Unusual Site of Langerhans Cell Histiocytosis Involving Nasopharynx
Lulwah Sami Alturki1*, Nasser Waleed Alobida1, Mohammad Alwatban2, Nader Alhejaily3 and Ameen Binnasser1
1Department of Otolaryngology-Head and Neck Surgery, King Fahad Medical City, Saudi Arabia
2Department of Radiology, Imam Abdulrahman Bin Faisal University, Saudi Arabia
3Department of Pathology, Prince Sultan Military Medical City, Saudi Arabia
Submission: August 05, 2021; Published: August 19, 2021
*Corresponding author: Lulwah Sami Alturki, Department of Otolaryngology-Head and Neck Surgery, King Fahad Medical City, Riyadh, Saudi Arabia
How to cite this article: Lulwah S A, Nasser W A, Mohammad A, Nader A, Ameen B. Unusual Site of Langerhans Cell Histiocytosis Involving Nasopharynx. Glob J Oto, 2021; 24 (4): 556145. DOI: 10.19080/GJO.2021.24.556145
Abstract
Langerhans cell histiocytosis (LCH) is a rare proliferative disorder that originates from myeloid-derived precursor dendritic cell, not the Langerhans cell in the skin. The etiology and subsequent development of LCH are idiopathic and not well understood. A 28-day full term baby girl referred her to high tertiary care center due to mass in nasopharynx for further management. Patient was intubated with normal size tube in low sitting mode, no facial dysmorphic feature, fiberoptic nasal scope showed patent nasal cavity bilaterally, mass was encountered at the lower end of nasopharynx with normal covering mucosa. MRI brain and sinuses with contrast demonstrates a single relatively well-defined mass, its epicenter seen at the nasopharynx posterior wall. Its showing extension to the adjacent osseous structures including C1 anterior arch, inferior clivus and bilateral occipital condyle. Transoral biopsy done in the operating room under general anesthesia which confirm the diagnosis of LCH. Case was discussed in the pediatric tumor board, and it was decided to start her on Vinblastine and prednisolone. Patient received Vinblastine 6 mg/m2 IV weekly bolus for 6 weeks, with systemic prednisone 40 mg/m2/day in three divided doses for 4 weeks and then tapered over the following 2 weeks. A follow-up FDG PET was performed for the whole body and MRI of head and neck Interval improvement of the nasopharyngeal and clival mass without significant residual, no enlarged or suspicious cervical lymph nodes. LCH is a rare condition and prevalent among early age group. Occur in any part of body including nasopharynx and oropharynx.
Keywords: Langerhans’cell; Histiocytosis; Nasopharynx
Introduction
Langerhans cell histiocytosis (LCH) is a rare proliferative disorder that originates from myeloid-derived precursor dendritic cell, not the Langerhans cell in the skin [1,2]. The estimated annual incidence of LCH in children are four to eight per million [3-5]. The etiology of LCH is unknown and there has been considerable debate whether LCH represents an inflammatory or a neoplastic disease. The discovery of recurrent mutations in the mitogen activated protein kinase (MAPK) pathway (i.e., BRAF and MAP2K1 mutations) indicates that it is a neoplastic disease [6,7]. The clinical presentation is variable and ranging from localized single-system involvement to disseminated life-threatening multisystem disease [8]. The purpose of reporting this case in a 28-day old baby is that it is rare and unusual site of LCH involving the nasopharynx.
