Depression Assessment in Elderly with Vestibular Vertigo
Nasrin Gohari1 and Zahra Hosseini Dastgerdi2*
1Audiology department, School of rehabilitation, Hamadan University of Medical Sciences, Iran
2Audiology department, School of rehabilitation, Isfahan University of Medical Sciences, Iran
Submission:November 19, 2022;Published:December 02, 2022
*Corresponding author: Zahra Hosseini Dastgerdi, Audiology department, School of rehabilitation, Isfahan University of Medical Sciences, Isfahan, Hezarjerib Street, Iran
How to cite this article: Nasrin G, Zahra Hosseini D. Depression Assessment in Elderly with Vestibular Vertigo. Glob J Oto, 2022; 25 (4): 556169. DOI: 10.19080/GJO.2022.25.556169
Abstract
Objective: Dizziness is one of the common complaints in the elderly. It can be caused by vestibular disorders. Depression is also prevalent in people with vestibular vertigo, and there is evidence that the two disorders are correlated. However, there is a paucity of research literature on depression and its correlation with vestibular vertigo in the elderly. No relevant studies have ever been conducted in Iran. Hence, this study aimed to analyze the correlations between depression and handicaps caused by vertigo in the elderly.
Method: This cross-sectional study was conducted on 50 elderly participants aged 60-70year old with vestibular vertigo. They made complaints about vertigo and comorbid handicaps on the Persian version of the Dizziness Handicap Inventory. Moreover, their depression degree was measured through the Persian version of the Beck Depression Short Form.
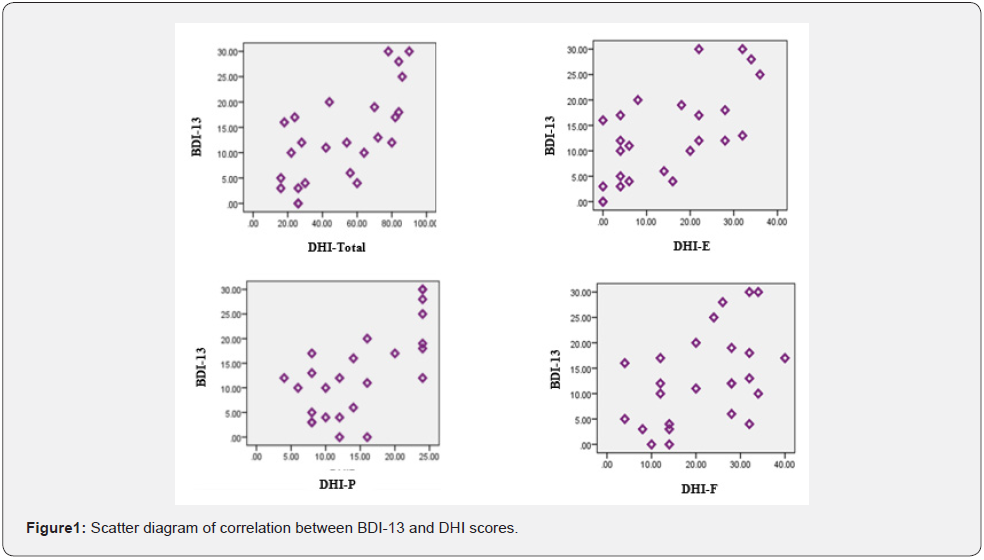
Results: According to the data, women and men accounted for 52% and 48% of the population, respectively. Their average age was 68.26±8.9 years old. The results indicated that 84% of the participants suffered from some degrees of depression. There was a significant positive correlation between the BDI-13 score and the total DHI score (r=0.663) that consisted of a physical DHI component (r=0.607), an emotional DHI component (r=0.683), and a functional DHI component (r=0.447).
Conclusion: The prevalence of depression was high in the statistical population, and there was a significant relationship between vertigo and the severity of depression.
