Retrospective Analysis of Phonatory Outcomes after CO2 Laser Thyroarytenoid Myoneurectomy in Patients with Adductor Spasmodic Dysphonia
Rohan Bidaye1*, Sachin Gandhi2*, Aishwarya M3 and Vrushali Desai4
1Senior Clinical Fellow in Laryngology, Deenanath Mangeshkar Hospital, India
2Head of Department of ENT, Deenanath Mangeshkar Hospital, India
3 Fellow in Laryngology, Deenanath Mangeshkar Hospital, India
4Chief Consultant, Speech Language Pathologist, Deenanath Mangeshkar Hospital, India
Submission:May 16, 2020; Published: June 08, 2020
*Corresponding author:Rohan Bidaye, Senior Clinical Fellow in Laryngology, Deenanath Mangeshkar Hospital, India Sachin Gandhi, Head of Department of ENT, Deenanath Mangeshkar Hospital, Pune, India
How to cite this article: Rohan B, Sachin G, Aishwarya M, Vrushali D. Retrospective Analysis of Phonatory Outcomes after CO2 Laser Thyroarytenoid Myoneurectomy in Patients with Adductor Spasmodic Dysphonia. Glob J Oto, 2020; 22(4): 556091.DOI: 10.19080/GJO.2020.22.556091
Abstract
Introduction: Adductor spasmodic dysphonia (ADSD) is a focal laryngeal dystonia characterized by spasms of laryngeal muscles during speech. Botulinum toxin injection in the Thyroarytenoid muscle remains the gold-standard treatment for ADSD. However, as Botulinum toxin injections need to be repeated periodically, the voice quality fluctuates over a longer period. A Microlaryngoscopic Transoral approach to CO2 laser Thyroarytenoid myoneurectomy (TAM) has been reported as an effective technique for treatment of ADSD. It provides sustained improvement in the voice over a longer duration.
Methods: Trans oral Microlaryngoscopic CO2 laser TAM was performed in 14 patients (5 females and 9 males), aged between 19 and 64 years who were diagnosed with ADSD. Data was collected from over 3 years starting from Jan 2014 – Dec 2016. GRBAS scale along with Multi-dimensional voice programme (MDVP) analysis of the voice and Video laryngo-stroboscopic (VLS) samples at the end of 3 and 12 months of surgery would be compared with the pre-operative readings.
Results: A total of 9 (64.2%) patients showed an improvement in grade after 3 months as well as 12 months after the surgery. While 12 (85.7%) patients showed an improvement in strain after 12 months of surgery. The spasms on VLS showed an improvement in 9 (64.3%) out of 14 cases after 3 months of surgery which was proven to be statistically significant.
Conclusion: This innovative surgical technique is a good alternative treatment for ADSD patients who seek a definite improvement of their condition.
Keywords: Laser; Spasmodic dysphonia; Surgery; Myoneurectomy
Abbreviations: ADSD: Adductor Spasmodic Dysphonia; TAM: Thyroarytenoid Myoneurectomy; MDVP: Multi-Dimensional Voice Programme; VLS: Video Laryngo-Stroboscopic
Introduction
Spastic Dysphonia (SD) is a rare but disabling voice disorder caused by involuntary movements or spasms of one or more muscles of larynx during speech [1]. The aetiology is believed to be multifactorial and is still not completely understood [2]. However, it is suspected to be neurological in origin and is likely due to a sensory disorder with the muscle spindle playing a central role [3,4]. SD is classified as a ‘rare disease’ by the National Institute of Health, USA. With a prevalence rate of 14 per 100,000 it predominantly affects women in the ratio of 2.5:1, with the peak of onset being between 30-50 years. It is classified mainly into Adductor Spastic Dysphonia (ADSD), Abductor Spastic Dysphonia and the mixed variant [5]. ADSD is characterized by involuntary spasms of laryngeal muscles during adduction, producing tense vocal cords and a strained voice. Abductor SD has uncontrolled spasms in abductor muscle resulting in breathy bursts when attempting to initiate phonation.