Case Report
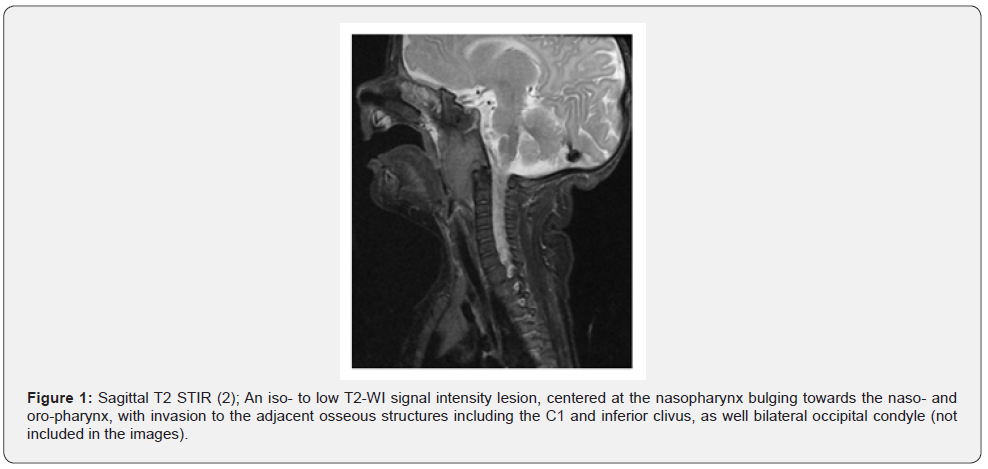
Full term baby girl delivered Lower segment caesarean section with good APGAR score. Patient was intubated immediate after birth with normal size tube due to respiratory distress for few days then extubated, on day six reintubated due to respiratory issue. Seen by the ENT team and recommended to do CT scan of head and neck to rule out congenital malformation as baby unable to wean off from ventilation. CT scan showed mass in nasopharynx, so they referred her to high tertiary care center for further management. The case was referred to a tertiary care center, King Fahad Medical City (KFMC) and admitted in NICU. They consulted our Pediatric Otolaryngology service to evaluate the 28 days full term baby girl, with no known medical illnesses, prenatal history was unremarkable. patient was intubated with normal size tube in low sitting mode, no facial dysmorphic feature, examination of oral and oropharynx reveled soft mass in posterior pharyngeal wall causing narrowing of the pharynx. Fiberoptic nasal scope showed patent nasal cavity bilaterally, mass was encountered at the lower end of nasopharynx with normal covering mucosa with no ulceration or discharge. MRI brain and sinuses with contrast demonstrates a single relatively well-defined mass, its epicenter seen at the nasopharynx posterior wall. Its showing extension to the adjacent osseous structures including C1 anterior arch, inferior clivus and bilateral occipital condyle Figure 1.
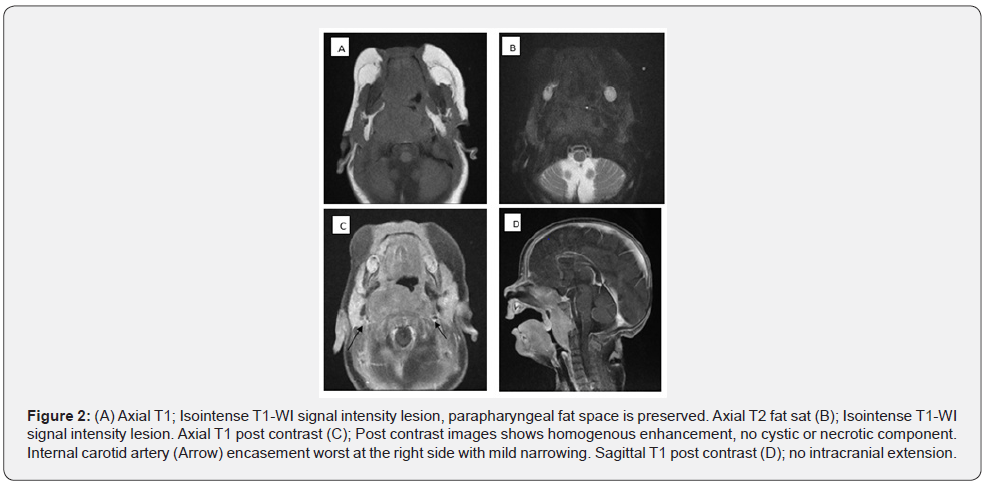
The lesion demonstrates homogenous iso T1-WI and intermediate to low T2-WI signal intensity, with enhancement and some restricted diffusion, Figures 1&2. No calcification or hemorrhage, and no cystic or necrotic component. The mass is bulging towards the nasopharynx leading to complete obstruction together with mild obstruction of the oropharynx Figure 1. The parapharyngeal fat is intact. The hypopharynx is clear. No intracranial extension. There is encasement of both internal carotid arteries most significant at the right side, Figure 2. No enlarged cervical lymph nodes. The brain MRI scan was normal, without underlying lesion or abnormal enhancement.
