Opportunities For Integration of Telemedicine into Otolaryngology
Salvador Aguirre, Thomas M Irwin III, W Spence Bodenhamer and Gary C Doolittle*
Professor, University of Kansas School of Medicine, USA
Submission: May 17, 2023; Published: May 25, 2023
*Corresponding author: Gary C Doolittle, MD, Professor, University of Kansas School of Medicine, 2330 Shawnee Mission Parkway, Mailstop 5003, Westwood, KS 66205, USA
How to cite this article: Aguirre S, Irwin TM III, Bodenhamer WS, Doolittle GC. Opportunities For Integration of Telemedicine into Otolaryngology. Glob J Oto, 2023; 26 (1): 556177. DOI: 10.19080/GJO.2023.26.556177
Abstract
Telemedicine has been thrust into the forefront of healthcare because of the COVID-19 pandemic. Obstacles faced during the pandemic made telemedicine a critical tool to facilitate patient care while minimizing in-person contact. Otolaryngology is a specialty that has been forced to adapt in order to adopt telemedicine and is finding it allows for new opportunities. Telemedicine helps to provide timely and convenient access to care, enable ongoing support for patients unable to attend clinic and maintain social distance during the pandemic. Telemedicine can also be used quite effectively to screen patients if they need to be seen by an otolaryngologist. Because otolaryngology examinations often involve physical examinations of small structures, these diagnostic procedures are often difficult or impossible to perform via telemedicine. Similarly, many primary care physicians are not trained in many otolaryngology practices or diagnostic procedures, and if they are, available equipment can be difficult to allow for their use via telemedicine. We discuss some barriers and potential solutions, detailing strategies that clinics and physicians can use to provide more effective otolaryngology care. Overall, telemedicine can make otolaryngologists more available to patients and primary care providers alike.
Keywords: Telemedicine; Otolaryngology; COVID-19 pandemic; Nasopharyngoscopy; Laryngoscopes
Opportunities for Integration of Telemedicine into Otolaryngology
The COVID-19 pandemic thrust telemedicine onto the world stage in a way not previously seen. With the disruption of in-person clinic visits worldwide, telemedicine became a lifeline for many patients across all specialties. Challenges to the implementation of telemedicine in more procedure-heavy specialties such as surgery and otolaryngology are readily apparent. How does one conduct a surgical assessment over video conferencing? What components of an in-office visit are possible over telemedicine, and how does the otolaryngologist make it a usable clinical tool? Fortunately, there are paths to making telemedicine not only a pandemic stopgap, but this paper will detail how it can become a desirable asset to the otolaryngologist going forward.
What Can Telemedicine Do for The Otolaryngologist Today?
During the pandemic, the number of otolaryngology consultants declined dramatically. Telemedicine services in otolaryngology allowed for continued patient care while keeping social distancing in place [1-3]. Telemedicine can provide timely and convenient access to care, reduce the risk of exposure to infectious diseases, and enable ongoing support for patients with chronic conditions. Telemedicine can allow clinicians to follow up with patients who might otherwise be unable to attend clinic visits for a variety of reasons including travel difficulties (expense, long distance, securing transportation), poor mobility, and scheduling problems, just to name a few. Telemedicine can be employed as a useful tool for taking a detailed history and ultimately determining whether a patient needs to be seen in person. As used in this setting, telemedicine can increase patient satisfaction and clinic efficiency [4].
Telemedicine can also be a resource in situations where the use of multidisciplinary conferencing is indicated (such as cochlear implantation or voice therapy, or in conjunction with speech pathology or audiology), and in settings where proper equipment is available and the otolaryngologist can be consulted within the primary care practitioner’s office for assistance in evaluation of a patient [5]. By extension, telemedicine can be used to screen the most basic of questions: does the patient need to be seen by an otolaryngologist? Telemedicine allows direct consultation between primary care providers (including family medicine, hospitalists, nursing home providers, rehabilitation specialists) and the otolaryngologist, allowing for a good history and some physical examination.
What are the Barriers to Telemedicine in Otolaryngology?
It is readily apparent that there are limitations. A limited physical examination is possible via telemedicine, and other diagnostic procedures such as endoscopy are not directly possible for the otolaryngologist via telemedicine. Moving to the notion of remote consultation, primary care physicians are rarely trained to do nasolaryngoscopy or nasopharyngoscopy in residency. Even if the primary care physician is trained to do these procedures, the clinic in which these physicians practice may not have access to video nasopharyngoscopy or even video otoscopy equipment. This has led to otolaryngology providers being less satisfied with telemedicine visits than patients and has (rationally) reduced the enthusiasm for its use in otolaryngology [6].
How to Make It Work in Otolaryngology Practice?
