frequency is reported to fluctuate widely, from 2% to 50%. [16]. In Chinese population, presence of Onodi cells has been reported as 20-30 [15]. In the adult group, 48% of Onodi cells were found, according to Bansberg et al. [17]. In the current study, incidence of Haller cells was found in 5.0% and Onodi cells were found in 4.5% of subjects which comparable to previous studies.
Frontal recess cells
The fronto-ethmoidal cells, are cells located above Agger Nasi. In functional endoscopic sinus surgery, it is essential to comprehend these variances since they impact the likelihood of complications and the operative outcome. To provide better understanding of the morphology of frontoethmoidal cells and their relationship to frontal recess, the International Frontal Sinus classification (IFSC) was introduced. A study was conducted in Mexico by Bravo-Arteaga et al. [18] SAFC (Supra- Agger Frontal cell) had a prevalence of 7.88% [18]. In Vietnam, Luan V reported SBFC (Supra-bullar frontal cell) in 4.3% patients [19], while a study from Malaysia reported a prevalence of 53% [20].
According to Asian analysis, a mere prevalence of 5.4% of SOEC (Supra-orbital ethmoid cell) was observed. [21]. In addition to raising the possibility of orbital injury during surgery, the presence of SOEC has been linked to orbital proptosis [9]. Our study revealed the commonest cell type as Agger Nasi (73.0%), followed by a Supra-bullar cell seen in 12.0%. SOEC was prevalent in 3.0% of subjects.
Sphenoid sinus variation
Sphenoid sinus may show extension of pneumatisation laterally to the pterygoids, and can involve the lesser and/or greater wing of sphenoid. The sphenoid sinus was divided into three categories by Hammer and Radberg. According to their analysis, the sellar variant accounted for 85% of all instances, making it the most prevalent pattern. The presellar and conchal types accounted for 11% and 2.5% of cases, respectively [22]. In the current study, the commonest type was pre-sellar, followed by conchal type of pneumatisation.
Olfactory fossa
Variations in anatomy can occasionally lead a surgeon to catastrophic outcomes. For instance, if low skull base is not known pre-operatively it may lead to intra-cranial complications post endoscopic surgery. In 1962, Keros classification was given describing the depth olfactory fossa. The cribriform plate and fovea ethmoidalis are taken into consideration. In type III (8- 16mm), the risk of injury to lateral lamella of cribriform plate with subsequent CSF leak is the highest. According to Ali et al. [23] 79% of patients had Keros II [23]. Nouraei et al. [2] reported 92% of patients had Keros type 1 olfactory fossa [9]. In 2014, Al-Abri R et al. 36% of patients had type III fossa [2]. In our study, Type I fossa was seen in 90% of the study population, whereas, only 2.0% subjects had type III fossa. The differences in race and ethnicity may contribute to the observed gap.
There have been various discussions over the contribution of these anatomical differences to the aetiology of chronic rhinosinusitis. However, the discussions have been inconclusive. In a study conducted in 2020, showed that anatomical variations and symptom severity had a statistically significant relationship [1]. However, according to reports of Asian researchers, no correlation has been established between the two, nor have they shown to worsen pre-existing rhino-sinusitis [24].
Conclusion
Nose and PNS are well known for their complicated anatomy and numerous variations. Modern imaging methods allow for detection of anatomical differences in patients. Our study concluded these various anatomical variations along with their prevalence. These variations are said to play role in symptomatology of patients having CRS. In our study the relation of variations with disease symptomatology remains unclear [25]. This study’s shortcomings include its relatively small sample size and most participants belonging to a single race. Variants in different ethnic groups require further research. Nevertheless, each variation must be considered individually, underscoring the significance of preoperative imaging.
References
- Shirama YB, Adamu A, Ahmed SS, Iseh KR, Ma’aji SM, et al. (2020) Relationship between Sinonasal Anatomical Variations and Symptom Severity in Patients with Chronic Rhinosinusitis. J West Afr Coll Surg 10(1): 20-25.
- Al-Abri R, Bhargava D, Al-Bassam W, Al-Badaai Y, Sawhney S (2014) Clinically significant anatomical variants of the paranasal sinuses. Oman Med J 29(2): 110-113.
- Turna O, Aybar M, Karagoz Y, Tuzcu G (2014) Anatomic Variations of the Paranasal Sinus Region: Evaluation with Multidetector CT. Istanbul Med J 15: 104-109.
- Balikci HH, Gurdal MM, Celebi S, Ozbay I, Karakas M (2016) Relationships among concha bullosa, nasal septal deviation, and sinusitis: retrospective analysis of 296 cases. Ear Nose Throat J 95(12): 487-491.
- Alsowey AM, Abdulmonaem G, Elsammak A, Fouad Y (2017) Diagnostic performance of multidetector computed tomography (MDCT) in diagnosis of sinus variations. Pol J Radiol 82: 713-725.
