Periorbital Abscess with Intracranial Complication
Ahmad Munzer Alwaa* and Saied Alhabash
Senior Consultant ENT Head & Neck Surgeon, University Hospital Sharjah, UAE
Submission: February 10, 2023; Published: February 24, 2023
*Corresponding author: Ahmad Munzer Alwaa MD, MSc, FRCS ED, FRCS (ORL-HNS), Senior Consultant ENT Head& Neck Surgeon, Head of ENT Department, University Hospital Sharjah, Clinical Assistant Professor College of Medicine University of Sharjah, United Arab Emirates
How to cite this article: Ahmad Munzer Alwaa* and Saied Alhabash. Periorbital Abscess with Intracranial Complication. Glob J Oto, 2023; 25 (5): 556171. DOI: 10.19080/GJO.2023.25.556171
Abstract
Background: Peri-orbital cellulitis secondary to rhinosinusitis is common. Peri-orbital cellulitis is a time critical condition requiring rapid assessment and management to avoid potential ophthalmological and neurological complications. However, very rarely does it present with early intracranial complications. The objective of this case report is to highlight the importance of considering intracranial and orbital cavity connections, as this may lead to intra-cranial extension.
Keywords: Peri-orbital cellulitis; Rhinosinusitis; Intracranial; Craniotomy; Antibiotics
Case Presentation
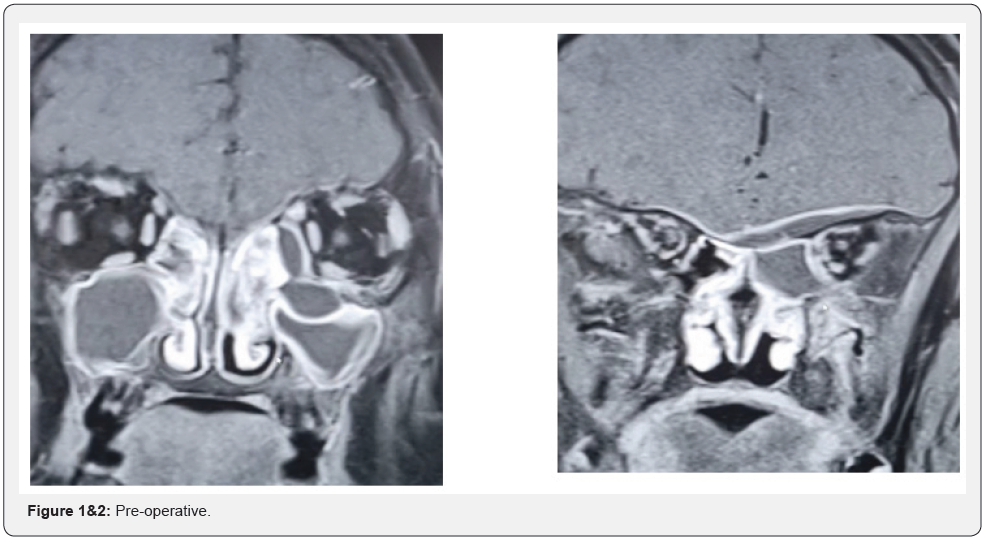
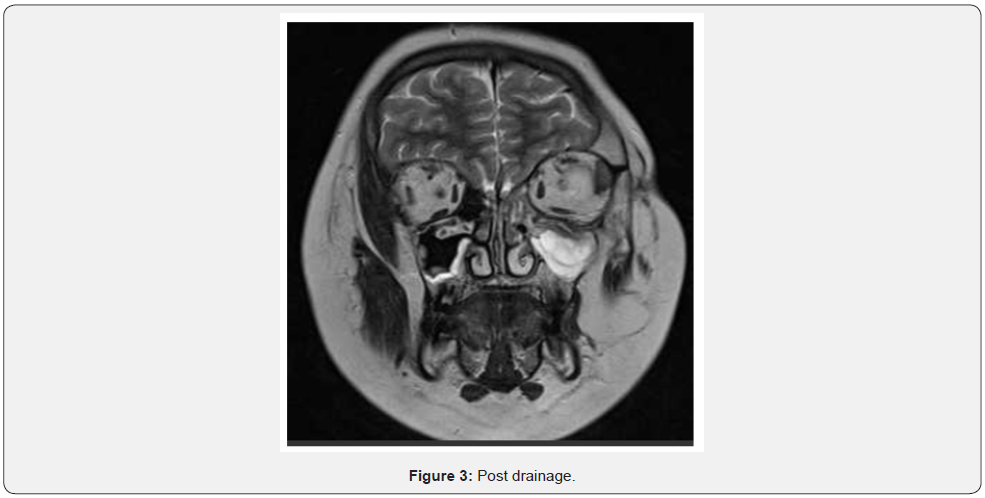
A 11-year-old boy presented with head nasal congestion and swelling lower eye lid of left eye. It was apparent from this that he had early intracranial extension of peri-orbital cellulitis (Figure 1&2). He was managed with one week of intravenous antibiotics and topical and intravenous steroids, which he responded well to. This was followed by an endoscopic drainage of the orbital sub-periosteal abscess. The intracranial collection subsequently improved on antibiotics alone, as was confirmed on a repeat enhanced computed tomography (Figure 3).