Telemedicine has irreversibly altered the landscape in medicine, and it is not going to go away. Given the barriers above, implementation presents a series of opportunities unique to otolaryngology. First of all, few primary care physicians are trained in the use of nasopharyngoscopy and flexible laryngoscopy. As otolaryngology relies on referrals from primary care, this offers an opportunity for the enterprising otolaryngologist to invite primary care physicians to train on the use of these instruments and to make connections with these PCPs so that they have someone in ENT that they can collaborate with. In addition, this added skill will provide more usable services in the PCP’s clinic. Secondly, flexible laryngoscopes are rather expensive [7,8].
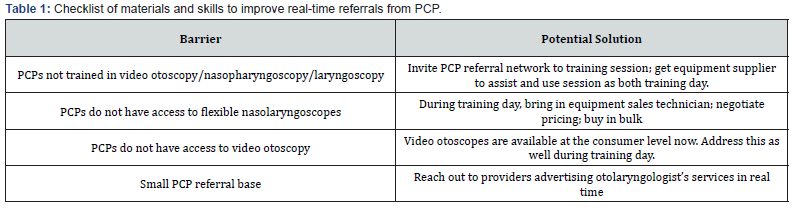
The enterprising otolaryngology practice would be welladvised to meet with their equipment suppliers and negotiate purchases of multiple laryngoscopes with video capability and then partner with primary care physicians in order to make these purchases cost-effective for the primary care practices, and to improve interplay between the otolaryngology practice and their expanding referral network. Thirdly, video otoscopy is now available at even the consumer level [9]. Plug-ins are now available for smartphones, and this barrier has declined precipitously for physicians [10]. Many primary care physicians are trained in basic otoscopy, and their effectiveness can be further enhanced by ready consultation access to otolaryngology in real time. By improving networking with primary care and assisting in training them to use some of the specialized instrumentation (and also understanding the workup sequence in otolaryngology), an otolaryngology practice can use telemedicine to increase its market penetration and expand its footprint well into its region (Table 1).
Future Ramifications
Telemedicine has established itself in the 21st century, especially in the era of the COVID-19 pandemic and beyond. This can be an opportunity for significant growth in the reach of otolaryngology practice and can increase the number of patients who attend in-person visits. This means courting primary care physicians and offering them telehealth consultations in real time. Working that out in terms of scheduling will vary by practice. If the primary care physicians are not trained in diagnostic procedures, offer to help train them.
Also, medical equipment manufacturers are never going to say no to the possibility of selling more of their equipment; contact your suppliers and ask them to assist you. Also set hours that a provider (who can be a nurse or advanced practice provider) can do telehealth consultations as screening for whether a patient needs to be seen in person. Telehealth can be used to make the otolaryngologist more available to patients and primary care providers. This, in turn, will drive traffic to the clinic and to the operating room.
References
- Lebedev G, Anton V, Pavel K, Eduard F, Irina F, et al. (2021) Justification of the method of remote monitoring of the health of young athletes based on mobile technologies. Procedia Computer Science 192: 3332-3341.
- Hu A, Sardesai MG, Meyer TK (2012) A need for otolaryngology education among primary care providers. Med Educ Online 17: 17350.
- Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, et al. (2020) Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 26(5): 309-313.
- Riley PE, Fischer JL, Nagy RE, Watson NL, McCoul ED, et al. (2021) Patient and Provider Satisfaction with Telemedicine in Otolaryngology. OTO Open 5(1): 2473974X20981838.
- Hoi KK, Curtis SH, Driver L, Wisnosky E, Zopf DA, et al. (2021) Adoption of Telemedicine for Multidisciplinary Care in Pediatric Otolaryngology. Ann Otol Rhinol Laryngol 130(10): 1105-1111.
- Choi JS, Kim JH, Park S, Matthew Lin, F Abdur-Rahman, et al. (2022) Telemedicine in Otolaryngology During COVID-19: Patient and Physician Satisfaction. Otolaryngol Head Neck Surg 167(1): 56-64.
- Parnes JA, Yeh DH, Glicksman JT, Tewfik MA, Sowerby LJ (2015) Surgeon-estimated costs of common consumables in otolaryngology. Laryngoscope 125(12): 2690-2694.
- Adams Jackson How much does a laryngoscope system cost?
- Bhavana K, Ahmad M, Sharma P (2018) Smartphone Otoscopy Sans Attachment: A Paradigm Shift in Diagnosing Ear Pathologies. OTO Open 2(3): 2473974X18786496.
- Koshechkin K, Lebedev G, Radzievsky G, Seepold R, Martinez NM (2021) Blockchain Technology Projects to Provide Telemedical Services: Systematic Review. J Med Internet Res 23(8): e17475.





























