Audit of The Prevalence of Eustachian Tube Dysfunction (ETD) Using A Validated ETD7 Questionnaire
Samir Gendy*
Consultant ENT Surgeon, Emersons Green and Devizes Practice plus Group Hospitals, UK
Submission: May 11, 2023; Published: May 25, 2023
*Corresponding author: Mr Samir Gendy FRCS(ORL), Consultant ENT Surgeon, Emersons Green and Devizes Practice plus Group Hospitals, Marshall Road, Devizes, SN10 3UF, UK
How to cite this article: Samir G. Audit of The Prevalence of Eustachian Tube Dysfunction (ETD) Using A Validated ETD7 Questionnaire. Glob J Oto, 2023; 26 (1): 556178. DOI: 10.19080/GJO.2023.26.556178
Keywords: Eustachian tube; Middle ear; ET dysfunction; Mucus; Patulous ETD
Introduction
The Eustachian tube is located in a part of the head and neck called the parapharyngeal space. It runs from the front wall of the middle ear to the side wall of the top part of the throat (nasopharynx). In adults, the Eustachian tube slopes down about 35 degrees. In children, the Eustachian tube only slopes about 10 degrees down. The Eustachian tube is made of bone, cartilage, and fibrous tissue. It is a hollow tube that is
lined with hair-like projections (cilia) that sweep mucus away from the middle ear toward the nasopharynx [1]. There are six muscles that help the Eustachian tube open and close. The muscles are located in the ear, head, neck, soft palate, and jaw. The Eustachian tubes help make sure the middle ear stays healthy by:
I. Keeping the air pressure on both sides of the eardrum equal
II. Draining secretions from the middle ear
III. Protecting the middle ear from pathogens like bacteria and viruses
Each Eustachian tube usually stays closed to act as a barrier to protect the ear. However, they will open when the muscles contract-for example, when a person is yawning and swallowing. When the air pressure changes outside, the Eustachian tube opens to allow air to move from the ear canal to the middle ear. This ensures the pressure can equalize on both sides of the eardrum. To keep the middle ear working right, the space around the tubes needs to be free of fluid and other debris. The cilia and mucosal folds in the Eustachian tube work together to drain the mucus that is made in the middle ear.
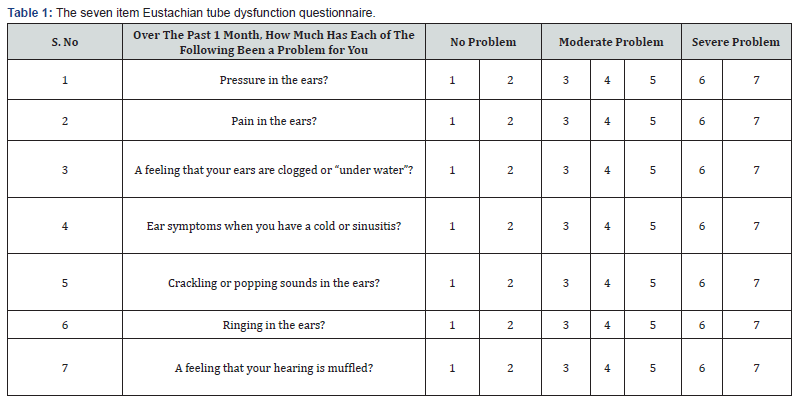
In 2015 a Consensus paper on management of ET dysfunction recommended the use of ETD7 validated questionnaire to assess the severity of ET dysfunction [1]. The ETD7 questionnaire (form enclosed) consists of 7 questions each has a response graded from 1 to 7 where 1 means no problem and 7 means severe problem then by adding the total score and dividing by 7 will give the average score that represents patient’s reflection on his/her ET dysfunction problem. A cut off point is a total score more than 14 and mean score more than 2.1 (Table 1) [2].
Material
In the period from September 2022 till end of December 2022 every patient who presented to the ENT clinics at Both Emerson’s green and Devizes Hospitals with symptoms suggestive of ET dysfunction for example: ear popping, ear fullness, pressure behind ear, fluid sensation, crackling sound of ears was handed the ETD7 questionnaire and explained the way to express his symptoms with the numbers in the form in addition to full ENT examination that includes otoscopy, audiogram, tympanometry, nasopharyngoscopy and Rinne’s and Weber’s tuning fork tests. The total number of patients were 25 adult patients with age range from 20 to 77 years old 14 female patients and 11 male patients of those patients 14 presented with symptoms of ETD of both ears while 11 presented with symptoms in one ear only. The Total ETDQ-7 Questionnaire scores ranged from 10 to 45 for the 25 patients with a mean total score of 27.1 and a mean item score ranged from1.4 to 6.4 with an average of 3.8.
Discussion
Eustachian tube dysfunction usually refers to a ventilator dysfunction and is defined by symptoms and signs of pressure dysregulation in the middle ear. In 2015 the Consensus panel on Eustachian tube dysfunction agreed that there are three subtypes of ET dysfunction: Dilatory ETD, Baro-Challenge-induced ETD, Patulous ETD. The Dilatory ETD is often preceded by upper respiratory tract infection, some patients may have prior history of otitis media with effusion. Some patients may report repeated Valsalva or jaw-thrust manoeuvres in an attempt to equalize negative middle ear pressure, others describe altered hearing or tinnitus. Dilatory ETD can be sub classified due to either Functional obstruction, Dynamic dysfunction (muscular failure) or due to anatomical obstruction.
In Baro-challenge-induced ETD patients have symptoms of aural fullness, popping in or discomfort in one or both ears that occurs or initiated under conditions of alteration to the ambient pressure typically manifested when scuba-diving or descent from altitude, patients are asymptomatic once return to the ground level and sometimes patients can present with temporary middle ear effusion or even Hemotympanum. Patulous ETD patients present with symptoms of aural fullness and auto phony that can improve on supine position or during upper respiratory tract infection and worsens during exercise. Patulous ETD is thought to be caused by abnormal patent Eustachian tube that can be precipitated by recent weight loss.
The Consensus panel confirmed that the ETD7 questionnaire is the only patient-reported outcomes tool to have undergone initial validation studies also it has the advantage of combining both subjective and objective measures of Eustachian tube functions. This study confirmed the importance of ETD7-questionnaire as a validated tool to reflect the severity of patient’s problem of Eustachian tube dysfunction and should be used in assessing patients with symptoms and signs suggestive of Eustachian Tube dysfunction.
References
- Schilder A,Bhutta M, CC Butler, C Holy, LH Levine, et al. (2015) Eustachian tube dysfunction : consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol 40(5): 407-411.
- Alper CM, Teixeira MS, Swarts JD 2018) Accuracy of the ETDQ-7Questionnaire for identifying persons with Eustachian tube dysfunction. Otolaryngol Head Neck Surg 158(1): 83-89.





