Keywords: Elderly, Dizziness; Vertigo; Depression; DHI
Abbreviations: DHI: Dizziness Handicap Inventory; BPPV: Benign Paroxysmal Positional; VM: Vertigo and Vestibular Migraine; HADS: Hospital Anxiety and Depression Scale; MMSE: Mini-Mental State Examination; BDI-13: Beck Depression Inventory; GDS: Geriatric Depression Scale; PBN: Parabrachial Nucleus; PRN: Posterior Raphe Nucleus; LC: Locus Coeruleus
Introduction
Vertigo and other types of dizziness with vestibular origins are common complaints among the elderly [1]. Several factors may contribute to the onset of vertigo or the aggravation of this condition in the elderly such as the aging of systems related to body balance, the presence of chronic diseases related to the continuous use of drugs, and sometimes polypharmacy [2]. In addition to dizziness and vertigo, vestibular complications cause other symptoms such as imbalance as well as autonomic and neuro-vegetative symptoms in the elderly [1]. also, many patients with vestibular disorders suffer from severe emotional conditions and symptoms of anxiety and depression [1]. According to many case reports and animal studies, emotional vacillation and mood change appear in vestibular disorders in addition to movement difficulties. Moreover, vestibular syndromes are usually accompanied by cognitive-emotional symptoms in patients [3].
Different studies analyzed the correlations between vertigo and psychological complications. Their results indicated that anxiety, panic attacks, fear of loneliness, interference in daily activities, feeling of being detached from reality, depersonalization, and depressed mood were the psychosomatic consequences of vertigo caused by vestibular disorders [2, 4]. The comorbidity of vestibular problems with psychological symptoms and disorders such as depression can lead to a vicious circle and can adversely impact the effectiveness of treatment and the quality of life in the elderly [5]. Most studies analyzed the correlations between vestibular defects and the occurrence of psychological disorders such as depression and anxiety in the youth and adult populations. Furthermore, vestibular dysfunction can be a major cause of emotional disorders (e.g., anxiety and depression) [5]. There are inadequate studies on the comorbidity of depression with vestibular vertigo in the elderly. The results mostly report the prevalence of psychological disorders and their different types in the elderly with vertigo. However, nothing has been reported with regard to the correlation between the vertigo-caused handicaps and the severity of psychological disorders such as depression.
Peluso, Quintana, and Gananca reported that the prevalence rates of depression cases in the elderly with chronic dizziness of the vestibular causes were 45.4% during life and 11.3% in the last 12 months [1]. Gazzola analyzed the factors of depression symptoms among the elderly with chronic vestibular defects and reported that nearly 55.8% of the participants had depression symptoms. According to the results, various factors such as memory and concentration disorders, insomnia, hearing disorders, very poor vision, female gender, and negligence to use walking aids worsened the severity of depression symptoms in the elderly [1]. Zhu et al. [6] analyzed the handicaps caused by vertigo and anxiety depression in patients with benign paroxysmal positional vertigo (BPPV) and vestibular migraine (VM). They reported that the emotional, functional, and physical effects of vertigo were greater on VM patients than on BPPV patients. Variations in the DHI scores of BPPV and VM patients were positively correlated with changes in anxiety and depression measured through the hospital anxiety and depression scale (HADS). In other words, more attention must be paid to the mental states of patients as the severity of vertigo increases [6].
Given that vertigo with vestibular causes and psychological disorders (e.g., depression) are common complaints in the elderly population. These conditions have negative effects on all aspects of their lives and health [1]. Moreover, the evaluation and management of clinical conditions in the elderly are different from those of other age groups. Thus, it is necessary to analyze the correlation between depression and vestibular vertigo in the elderly in a bid to provide optimal evaluation and intervention solutions. This study aimed to assessment the correlations between vestibular vertigo and resultant handicaps as well as the severity of depression in the elderly.