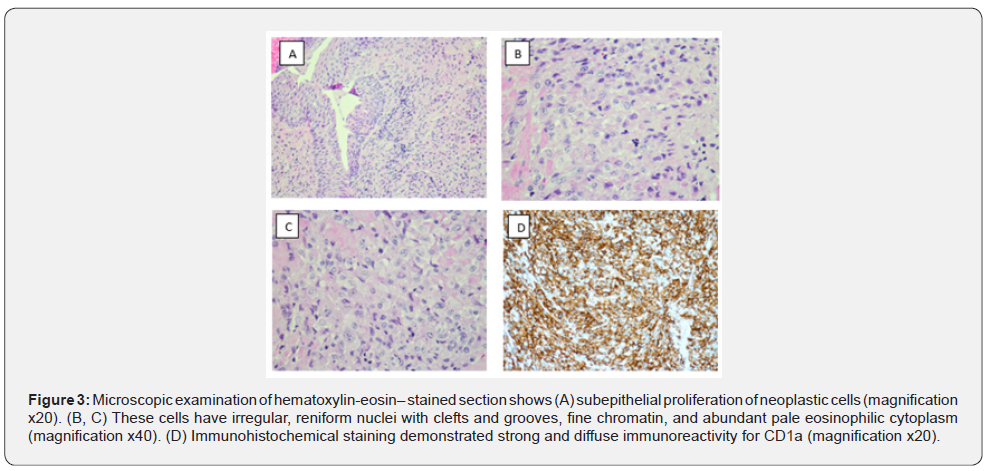
After discussing the case between multiple teams, the plan was to perform transoral biopsy in the operating room under general anesthesia, biopsy taken and send for histopathology which confirms the diagnosis of LCH Figure 3. The patient’s case was discussed in the pediatric tumor board, and it was decided to start her on Vinblastine and prednisolone. Patient received Vinblastine 6mg/m2 IV weekly bolus for 6 weeks, with systemic prednisone 40 mg/m2/day in three divided doses for four weeks and then tapered over the following two weeks. A follow-up FDG PET was performed for the whole body and MRI of head and neck Interval improvement of the nasopharyngeal and clival mass without significant residual, No enlarged or suspicious cervical lymph nodes.
Discussion
LCH is a rare condition, and it presents clinically in different ways. The etiology and subsequent development of LCH are idiopathic and not well understood. It is suggested that this disease might be seriously affected by predisposing factors that are viral or genetic. However, here's no conclusive prove for it [9]. The clinical presentation of LCH is highly heterogeneous. LCH may involve many organs (skin, bone, central nervous system, spleen, lungs, liver, or gastrointestinal tract) [10]. Definitive diagnosis depends on the identification of characteristic immunohistochemical (IHC) or ultrastructural features of the biopsy specimen [11]. Langerhans cells show strong positivity by IHC studies for S100 protein and CD1a [12]. The optimal management requires interdisciplinary collaboration between specialists (oral surgeon, dentist, ENT, radiologist, pathologist, and oncologist)[13].