Mixed SD has the characteristics of both [6]. 80% of the cases of SD are of the adductor type [7]. Chemo denervation with Botulinum toxin has been the treatment of choice since the 1980’s. However, it takes about two weeks for the full therapeutic efficacy of this treatment to be evident. In addition to that, the therapeutic benefits of this treatment are temporary and usually wear off within a few weeks to a few months depending on the dose used. As such, repeated injections are required to sustain the desired effect [8-10]. The centres for botulinum toxin therapy are also rather limited, especially in India. These abovementioned limitations of Botulinum toxin injections have paved the need for different surgical approaches to treat this condition. The surgical options published are Thyroarytenoid myectomy/ myoneurectomy, Thyroplasty type II and type III and Selective laryngeal adductor denervation-reinnervation, Laryngeal nerve crush and recurrent laryngeal nerve resection [8,11-14]. A transoral approach to laser Thyroarytenoid myoneurectomy (TAM) to treat ADSD was reported by Domingoes et al. and Su et al. more than a decade ago [15,16]. This surgery has shown favourable results in terms of phonatory outcomes [17,18]. The aim of the present study is to report the subjective and objective voice outcome after Transoral CO2 laser TAM in patients with ADSD.
Materials and Methods
This retrospective study approved by the institution’s ethical committee was conducted by the Department of Laryngology. A total of 14 patients with the diagnosis of ADSD who satisfied the criteria and were enrolled into the study. The data was collected from our previous records from Jan 2014-Dec 2015 over a 3-year period. The inclusion criteria were patients diagnosed with ADSD and had consented for the surgery. Patients with previous Botox injections were included in the study. A gap of 6 months was maintained for the Botox to completely wear off before the surgery. Patients with any accompanying neuromuscular disorder or structural changes in the larynx were excluded. Data was collected from files of the patients who underwent TAM for ADSD. GRBAS scale along with MDVP (Multi-dimensional voice programme) analysis of the voice and Video Laryngo-Stroboscopic (VLS) evaluation was performed with a flexible laryngoscope.
The sample of voice was recorded in a soundproof room with a Neutrik microphone at the first visit and at every follow up. The recorded samples were used to calculate the GRBAS scale and underwent MDVP analysis. The recordings before the surgery were compared with the post-surgery 3 and 12-month follow up. Both subjective and objective parameters were used. GRBAS is a scale for perceptual analysis of voice where G (Grade), R (Roughness), B (Breathiness), A (Asthenicity) and S (Strain) is graded as 0 = normal, 1 = mild, 2 = moderate and 3 = severe on the scale. The CSL 4500B (Kay Pentax) connected to a PC was used for the acoustic analysis. The parameters evaluated included the fundamental Frequency (F0), Noise to Harmonic Ratio (NHR), Jitter and Shimmer in the pre- and the post-operative voice. The VLS recordings were assessed for glottal closure, supraglottal closure and the presence of spasms. Each parameter was rated on a 4-point scale as three – increased, 2-normal, 1-reduced and 0- Absent.
The Surgical Technique for TAM
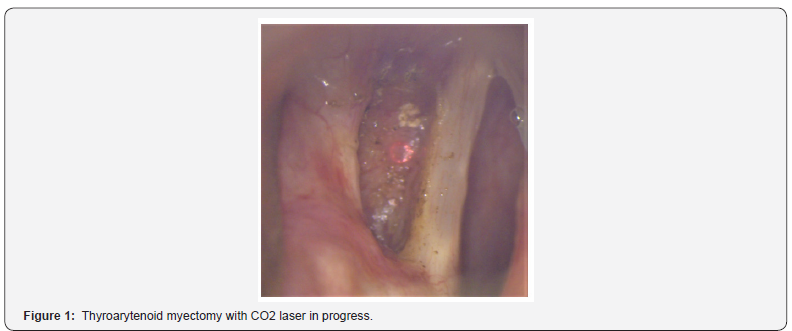
Sub glottis Jet ventilation technique was used with a Hunsaker catheter. Direct laryngoscope was introduced achieving proper visualisation with a microscope. We used the Lumenis ultra pulse CO2 laser with the Acublade coupled to a Leica microscope. Bilateral ventricular folds were excised with CO2 laser in Pulse mode at a power setting of 4W. This allows better exposure of the vocal folds from the free edge medially to the thyroid cartilage laterally. This also ensures management of secondary hypertrophy of the ventricular folds. Partial myectomy of thyroarytenoid muscle was performed with a CO2 laser in the scanner mode with a diameter of 1-1.5 mm and intensity adjusted at 6W (Figure 1). Care was taken with the medial limit of vaporization being 1 mm lateral to the vocal ligament and the lateral limit was 1 mm medial to the inner perichondrium of the thyroid cartilage.