Material and Method
Participants
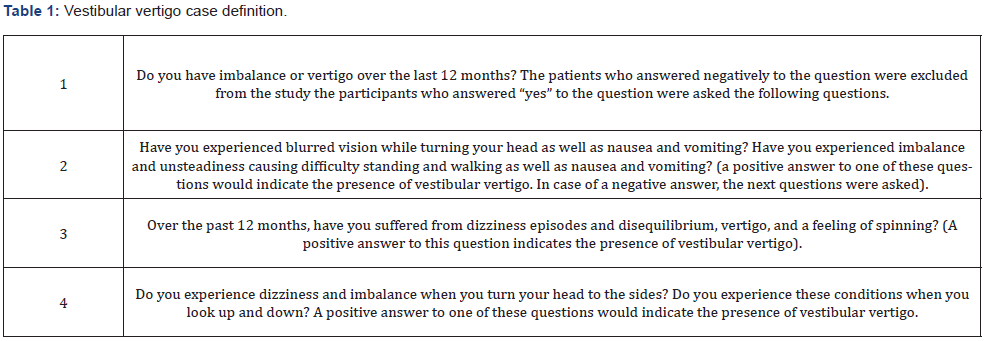
The statistical population included 50 elderly participants aged 60-70 years with vestibular vertigo. Their diagnosis of vertigo was based on standard flowchart for determining vestibular vertigo developed by Albathi and Agrawal diagnosis of otorhinolaryngologist. This flowchart was adapted from the 2008 National Health Interview Survey. Its Questions are listed in (Table 1) [7]. Cause of vertigo diagnosed, 17 of the participants had Benign Paroxysmal Positional Vertigo (BPPV), 16 unilateral and bilateral reduced vestibular response, and 6 delayed endolymphatic hydrops, 3 trauma, 3 sudden deafness and vertigo, 3 vestibular neuronitis, 2 Labyrinthitis by otorhinolaryngologist based on examination of elderly and their medical records. The participants were selected through convenience sampling from daily care elderly centers in Hamadan. They were then asked for written consent forms for participation in the study. The inclusion criteria were as follows: being aged above 60 years old, having vestibular vertigo in accordance with its standard definition based on the NHIS flowchart [7], having no cognitive disorders, having a score above 25 in the mini-mental state examination (MMSE) [8], not receiving vestibular rehabilitation, and having no history of communication problems and neurological disorders, no serious metabolic disorders that require medication, and no cardiovascular disorders.
Evaluations
After the participants were selected in accordance with the inclusion criteria, the dizziness handicap inventory (DHI) and the Beck depression inventory (BDI-13) were both completed with one of the authors. The following subsections concern the questionnaires and the methods of calculating their scores.
Persian Version of Dizziness Handicap Inventory (DHI)
The Persian version of the DHI contains 25 items aimed at analyzing the outcomes of vestibular and balance disorders. The total score ranges from 0 (no handicaps) to 100 (severe handicaps). This inventory includes three subscales called physical (DHI-P), emotional (DHI-E), and functional (DHI-F) components. In its original version, a total score below 14 criteria would be considered normal. In the Persian version, a cutoff point of 10 with 100% sensitivity and specificity can be used to distinguish normal people with no handicaps from people with dizziness handicaps [9]. The internal consistency of DHI-P was good, the Cronbach’s alpha was 0.79, 0.82, 0.83, and 0.90 for total and emotional, physical and functional subscales; respectively, in reliability, There was a high correlation between test re-test scores (r = 0.90) (19).
Persian Version of Shortened Beck Depression Inventory
The 13-item short form of the BDI-13 was developed to facilitate rapid implementation in clinical and research settings. This 13-item short-form depression inventory includes 13 self-report statements that express the specific symptoms of depression. It was compiled through the study of the original 21-item developed by Beck et al. in 1961. In fact, Beck et al. [10] reported the correlation between the 21-item form and the 13- item short form from 0.89 to 0.97 and introduced the short form as an acceptable substitute for the long form [10]. Lightfoot and Oliver reported Cronbach’s alpha of BDI-13 at 0.87 and with a reliability score of 0.9 after two weeks [11]. In Iranian cases, Cronbach’s alpha ranged from 0.89 to 0.94 [12]. The inventory scores were classified as normal cases (0-3), mild depression (4- 7), mild-to- average depression (8-11), average depression (12- 15), and severe depression (16-39) [12].
Statistical Analysis
The statistical analysis was performed in SPSS 23 (IBM, Armonk, NY, USA). The mean (±standard deviation) and quantity (percentage) were used for descriptive analysis. The Kolmogorov- Smirnov test was employed to check the data normality, whereas the Spearman’s rank-order correlation was utilized to analyze the data correlation. The significance level was considered 0.05.