In our case report biopsy were necessary to diagnose the patient’s condition, which shows a subepithelial proliferation of neoplastic cells with irregular, reniform nuclei with clefts and grooves, fine chromatin, and abundant pale eosinophilic cytoplasm. The cells are admixed with varying proportions of eosinophils and other inflammatory cells. Immunohistochemical staining demonstrated strong and diffuse immunoreactivity for CD1a, S100 and CD68 confirming the diagnosis of LCH Figure 3. Highlighting the challenge of radiology including MRI which can give various differential diagnosis. Manifestations of LCH in nasopharynx and oropharynx regions in Literatures are limited and mostly consists of case reports or retrospective series [14]. In severe cases with systemic LCH presentations, chemotherapy improves the outcome, however due to the rareness of the disease, it is still unclear which ways are best suited for different clinical situations [13]. In our case, the patient received six cycles chemotherapy with no relapsing after three months.
Conclusion
LCH is a rare condition and prevalent among early age group. Occur in any part of body including nasopharynx and oropharynx. Multidisciplinary team need to reach the diagnosis and treatment.
References
- Davies H, Bignell G R, Cox C, Stephens P, Edkins S, et al. (2002) Mutations of the BRAF gene in human cancer. Nature 417(6892): 949-954.
- Allen C E, Li L, Peters T L, Leung H E, Yu A, et al, (2010) Cell-Specific Gene Expression in Langerhans Cell Histiocytosis Lesions Reveals a Distinct Profile Compared with Epidermal Langerhans Cells. J Immunol 184(8): 4557-4567.
- A Guyot Goubin, J Donadieu, M Barkaoui, S Bellec, C Thomas, et al. (2008) Descriptive epidemiology of childhood Langerhans cell histiocytosis in France, 2000-2004. Pediatr Blood Cancer 51(1): 71-75.
- J A Salotti, V Nanduri, M S Pearce, L Parker, R Lynn, et al. (2009) Incidence and clinical features of Langerhans cell histiocytosis in the UK and Ireland. Arch Dis Child 94(5): 376-380.
- H Stålemark, E Laurencikas, J Karis, D Gavhed, B Fadeel, J I Henter, (2008) Incidence of Langerhans cell histiocytosis in children: A population-based study. Pediatr Blood Cancer 51(1): 76-78.
- Brown N A, Furtado L V, Betz B L, Kiel M J, Weigelin H C. et al. (2014) High prevalence of somatic MAP2K1 mutations in BRAF V600E-negative Langerhans cell histiocytosis. Blood 124 (10): 1655-1658.
- Badalian Very G, Vergilio J A, Degar B A, MacConaill L E, Brandner B, et al. (2010) Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood 116(11): 1919-1923.
- Broadbent V, Gadner H (1998) Current therapy for Langerhans cell histiocytosis”. Hematol Oncol Clin North Am 12(2): 327-338.
- Alhaidri NE, Alim B, Alrushaid NR, Fatani H, Binnasser AS (2021) Temporal Bone Langerhans Cell Histiocytosis: An Uncommon Bilateral Presentation. Cureus 13(1): e12732.
- D J Glotzbecker MP, Carpentieri DF (2002) Langerhans cell histiocytosis: Clinical presentation, pathogenesis, and treatment from the LCH etiology research group at the children’s hospital of Philadelphia. Univ Pennsylvania Orthop J 15: 67-73.
- J Marquet, F Declau, M De Cock, K De Paep, B Appel, et al. (1988) Congenital middle ear malformations. Acta Otorhinolaryngol Belg 42(2): 117-302.
- M Edelweiss, L J Medeiros, S Suster, C A Moran (2007) Lymph node involvement by Langerhans cell histiocytosis: a clinicopathologic and immunohistochemical study of 20 cases. Hum Pathol 38 (10): 1463-1469.
- J Luz, D Zweifel, M Hüllner, M Bühler, M Rücker, B Stadlinger (2018) Oral manifestation of Langerhans cell histiocytosis: A case report. BMC Oral Health 18(1): 106.
- H Nomori, S Watanabe, T Nakajima, Y Shimosato, T Kameya (1986) Histiocytes in nasopharyngeal carcinoma in relation to prognosis. Cancer 57(1): 100-105.





