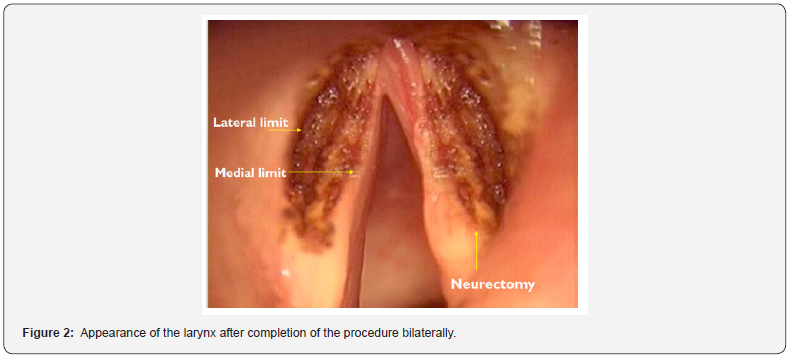
Anteriorly, the extent was the junction of the anterior and the middle 1/3rd of the vocal cord and the posterior limit was the vocal process. The depth of dissection was gauged with a probe and was around 3-4 mm into the vocalis muscle. The terminal nerve fibres of the thyroarytenoid branch of the inferior laryngeal nerve are commonly located just anterior and lateral to the vocal process. Neurectomy was performed by diffuse cauterisation of the area with the help of a suction cautery (Figure 2). All patients were given intraoperative intravenous steroids to reduce development of laryngeal oedema. Oral Antibiotics and Anti-inflammatory medications were continued for 5 days post-surgery. Statistical analysis was done with the help of SPSS 20. Frequencies were calculated and Wilcoxon signed ranks test was used to compare the mean scores. A p-value of 0.05 was defined as statistically significant.
Results
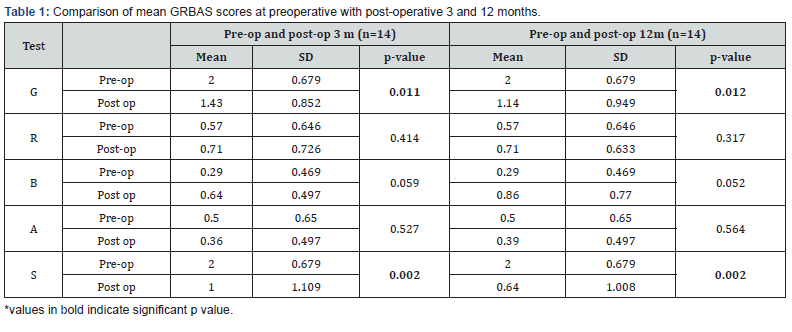
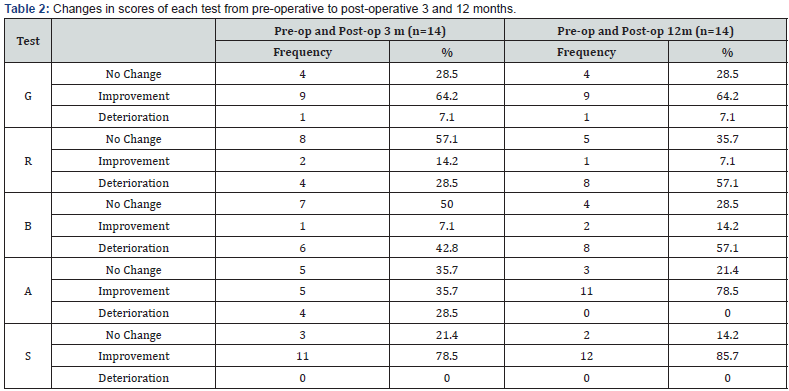
Our study sample had 14 patients out of which 5 were females and 9 were males. Their ages ranged from 19 and 64 years of age. There was a statistically significant improvement in both the Grade and Strain values in the pre and post-operative 3-month and 12-month groups (Table 1). A total of 9 patients (64.2%) showed an improvement in grade after 3 months as well as 12 months after the surgery. While 11 (78.5%) patients showed an improvement in strain post 3 months. 12 (85.7%) patients showed an improvement in strain post 12 months after surgery. Breathiness showed deterioration in 8 patients (57.1%) at the end of 12 months, however this was not statistically significant (Table 2).
