The Incidence of Vasovagal Attack after Septoplasty Surgery
Abdulwahid Alqhtani1*, Waleed Alghamdi2, Mohammad Aqeel2, Khalid Alqhtani3 and Ahmad Etwadi3
1 Department of ORL-HNS, AFHSR, Southern of Saudi Arabia, Saudi Arabia
2 Department of ORL-HNS, Aseer Central Hospital Kingdom of Saudia Arabia, Saudi Arabia
3 Department of ORL-HNS, Khamis General Hospital, Southern of Saudi Arabia, Saudi Arabia
Submission:June 22, 2020; Published:July 08, 2020
*Corresponding author:Abdulwaheed Alqhtani, Department of ORL-HNS AFHSR, Southern of Saudi Arabia, Saudi Arabia
How to cite this article: Abdulwahid A, Waleed A, Mohammad A, Khalid A, Ahmed E. The Incidence of Vasovagal Attack after Septoplasty Surgery. Glob J Oto, 2020; 22(5): 556098. DOI: 10.19080/GJO.2020.22.556098
Abstract
Background: vasovagal syncope is referred to as neurocardiogenic syncope which is subtypes of neutrally mediated (reflex) syncope. VVS characterized by a transient loss of consciousness due to a neurologically induced drop in blood pressure. The vasovagal response (VVR) is a possible complication that may occur during rhinologic manipulation.
Aims/Objectives: To detect the incidence and correlates of vasovagal attack after septoplasty among patients in Khamis general hospital, Southern of Saudi Arabia.
Methodology: A retrospective record-based study was conducted including all patients with clinically diagnosed DNS and undergone surgical intervention at Khamis Mushayet General Hospital. Data extracted included patient’s demographic data, clinical signs and symptoms, history of post-operative vasovagal attacks.
Results:The study included a total sample of 94 patients, 46 (48.4%) patients had traumatic nasal deviation and 48 (51.6%) had no history of trauma. Sixty-seven (71.3%) of the patients aged less than 30 years and 56 (59.6%) were males. Nasal obstruction was the most recorded clinical complaint among the patients in total (96.8%) followed by snoring (65.6%). Vasovagal attacks were not commonly recorded among the included cases.
Conclusions & recommendations: In conclusion, the study revealed that vasovagal attack was not common among patients who undergone septoplasty. Also, experiencing post-surgical vasovagal attacks was nearly the same for all patients regardless their ages and gender
Keywords:Septoplasty; Complications; Vasovagal attack; Syncope; Determinants
Background
Vasovagal syncope (VVS) is commonly recorded postoperative attacks due to vagus nerve stimulation causing bradycardia [1,2]. Vasovagal syncope is referred to as neurocardiogenic syncope [3-5], which is subtypes of neurally mediated (reflex) syncope [6]. VVS characterized by a transient loss of consciousness due to a neurologically induced drop in blood pressure [7]. Sweating may precede the attack immediately with blurred vision or ringing in the ears [8]. Occasionally the person may twitch when unconscious. Person with VVS may be injured from a fall.
Recently, otolaryngology instruments and surgical procedures have significantly improved, with a shift toward more minimally invasive procedures [9,10]. The vasovagal response (VVR) is a possible complication that may occur during rhinologic manipulation. A treatment algorithm for this phenomenon has not been previously established in rhinology. Most types of septoplasty techniques include the use of nasal packing [12]. First experiences with this packs show some postoperative adhesions and crusting [13]. Complications related to pack insertion include pain, vasovagal attack, cardiovascular collapse, hypovolemic shock, vasovagal reflex and trauma to columella, nasal mucosa, and soft palate [14]. The current study aimed to assess the incidence of vasovagal attacks post septoplasty and its relationship with patients’ characteristics.
Methodology
A retrospective record-based approach was used targeting all patients with clinically diagnosed DNS and undergone surgical intervention at Khamis Mushayet General Hospital during the period from January 2017 to end of May 2019. All medical files were reviewed, and clinical data were extracted using prestructured data extraction sheet to minimize data extraction error. Files with incomplete data were excluded if personal contact with the patient failed. Data extracted included patient’s demographic data, trauma related data, clinical signs and symptoms, besides post-operative recorded complications, and occurrence of vasovagal attacks.
Data Analysis
After data were collected it was revised, coded, and fed to statistical software IBM SPSS version 22. The given graphs were constructed using Microsoft excel software. All statistical analysis was done using two tailed tests and alpha error of 0.05. P value less than or equal to 0.05 was statistically significant. Frequency and percent were used to describe the frequency distribution of the different collected variables including signs and symptoms and post-operative complications and history of vasovagal attacks. Cross tabulation was used to show the post-operative vasovagal attack in relation to patient’s personal characteristics using chisquare test.