Results
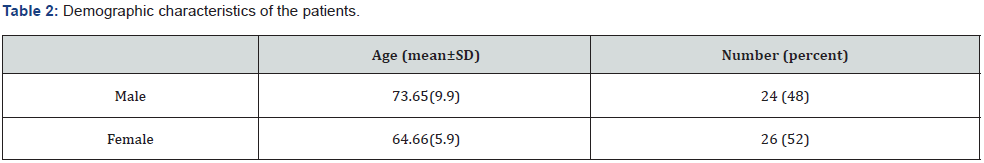
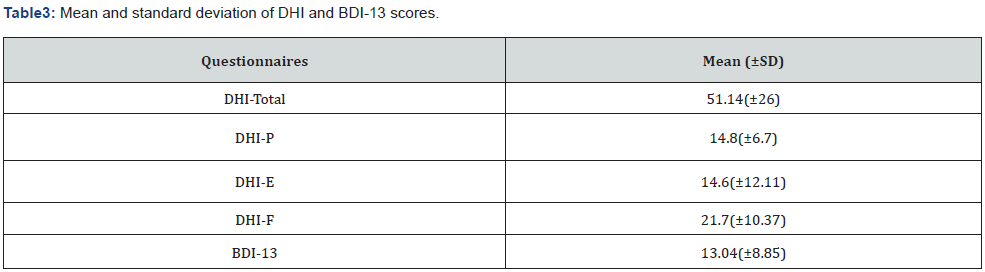
The statistical population included 50 elderly participants with vestibular vertigo. (Table 2) demonstrates their demographic information. (Table 3) presents the average scores of the DHI, its subscales, and the BDI-13. According to the BDI-13 scores, participants were classified as mild-to-moderate depression cases on average. The distribution of depression in 50 people was as follows: 8 normal cases (16%), 7 mild depression cases (14%), 6 mild-to-moderate depression cases (12%), 9 moderate depression cases (18%), and 20 severe depression cases (40%). (Table 4) reports the results of correlations between DHI and BDI- 13 scores. Accordingly, BDI-13 scores had significant correlations with the total DHI score (r=0.663, p<0.001) as well as DHI-P (r=0.607, p<0.001), DHI-E (r=0.683, p<0.001), and DHI-F (r=0.447, p=0.001). In other words, the handicap scores of dizziness and those of physical, emotional, and functional dimensions increased as depression worsened. The relationship between BDI-13 and DHI scores is shown in (Figure1).
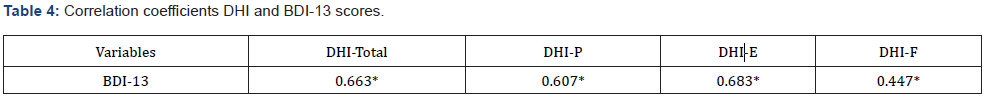
*Correlation is significant at the 0.01 level (two-tailed).
Discussion
According to the analysis of results, the prevalence of depression in the elderly with vestibular vertigo was high. There was a significant correlation between the severity of depression and handicaps caused by vertigo. The findings are discussed below.
Analysis of Dizziness Handicap Inventory Scores in the Elderly with Vestibular Vertigo
According to the demographic information, most of the participants were female. This is consistent with the higher prevalence rates of dizziness and vestibular disorders among women [2]. In the statistical population, the average DHI score indicated moderate handicaps [13]. Vertigo is among the most important disabling medical conditions in which handicaps worsen as patients age [14]. In fact, vertigo-related disorders become increased with age; and also, functional handicaps are exacerbated. This study did not analyze the cause of vestibular vertigo with diagnosis systems include video nystagmogrphy and video head impulse test. However, BPPV had a high prevalence rate among other vestibular disorders in the elderly population (nearly a third of the causes of vertigo in this population are related to BPPV) according to the otorhinolaryngologist diagnosis. Considering the moderate DHI scores, the DHI scores greater than or equal to 50 in the elderly with vertigo were identified as good predictors of BPPV [15]. In the present study, BPPV was diagnosed in most of the participants (DHI score: 51.14±26). Saxena and Prabhakar reported that the DHI score was higher in the elderly with BPPV than in other vestibular cases [15].
Analyzing Prevalence and Severity of Depression in the Elderly with Vestibular Vertigo
According to the results of analyzing the prevalence of depression through the BDI-13, 84% of the elderly in the population suffered from some degrees of depression. On average, the severity of depression in the population was moderate, and 40% of the elderly had severe depression. The prevalence of depression cases was much higher in this study than in other studies. Gazzola et al. [1] analyzed the causes of depression symptoms in 120 elderly participants with chronic vestibular defects. They reported that 55.8% of the population scored above the cutoff point, something which indicated the presence of depressed moods among their participants [1]. In another study in 2016, the prevalence was 45.5% in 44 elderly participants with chronic dizziness of vestibular causes with moderate-to-severe depression symptoms [2].