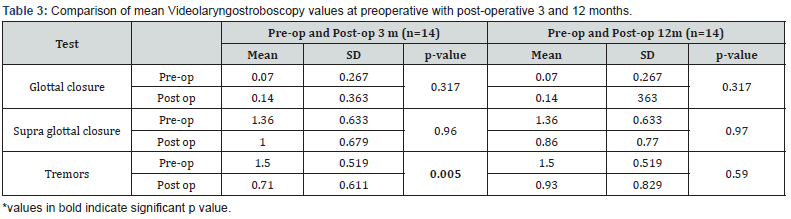
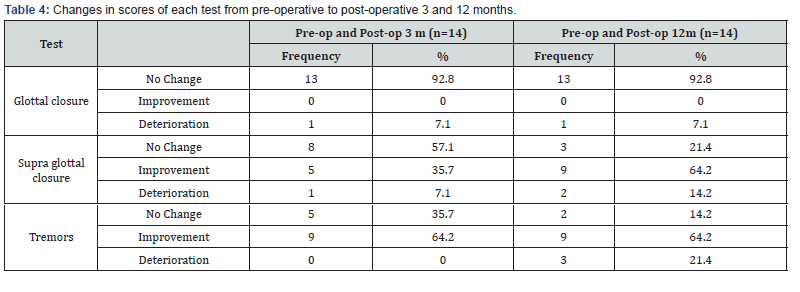
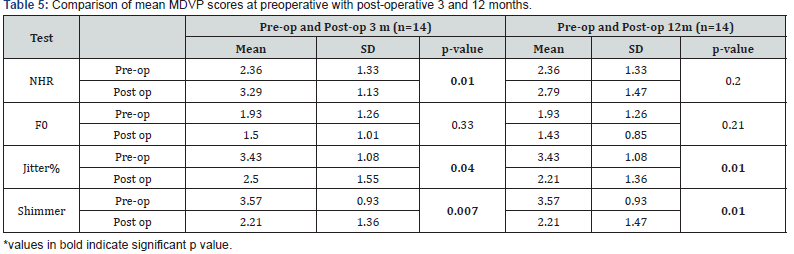
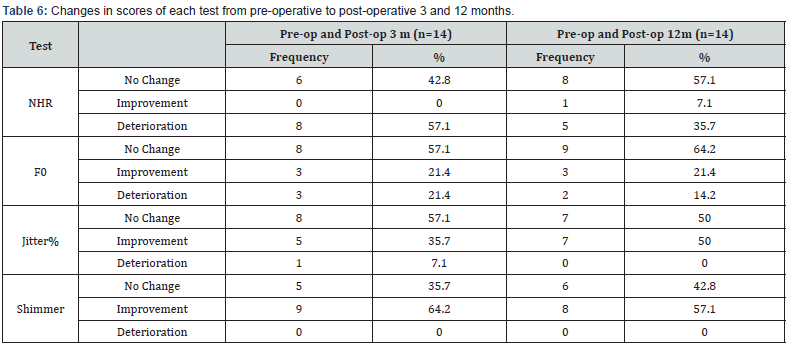
The tremors on VLS showed an improvement in 9 out of 14 cases (64.3%) after 3 months of surgery, which was proven to be statistically significant too. There was no deterioration of tremors seen in any of the patients 3 months after surgery. Glottal closure was complete in 13 out of the 14 patients (92.8%) at the end of 12 months. Supra glottal closure showed improvement in 9 out 14 patients at the end of 12 months (Table 3 & 4). MDVP values of F0, NHR, Jitter and Shimmer were expressed as standard deviations for the ease of analysis. Mean MDVP scores showed a statistically significant improvement in Jitter and shimmer both at post-operative 3-month and 12-month interval. Jitter improved in 7(50%) out of the 14 patients while shimmer improved in 8 (57.1%) at the end of 12 months. NHR deteriorated in 8 patients at 3 months follow up, however that figure reduced to 5 at the end of 12 months (Table 5 & 6).