Conclusion
This case raises the importance of considering intracranial and orbital cavity connections in this age, which in this patient caused the early intracranial extension. This also suggests that spontaneous intracranial involvement can improve without requiring a craniotomy. This case exemplifies the importance of a multidisciplinary team approach and good communication in complicated case management. Furthermore, clinical improvement following medical treatment should alert the clinician to the possibility of spontaneous resolution of some cases with close monitoring, without the need for craniotomy.
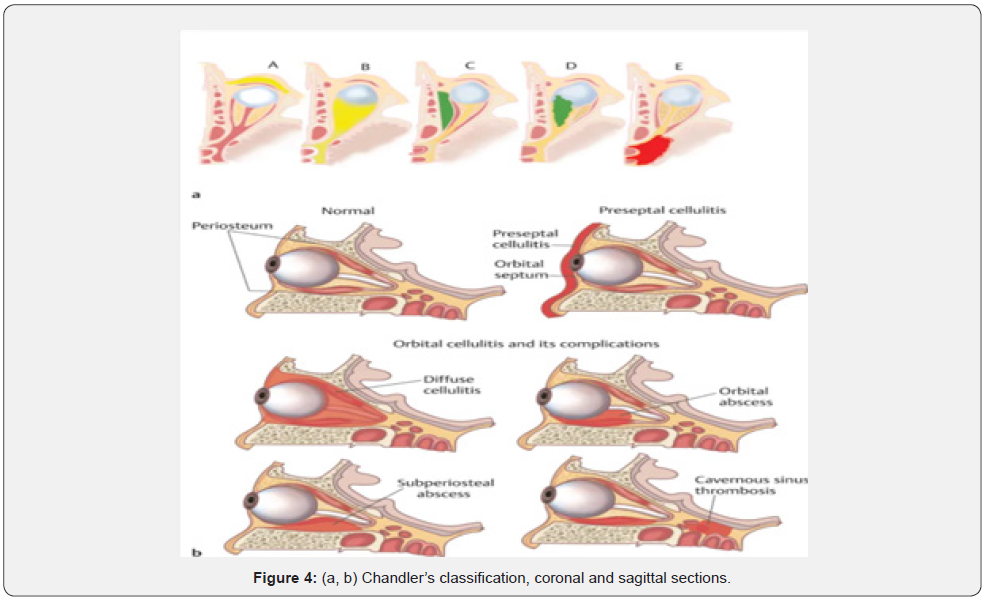
The treatment for periorbital cellulitis includes coverage for the most commonly isolated bacteria from this condition, Staphylococcus aureus, and the Streptococcus species. Most conditions of periorbital cellulitis resolve after five to seven days with proper antibiotics [1,2]. Most cases at early presentation can respond to medical treatment. There are four stages of this infection according to Chandler’s classification (Figure 4) [3].
References
- Tritt A, Kay-Rivest E, Paradis T, Duval M (2019) Daily outpatient intravenous antibiotic therapy for the management of paediatric periorbital cellulitis, a retrospective case series. Clin Otolaryngol 44(3): 273-278.
- Aryasit O, Aunruan S, Sanghan N (2021) Predictors of surgical intervention and visual outcome in bacterial orbital cellulitis. Medicine (Baltimore) 100(25): e26166.
- ACO Okonkwo, S Powell, S Carrie, SL Ball (2018) A review of periorbital cellulitis guidelines in Fifty-One Acute Admitting Units in the United Kingdom. Clin Otolaryngol 43(2): 718-721.





