- Dasar U, Gokce E (2016) Evaluation of variations in sinonasal region with computed tomography. World J Radiol 8(1): 98-108.
- Messerklinger W (1967) On the drainage of the normal frontal sinus of man. Acta Otolaryngol 63(2): 176-181.
- Azila A, Irfan M, Rohaizan Y, Shamim AK (2011) The prevalence of anatomical variations in osteomeatal unit in patients with chronic rhinosinusitis. Med J Malaysia 66(3): 191-194.
- Nouraei SA, Elisay AR, Dimarco A, Abdi R, Majidi H, et al. (2009) Variations in paranasal sinus anatomy: implications for the pathophysiology of chronic rhinosinusitis and safety of endoscopic sinus surgery. J Otolaryngol Head Neck Surg 38(1): 32-37.
- Başak S, Akdilli A, Karaman CZ, Kunt T (2000) Assessment of some important anatomical variations and dangerous areas of the paranasal sinuses by computed tomography in children. Int J Pediatr Otorhinolaryngol 55(2): 81-89.
- Kennedy DW, Zeinreich SJ (1998) Functional endoscopic approach to inflammatory sinus disease: Current perspectives and technique modifications. Am J Rhinol 2(3): 89-96.
- Cho JH, Park MS, Chung YS, Hong SC, Kwon KH, et al. (2011) Do anatomic variations of the middle turbinate have an effect on nasal septal deviation or paranasal sinusitis? Ann Otol Rhinol Laryngol 120(9): 569-574.
- Kasemsiri P, Thanaviratananich S, Puttharak W (2011) The prevalence and pattern of pneumatization of Onodi cell in Thai patients. J Med Assoc Thai 94(9): 1122-1126.
- Mokhasanavisu VJP, Singh R, Balakrishnan R, Kadavigere R (2019) Ethnic variation of sinonasal anatomy on CT scan and volumetric analysis. Indian J Otolaryngol Head Neck Surg 71(Suppl 3): 2157-2164.
- Badia L, Lund VJ, Wei W, Ho WK (2005) Ethnic variation in sinonasal anatomy on CT-scanning. Rhinology 43(3): 210-214.
- Shpilberg KA, Daniel SC, Doshi AH, Lawson W, Som PM (2015) CT of anatomic variants of the paranasal sinuses and nasal cavity: poor correlation with radiologically significant rhinosinusitis but importance in surgical planning. AJR Am J Roentgenol 204(6): 1255-1260.
- Bansberg SF, Harner SG, Forbes G (1987) Relationship of the optic nerve to the paranasal sinuses as shown by computed tomography. Otolaryngol Head Neck Surg 96(4): 331-335.
- Bravo-Arteaga SY, Durán-Ortiz M, Pineda-Cásarez F, Díaz-Sainz DE (2021) Frontoetmoidal cells prevalence in Mexican population using the International Frontal Sinus Anatomy Classification (IFAC). Otorrinolaringología 66(4): 309-315.
- Tran LV, Ngo NH, Psaltis AJ (2019) A Radiological study assessing the prevalence of frontal recess cells and the most common frontal sinus drainage pathways. Am J Rhinol Allergy 33(3): 323-330.
- Fawzi NEA, Lazim NM, Aziz ME, Mohammad ZW, Abdullah B (2022) The prevalence of frontal cell variants according to the International Frontal Sinus Anatomy Classification and their associations with frontal sinusitis. Eur Arch Otorhinolaryngol 279(2): 765-771.
- Zhang L, Han D, Ge W, Tao J, Wang X, et al. (2007) Computed tomographic and endoscopic analysis of supraorbital ethmoid cells. Otolaryngol Head Neck Surg 137(4): 562-568.
- Keerthi PH, Savagave SG, Sakalecha AK, Reddy V, L YU (2022) The Evaluation of Variations in Patterns of Sphenoid Sinus Pneumatization Using Computed Tomography in a South Indian Population. Cureus 14(3): e23174.
- Ali A, Kurien M, Shyamkumar NK, Selvaraj (2005) Anterior skull base: High-risk areas in endoscopic sinus surgery in chronic rhinosinusitis: A computed tomographic analysis. Indian J Otolaryngol Head Neck Surg 57(1): 5-8.
- Kaygusuz A, Haksever M, Akduman D, Aslan S, Sayar Z (2014) Sinonasal anatomical variations: their relationship with chronic rhinosinusitis and effect on the severity of disease-a computerized tomography assisted anatomical and clinical study. Indian J Otolaryngol Head Neck Surg 66(3): 260-266.
- Hung K, Montalvao C, Yeung AWK, Li G, Bornstein MM (2020) Frequency, location, and morphology of accessory maxillary sinus ostia: a retrospective study using cone beam computed tomography (CBCT). Surg Radiol Anat 42(4): 219-228.





