Discussion
Peek Woo et al. [19] in 1990 described the new thyroplasty approach to laser assisted thryoarytenoid myectomy. Kaufmann et al. [20] described the procedure of Thyroarytenoid and Lateral Cricoarytenoid myectomy using an external approach, which showed encouraging preliminary results. Domingoe’s et al in 2006 first reported Endoscopic laser TAM in patients with ADSD [7]. He performed the surgery using a CO2 laser for the partial myectomy followed by an electrocutery knife for the Neurectomy of the thyroarytenoid branch of the inferior laryngeal nerve. Voice improvement was reported in the 6 patients. The follow up of the cases was done for 23 months and the criteria of success for the surgery was based on the VHI scale. Hussaina in 2010 reported a case series of 4 patients with a 2 and a half year follow up which reported improvement in the voice quality, fluency and elimination of voice breaks [21]. Chih Ying Su et al. with 52 patients is the largest reported series of TAM in patients with ADSD. In his prospective study subjective and objective voice assessment with acoustic (MDVP) and aerodynamic measurements were performed and analysed. The 12 months follow up showed marked improvement in voice in more than 90% of his patients [17].
Our results were like the above-mentioned studies. Our series has shown a well lasting improvement in GRBAS suggesting a good subjective improvement in voice. MDVP as an objective analysis also showed a significant improvement in the quality of voice. VLS, which was used to visualise the reduction in the spasms, was evidence of the surgery being very effective. In our series of 14 patients comparing the GRBAS shows an improving trend up to 12 months post operatively. Strain is the component of GRBAS most commonly affected in patients with ADSD. Strain showed the most significant difference with improvement in 12 out of the 14 patients. The Strain component was primarily responsible for the poor grade of voice preoperatively. The Grade of voice showed significant improvement at the end of 3 months, which was sustained over the entire 12 months of follow up. It is commonly observed that strain and breathiness are inversely related and so has been our finding during the study. Breathiness in the voice was expected and found to have increased in a few patients. However, the results were not statistically significant.
VLS examination of the larynx pre and post operatively was performed by Su et al. [17]. Their study showed promising improvement and so we decided to incorporate VLS examination in our protocol. Preoperatively, the most frequent abnormal finding on VLS was the presence of Spasms along with supra glottal compression. This correlates with the Strain in voice on GRBAS. Spasms showed a statistically significant improvement in 9 out of 14 patients at the end of 3 months. However, there was reappearance of spasms in the post op 12-month group, suggestive of regeneration of the nerve endings. This reappearance was not seen symptomatically as the subjective and objective voice quality remained consistent over the 12 months follow up. Thyroarytenoid myectomy without neurectomy showed signs of relapse after a few months [22]. Also, laryngeal nerve transections showed similar results which was proposed to be cause of regeneration of the nerve or reinnervation of the muscle [23-26]. Combining neurectomy with myectomy reduced the chances of relapse by impairing the process of re-innervation of the remnant muscle [15]. The glottal closure remained complete in all except one. The supra glottal compression was noted to improve over the course of 1 year and this was in accordance with the reduced Strain on GRBAS scale.
