Paranasal Sinus Phaeohyphomycosis: A Case Report and Literature Review
Karthikeyan R1, Kezevino Nagi2*, Arun Alexander3, Sivaraman Ganesan5 and Sunil Kumar Saxena4
1 Senior Resident, Department of ENT, JIPMER, India
2Junior Resident, Department of ENT, JIPMER, India
3 Professor, Department of ENT, JIPMER, India
4 Senior Professor & HOD, Department of ENT, India
5Associate Professor, Department of ENT, India
Submission:July 08, 2020; Published:August 17, 2020
*Corresponding author:Kezevino Nagi, Junior Resident, Department of ENT JIPMER, Puducherry, India
How to cite this article: Karthikeyan R, Kezevino N, Arun A, Sunil K S, Sivaraman G, Sunil K S. Paranasal Sinus Phaeohyphomycosis: A Case Report and Literature Review. Glob J Oto, 2020; 23 (2): 556107 DOI: 10.19080/GJO.2020.23.556107
Abstract
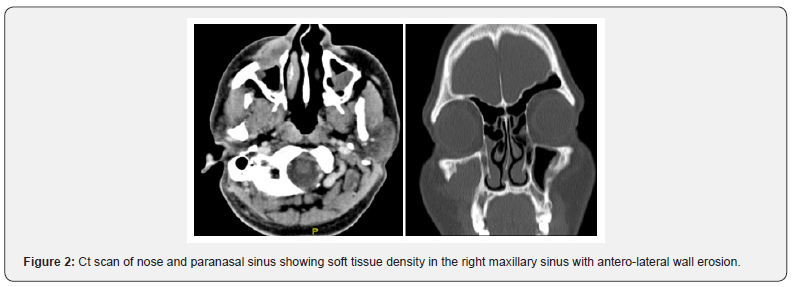
Fungal infections of the paranasal sinuses manifest from simple colonization (Eg: fungal ball) to invasive forms (Eg: Rhizopus: Mucor) depending on the immune status of the host. Infection with lesser-known species like dermatophyseal fungus has been rarely reported in the literature. We report a rare case of Paranasal sinus phaeohyphomycosis in a 30-year-old immunocompetent male presenting to our tertiary care centre with right cheek swelling of 1-year duration with CT showing homogeneously enhancing soft tissue density in the right maxillary sinus with erosion of the anterolateral wall. FNAC revealed pseudo septate, bulbous pigmented fungal hyphae which resolved with surgical debridement and antifungal therapy for 6 weeks.
Keywords: Fungal sinusitis; Phaeohyphomycosis; Paranasal sinus
Introduction
Phaeohypomycosis is a chronic infectious condition caused by dematiaceous or “melanised” fungi which commonly involves the skin and subcutaneous tissue [1]. Usual clinical manifestations are subcutaneous abscess or cystic swelling [1]. Phaeohyphomycosis is of rare occurrence in the paranasal sinus and in patients who are immune-competent [2]. Here is a case study of a 30-year-old immunocompetent male patient with dermatophyseal fungal infection of the paranasal sinus.
Case Report
A 30-year-old immune-competent male presented to our outpatient clinic with c/o Right cheek swelling for 1-year duration with no other nasal complaints. He gives history of previous Endoscopic Sinus surgery 1 year ago for sinusitis at a private hospital. O/E He had a diffuse, non-tender, hard swelling in the right cheek region with no skin changes or paraesthesia. Nasal Endoscopy was normal.
Haematological and blood biochemistry were within normal limits. Serological tests for HIV types I and II were non-reactive. Fine needle aspiration cytology (FNAC) revealed a well-formed epithelioid granuloma, many multinucleate foreign body type giant cells containing pseudo septate, bulbous pigmented fungal hyphae compatible with phaeohyphomycosis. Computed Tomography (CT) showed soft tissue density in the right maxillary sinus with erosion of the anterolateral wall.
Under general anaesthesia, he underwent a Caldwell Luc procedure and disease clearance was done. Intraoperatively: there was a defect in the anterolateral wall with fungal debri noted in the subcutaneous plane and the right maxillary sinus cavity. He was started on Tab Itraconazole and continued for 6 weeks postoperatively.
Discussion
Phaeohyphomycosis are fungal infections caused by fungi with dark hyphae, which appear as melanized filament [3]. At present, Coniosporium, Cyphellophora, Fonsecaea, Phialophora Exophiala, Rhinocladiella and Cladophialophora species are the most clinically relevant dematiaceous fungi worldwide [3]. Phaeohyphomycosis represents a broad range of primary and opportunistic mycoses [4] classified into four clinical forms, which includes superficial, cutaneous, systemic, and dissemination [5]. Paranasal sinus phaeohyphomycosis is a rare infection [6], and immunocompromised state is not a pre-requisite [7] as observed in our patient [4]. From the present case study, we highlight that any patient with subcutaneous swelling in the cheek with CT finding of erosion of sinus we should consider dermatophyseal fungal infection as one of the differential diagnosis in an immunocompetent patient with no other risk factors(Diabetes mellitus/hypertension/ immunosuppressant therapy etc). Surgical clearance of the disease with antifungal therapy [6] for atleast 6 weeks duration has shown to have near-complete response as seen in our patient. Patient is still under follow-up [8].


Conclusion
This is a rare case report of a Paranasal sinus phaeohyphomycosis in an immunocompetent patient. Highlighting that any patient with subcutaneous swelling in the cheek with CT finding of erosion of sinus we should consider dermatophyseal fungal infection as one of the differential diagnosis in an immunocompetent patient with no other risk factors(Diabetes mellitus/hypertension/ immunosuppressant therapy etc).
References
- Arcobello JT, Revankar SG (2020) Phaeohyphomycosis. Semin Respir Crit Care Med 41(01): 131-140.
- Mehta SA, Kaul S, Mehta MS, Kelkar RS, Mehta AR (1993) Phaeohyphomycosis of the paranasal sinuses masquerading as a neoplasm: A case report. Head Neck 15(1): 59-61.
- Huang C, Zhang Y, Song Y, Wan Z, Wang X, Li R (2019) Phaeohyphomycosis caused by Phialophora Americana with CARD9 mutation and 20‐year literature review in China. Mycoses 62(10): 908-919.
- Rai S, Sandhu S, Rajkumar Y, Tiwari R (2012) Hyalohyphomycosis of maxillary antrum. J Oral Maxillofac Pathol 16(1): 149.
- Chintagunta S, Arakkal G, Damarla S, Vodapalli A (2017) Subcutaneous phaeohyphomycosis in an immunocompetent Individual: A case report. Indian Dermatol Online J 8(1): 29.
- Ben Ami R, Lewis RE, Raad II, Kontoyiannis DP (2009) Phaeohyphomycosis in a Tertiary Care Cancer Center. Clin Infect Dis 48(8): 1033-1041.
- Jayawickrama N, Gamage H, Perera P (2012) Conidiobolus Coronatus infection of the paranasal sinuses masquerading as a sino-nasal tumor. Ceylon Med J 57(2): 87.
- Jeragh A, Ahmad S, Khan Z, Tarazi RY, Ajmi S, et al. (2019) Subcutaneous phaeohyphomycosis caused by Amesia atrobrunnea in Kuwait. Journal de Mycologie Médicale 29(2): 193-197.





