Results
The study included a total sample of 94 patients, 46 (48.4%) patients had traumatic nasal deviation and 48 (51.6%) had no history of trauma. Sixty-seven (71.3%) of the patients aged less than 30 years and 56 (59.6%) were males (Table 1). Nasal obstruction was the most recorded clinical complaint among the patients in total (96.8%) followed by snoring (65.6%), frontal headache (51.6%), and nasal discharge (46.2%) while epistaxis was recorded among 23.7% of the cases. As for post-operative complications, Figure 1 demonstrates that 32% of the cases had nasal obstruction followed by external nasal deformity (17%), smell disturbance (11%), dental anaesthesia (10%), infection (10%), septal perforation (6%), and nasal bleeding (5%) (Table 2).
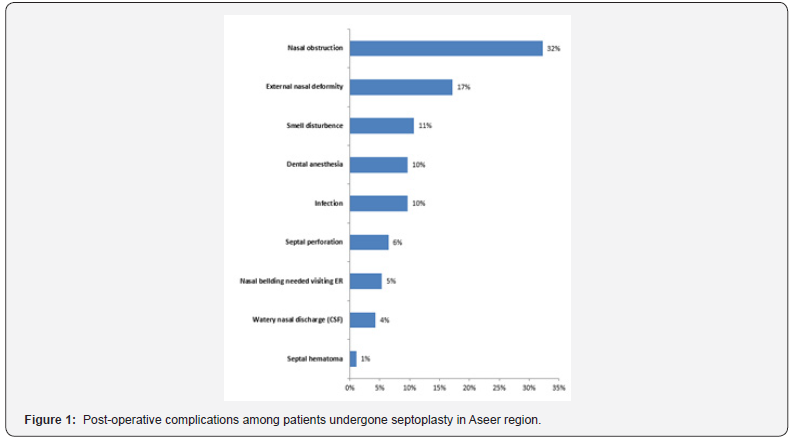
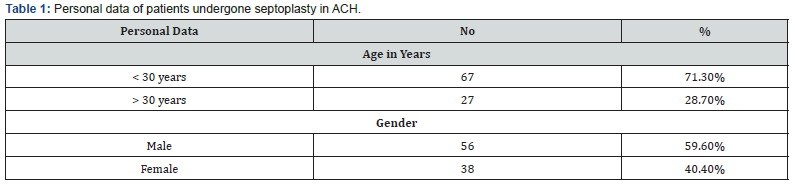
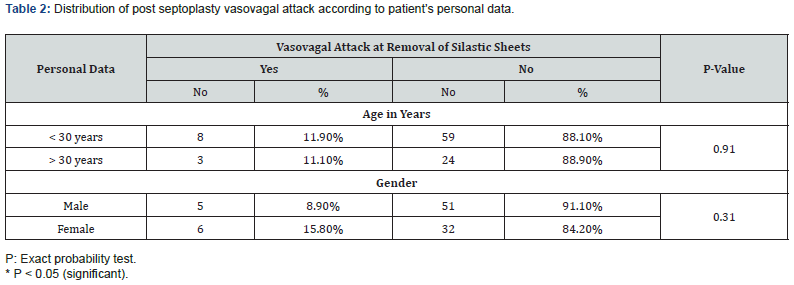
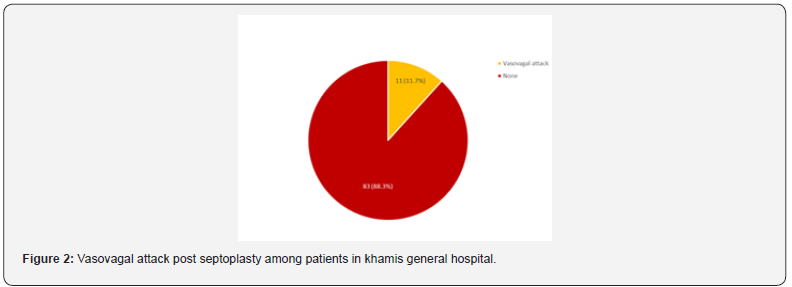
Figure 2 illustrates the incidence of post septoplasty vasovagal attack. It was diagnosed among 11 patients (11.7%). Vasovagal attack was insignificantly higher among patients aged above 30 years than those who were below the age of 30 (88.9% vs. 88.1%, respectively; P=.910). Also, it was insignificantly more diagnosed among male patients (91.1%) than female patients (84.2%) (P=.310).
Discussion
Vasovagal syncope (VVS) is an alarming but benign condition that may recorded postoperatively for the first time in even healthy patients [15]. Although VVS is associated with nasal manipulation, no data have been found to quantify this incidence with otolaryngology surgeries. In the current study researchers aimed to find out the incidence and correlates of vasovagal attack after septoplasty surgery. The study revealed that nasal obstruction was the most recorded complain before surgery and still post-surgery main complications. Vasovagal attack was recorded among nearly 1 out of each 10 patients. Age and gender were insignificantly associated with the higher incidence of experiencing post-surgical vasovagal syncopal attacks.