MDVP is the most widely used research computerised voice analysis system and is reliable in the measurement of fundamental frequency; jitter and shimmer [27]. Jitter and shimmer are the most important parameters to judge an improvement in the voice after surgery for ADSD. A reduction in the values suggest an improvement in the voice quality. The MDVP readings showed an improvement in jitter and shimmer which was sustained over the entire 12-month period after the surgery. Fundamental frequency remained unaffected. NHR is the measure for glottal closure with incomplete closures corresponding to higher NHR values. NHR worsened initially but recovered by the end of 12 months. This could be because of the transient glottal gap arising post-surgery. However, none of the values were proven to be statistically significant.
Various studies have proven the efficacy of Botulinum toxin type an injections in the Thyroarytenoid muscle with improvement in symptoms [28]. This proves that Thyroarytenoid is the major muscle responsible for the disease symptoms. Lateral Cricoarytenoid is the primary adductor of the glottis and damage to it can lead to significant glottal incompetence. Therefore, the vaporization was strictly limited to the Thyroarytenoid and the ventricular folds avoiding damage to the adjacent muscles in the larynx [17]. Laser excision of the Thyroarytenoid fibres results in its replacement with fibrotic tissue. Because of which the motor end plates significantly reduce in number [16]. The maximum number of motor end plates are found in the middle 1/3rd (74%) of the Thyroarytenoid muscle followed by the posterior 1/3rd (19%) [29]. The least number of end plates are found in the anterior 1/3rd (7%). Rossi et al noted similar findings with maximum end plates in the middle 1/3rd [30].
Therefore, the excision of the Thyroarytenoid was limited to the posterior 2/3rd of the muscle and the anterior 1/3rd was spared as it offers no further surgical benefit and carries risk of glottal incompetence after the surgery. ADSD patients often show the presence of ventricular fold hyper function/hyper adduction. Rosen et al has reported that the vocalis muscle provides a few muscle fibres extending up to the ipsilateral ventricular fold [16,31]. Also, a significant number of motor end plates have been detected in the ventricular folds. Botox injected into the ventricular folds by Schonweiler et al. showed improvement in the hyper function of the ventricular folds [32]. Hence ventricular fold resection helps not only in the exposure but also with the reduction in the strain in voice because of the supraglottic component. The volume of muscle removed during the surgery was around 70 – 80 %. A 3-4 mm depth of vaporization was considered as an adequate removal. Su et al in his study had noticed post-operative strain in the patients who underwent less than 70% removal of the muscle [17].
These patients had to undergo a revision surgery. With the removal of more than 70% of the Thyroarytenoid muscle, the patient does notice significant breathiness for period of 2-3 months. However as noted in our study the breathiness subsided over a period. Most patients developed hoarse voice in the immediate post-operative period, which gradually improved during follow up. The immediate hoarse voice was because of Edema of the larynx and transient neurological dysfunction. We did not notice any aspiration amongst the 14 patients in the postsurgical period. There were no complications reported in our series. Same was the case with Su et al. [17]. However out of the 52 patients of Su et al. [17] patients required a revision surgery. The case series consolidates the results from previous studies proving the efficacy of the surgery. It also objectively demonstrates an improvement in the voice and a reduction in spasms on VLS.
Conclusion
Trans oral CO2 laser TAM shows a significant long-term improvement in voice quality. This surgery provides a good alternative line of management in patients with ADSD.
References
- Blitzer A, Lovelace RE, Brin MF, Fahn S, Fink ME (1985) Electromyographic findings in focal laryngeal dystonia (spastic dysphonia). Ann Otol Rhinol Laryngol 94: 591-594.
- Murry T (2014) Spasmodic dysphonia: let’s look at that again. J Voice 28: 694-699.
- Schweinfurth JM, Billante M, Courey M S (2002) Risk Factors and Demographics in Patients with Spasmodic Dysphonia. The Laryngoscope 112: 220-223.
- Walter U, Blitzer A, Benecke R, Grossmann A, Dressler D (2014) Sonographic detection of basal ganglia abnormalities in spasmodic dysphonia. Eur J Neurol 21(2): 349-352.
- Whurr R, Lorch M (2016) Review of differential diagnosis and management of spasmodic dysphonia. Curr Opin Otolaryngol Head Neck Surg 24(3): 203-207.
- Blitzer A, Brin MF, Stewart CF (1998) Botulinum toxin management of spasmodic dysphonia (laryngeal dystonia): A 12-year experience in more than 900 patients. The Laryngoscope 108: 1435-1441.