Many factors such as gender, literacy level, retirement, presence of chronic disorders, memory and concentration disorders, insomnia, and hearing impairment can affect the prevalence and severity of depression in the elderly population with chronic vestibular defects. These factors can cause heterogeneity in the statistical population as well as inconsistency in the results of different studies [1, 2]. According to Gazzola, a higher number of depression symptoms among the elderly with chronic vestibular disorders had been related to the presence of memory and concentration disorders, insomnia, hearing disorders, very poor vision as well as greater emotional effects of dizziness, femininity, and non-use of walking aids [1]. In this study, 52% of the participants were women. Furthermore, the participants had no cognitive impairments, thereby having no difficulty communicating with the interviewer.
In a study by Peluso, 88.6% of the participants were women, a rate which is higher than that of the present study. Although there are fewer women in the present study than in Peluso’s, the prevalence of depression was higher. This difference is probably associated with the other determinants of depression in the elderly population with vestibular vertigo. Peluso considered other factors such as the level of literacy, employment status, and marital status, which were not analyzed in our study. In addition, different definitions of depression and the use of various tools to define the presence and extent of depression can be considered the causes of contradictory results. In the present study, depression was measured through the BDI-13, which is different from the criteria used in the other two studies, i.e., the Brazilian version of the Composite International Diagnostic Interview Version 2.1 (CIDI 2.1) in Peluso’s study and the Geriatric Depression Scale (GDS) in Gazzola’s study [1, 2].
Analyzing Correlations between Depression and Vertigo-Caused Handicaps in the Elderly with Vestibular Vertigo
Among other results of this study, there were moderate positive correlations between the severity of depression and the DHI scores. The correlations between psychological complications such as depression and anxiety and vestibular disorders (Meniere’s, VM, and BPPV) were confirmed in the young-to-elderly age groups [6]. Conducting a comprehensive analysis of NHIS data on 20,950 adults above the age of 18, Bigelow (2015) reported that vestibular vertigo, cognitive impairment, and psychiatric disorders were correlated consistently. In the analysis of their findings, they indicated that people with vestibular vertigo were three times more vulnerable to depression, anxiety, or panic attacks than the general population. Furthermore, their mental disorders were moderate [16]. There are also complex interactions between the vestibular system and psychological disorders. In other words, vestibular vertigo can cause psychological complications and complaints such as depression.
According to research findings, vestibular stimulation is effective in reducing psychological problems [3]. Evidence also shows that vestibular activities decrease in emotional disorders such as depression [17]. Moreover, emotional disorders aggravate vestibular symptoms [3]. Patients avoid activities that are associated with vertigo due to the unpleasant feeling of vertigo or anxiety over the possibility of physical harm or social embarrassment. Unfortunately, this avoidance behavior can actually worsen dizziness and psychotic symptoms [18]. The elderly with vestibular disorders experience various psychological complications such as panic attacks, anxiety, and depression more often than other young people and adults due to personal and social limitations caused by dizziness and other symptoms of vestibular disorders as well as the inability to compensate for these limitations [1].
The neural mechanisms for the correlations between vertigo and psychiatric disorders are still unclear. However, these connections are apparently due to the significant overlap of anatomical neural regions and neurotransmitters involved in the vestibular system and pathways of emotional processing [16]. According to the research evidence, the vestibular system is correlated with cortical and subcortical structures of anxiety [3]. According to the Balaban model, the parabrachial nucleus (PBN) is among the major structures located in a strategic position on the path of sensorimotor information. It seems to be the anatomical location that connects vestibular defects and psychological problems. The posterior raphe nucleus (DRN) and locus coeruleus (LC) are among the other neurotransmitter structures and the nuclei affecting emotional reactions, vestibular structures, and balance [3].
One of the limitations of this study was no checking of all disorders and mental and social conditions of the elderly. Many factors in old age can lead to depression. Various studies have shown that older age, being female, marital loss, presence of known chronic disease, and poor social support were contributing factors for depression in elderly [19]. Since there are several disorders in the elderly at the same time, it is not possible to find a group that only has a vestibular disorder, so it is recommended to carry out evaluations in younger people to reduce confusing disorders.
Conclusion
The prevalence of depression was very high in the elderly with vestibular vertigo. In fact, the severity of depression was correlated with the total DHI score and its subscales. These results are very disturbing and thought-provoking in the statistical population, thereby highlighting the need for a more comprehensive study on a larger sample size by considering all factors causing and aggravating depression in the elderly with vestibular vertigo. It is also recommended to consider psychological complications such as depression in the evaluation and intervention plans adopted to treat the elderly with vertigo. In other words, depression should be regarded as a major factor in the rehabilitation of the elderly, their quality of life, and their life expectancy.