Glossopharyngeal neuralgia was first recorded in 1910 which described by recurrent pain related to the visceral region of Cranial Nerves IX and XII [16]. The association of hypotensive syncope was not reported until 1927 [17], and then again in 1942 [18]. Syncope has been featured as an even less frequent among patients with these cranial nerve neuralgias [19]. The term “vagoglosso pharyngeal neuralgia” was initiated to describe an associated vagus nerve reflex as a possible etiology in “painless cranial nerve neuralgias” with syncope [20].
Conclusion
In conclusion, the study revealed that vasovagal attack was not common among patients who undergone septoplasty. Also, experiencing post-surgical vasovagal attacks was nearly the same for all patients regardless their ages and gender. A larger scale study including more cases with more clinical assessment is advised to be conducted to have more knowledge and explanations for the findings.
References
- Fenton AM, Hammill SC, Rea RF, Low PA, Shen WK (2000) Vasovagal syncope. Ann Intern Med 133(9): 714-725.
- Amundson J, Hamdan MH (2016) Increased syncopal episodes post-surgery· Dx? J Fam Pract 65(5): 333-335.
- Arakeri G, Arali V (2010) A new hypothesis of cause of syncope: trigeminocardiac reflex during extraction of teeth. Med Hypotheses 74: 248-251.
- Kinsella SM, Tuckey JP (2001) Perioperative bradycardia and asystole: relationship to vasovagal syncope and the Bezold-Jarisch reflex. Br J Anaesth 86: 859-868.
- Chen Scarabelli C, Scarabelli TM (2004) Neurocardiogenic syncope. BMJ 329(7461): 336-341.
- Brignole M, Alboni P, Benditt D, L Bergfeldt, J J Blanc, et al. (2001) Task Force on Syncope, European Society of Cardiology. Task force on syncope, European Society of Cardiology. Part 1. The initial evaluation of patients withsyncope. Europace 3: 253-260.
- Adkisson WO, Benditt DG (2017) Pathophysiology of reflex syncope: A review. J Cardiovasc Electrophysiol 28(9): 1088-1097.
- Alboni P, Alboni M (2017) Typical vasovagal syncope as a “defense mechanism” for the heart by contrasting sympathetic overactivity. Clin Auton Research 27(4): 253-261.
- Albritton FDt, Casiano RR, Sillers MJ (2012) Feasibility of in office endoscopic sinus surgery with balloon sinus dilation. Am J Rhinol Allergy 26: 243-248.
- Prickett KK, Wise SK, DelGaudio JM (2012) Cost analysis of office-based and operating room procedures in rhinology. Int Forum Allergy Rhinol 2: 207-211.
- Lee JG, Leung JW, Cotton PB (1995) Acute cardiovascular complications of endoscopy: prevalence and clinical characteristics. Dig Dis 13: 130-135.
- Shafi M (2016) Complications of post septoplasty nasal packing and trans-septal suturing. Journal of Surgery Pakistan (International) 21: 3.
- Shah G (2018) Comparison of septoplasty with and without nasal packing: its association with post-operative nasal adhesion formation. JIMDC 7(3): 169-173.
- Weber R, Keerl R, Hochapfel F, Draf W, Toffel PH (2001) Packing in endonasal surgery. Am J otolaryngol 22(5): 306-320.
- Moya A, Bringnole M, Menozzi C, R Garcia Civera, S Tognarini, et al. (2001) Mechanisms ofsyncope in patients with isolated syncope and in patients with tilt-positive syncope. Circulation 104: 1261-1267.
- Weisenberg TH (1910) Cerebellopontine tumor diagnosed for six years as ticdouloureux: the symptoms of irritation of the 9th and 12th cranial nerves. JAMA 54: 1600-1604.
- Harris W (1921) Persistent pain in lesions of the peripheral and centralnervous system. Br Med J 2(3178): 896-900.
- Rushton JG, Stevens JC, Miller RH (1981) Glossopharyngeal (vagoglosso-pharyngeal) neuralgia: a study of 217 cases. Arch Neurol 38: 201-205.
- Riley HA, German WJ, Wortis H (1942) Glossopharyngeal neuralgiainitiating or associated with cardiac arrest. Trans Am Neurol Assoc 68: 28-29.
- White JC, Sweet WH (1969) Pain and the neurosurgeon: a 40-yearexperience. Springfield (IL): Charles C. Thomas, Publisher, pp. 265-280.





