Acknowledgments
We warmly appreciate the esteemed officials of Hamadan Welfare Organization and the directors of Khorshid daily care centers, Ms. Naderi Movahed, Hamian Mehr Center, Ms. Heshmati, and Habib Ibn Mazaher Center, Mr. Mahmoudian, as well as all the participants in this study.
References
- Gazzola JM, Mayra CA, Flavia D, Camila M, MM Fukujima, et al. (2009) Factors related to depressive symptoms in elderly people with chronic vestibular dysfunction. Archives of Neuropsychiatry 67(2b): 416-422.
- Peluso ETP, MI Quintana, FF Ganança (2016) Anxiety and depressive disorders in elderly with chronic dizziness of vestibular origin. Braz J Otorhinolaryngol 82(2): 209-214.
- Hilber P, Jan C, Anne LG, Marie-Laure M, Jan T, et al. (2019) Cooperation of the vestibular and cerebellar networks in anxiety disorders and depression. Prog Neuropsychopharmacol Biol Psychiatry 89: 310-321.
- Yardley L (2000) Overview of psychologic effects of chronic dizziness and balance disorders. Otolaryngol Clin North Am 33(3): 603-616.
- Yuan Q, Lisheng Y, Dongmei S, Xingxing K, Hua Z (2015) Anxiety and depression among patients with different types of vestibular peripheral vertigo. Medicine 94(5): e453.
- Zhu C, Yiqing L, Yi J, Xingquan Z (2020) Dizziness handicap and anxiety depression among patients with benign paroxysmal positional vertigo and vestibular migraine. Medicine 99(52): e23752.
- Albathi M, Yuri A (2017) Vestibular vertigo is associated with abnormal sleep duration. J Vestib Res 27(2-3): 127-135.
- Seyedian M, M Falah, M Nourouzian, S Nejat, A Delavar, et al. (2008) Validity of the Farsi version of mini-mental state examination. ScienceOpen.
- Jafarzadeh S, Eshagh B, Akram P, Shohreh J, Ahmad D (2014) Validity and reliability of the Persian version of the dizziness handicap inventory. J Res Med Sci 19(8): 769-775.
- Beck AT, WY Rial, K Rickels (1974) Short form of depression inventory: cross-validation. Psychol Rep 34(3): 1184-1186.
- Lightfoot SL, J Oliver (1985) The Beck Inventory: Psychometric properties in university students. J Pers Assess 49(4): 434-436.
- Dadfar M, Z Kalibatseva (2016) Psychometric properties of the persian version of the short beck depression inventory with Iranian psychiatric outpatients. Scientifica 2016: 8196463.
- Treleaven J (2006) Dizziness handicap inventory (DHI). Aust J Physiother 52(1): 67.
- Wassermann A, S Finn, H Axer (2022) Age-associated characteristics of patients with chronic dizziness and vertigo. J Geriatr Psychiatry Neurol 35(4): 580-585.
- Saxena A, MC Prabhakar (2013) Performance of DHI score as a predictor of benign paroxysmal positional vertigo in geriatric patients with dizziness/vertigo: a cross-sectional study. PloS one 8(3): e58106.
- Bigelow RT, YR Semenov, Sascha L, Howard JH, Y Agrawal (2016) Vestibular vertigo and comorbid cognitive and psychiatric impairment: the 2008 National Health Interview Survey. J Neurol Neurosurg Psychiatry 87(4): 367-372.
- Soza AM, B Certanec, E Tapia (2018) Abnormal vestibular asymmetries in patients with major depression. J Clin Trials Nerv Syst Dis 3(2): 1-7.
- Best C, A Eckhardt-Henn, Regine T, Marianne D (2009) Psychiatric morbidity and comorbidity in different vestibular vertigo syndromes. Results of a prospective longitudinal study over one year. J Neurol 256(1): 58-65.
- Mulat N, H Gutema GT Wassie (2021) Prevalence of depression and associated factors among elderly people in Womberma District, north-west, Ethiopia. BMC psychiatry 21(1): 1-9.





