- Rubin AD, Wodchis WP, Spak C, Kileny PR, Hogikyan ND (2004) Longitudinal Effects of Botox Injections on Voice-Related Quality of Life (V-RQOL) for Patients with Adductor Spasmodic Dysphonia Part II. Arch Otolaryngol Head Neck Surg 130(4): 415-420.
- Mendelsohn AH, Berke GS (2012) Surgery or Botulinum toxin for Adductor spasmodic dysphonia: A comparative study. Ann Otol Rhinol Laryngol 121: 231-238.
- Elmiyeh B, Prasad VMN, Upile T (2010) A single centre retrospective review of unilateral and bilateral Dysport injections in adductor spasmodic dysphonia. Logoped Phoniatr Vocol 35: 39-44.
- Esposito M, Dubbioso R, Apisa P, Allocca R, Santoro L, et el. (2015) Spasmodic dysphonia follow up with Videolaryngoscopy and voice spectography during treatment with Botulinum toxin. Neurol Sci 36: 1679-1682.
- Chan S W, Baxter M, Oates J, Yorston A (2004) Long-Term Results of Type II Thyroplasty for Adductor Spasmodic Dysphonia. The Laryngoscope 114: 1604-1608.
- Biller HF, Som ML, Lawson W (1983) Laryngeal nerve crush for spastic dysphonia. Ann Otol Rhinol Laryngol 92: 469.
- Aronson AE (1983) Adductor spastic dysphonia: 3 years after recurrent laryngeal nerve resection. Laryngoscope 8: 1-8.
- Sanuki T, Yumoto E, Kodama N et al. (2014) Long-term voice handicap index after type II thyroplasty using titanium bridges for adductor spasmodic dysphonia. Auris Nasus Larynx 41: 285-289.
- Domingos HT, Fernanada SC, Rui I, Luiz US, Adriana H (2006) Impact in vocal quality in partial myectomy and neurectomy endoscopic of thyroarytenoid muscles in patients with adductor spasmodic dysphonia. Ev Bras Otorhinolaryngol 72: 261-266.
- Su CY, Chuang HC, Tsai SS, Chiu JF (2007) Transoral approach to laser thyroarytenoid myoneurectomy for treatment of adductor spasmodic dysphonia: short-term results. Ann Otol Rhinol Laryngol 116: 11-18.
- Su CY, Lai CC, Wu PY, Huang HH (2010) Tran’s oral laser ventricular fold resection and thyroarytenoid myoneurectomy for adductor spasmodic dysphonia: Long-term outcome. Laryngoscope 120(2): 313-318.
- Gandhi S, Remacle M, Mishra P (2014) Vocal outcome after endoscopic thyroarytenoid myoneurectomy in patients with adductor spasmodic dysphonia. Eur Arch Otorhinolaryngol 271: 3249-3254.
- Woo P (1990) Carbon dioxide laser assisted thyroarytenoid myomectomy. Lasers Surg Med 10: 438-443.
- Koufmann JA, Rees CJ (2006) Treatment of adductor type spasmodic dysphonia by surgical myectomy: A preliminary report. Ann Otol Rhinol Laryngol 115: 97-102.
- Hussaina A, Shakeela M (2010) Selective lateral laser thyroarytenoid myotomy for adductor spasmodic dysphonia. J laryngol Otol 124: 886-891.
- Tsuji DH, Takahashi MT, Imamura R, Hachiya A, Sennes LU (2012) Endoscopic laser thyroarytenoid myoneurectomy in patients with adductor spasmodic dysphonia: a pilot study on long-term outcome on voice quality. J Voice 26(5): 666.e7-12.
- Netterville JL, Stone RE, Rainey C, Zealear DL, Ossoff RH (1991) Recurrent laryngeal nerve avulsion for treatment of spastic dysphonia. Ann of otol rhinol Laryngol 100: 10-14.
- Aronso AE, Desanto LW (1983) Adductor spastic dysphonia. 3 year after recurrent laryngeal nerve resection. Laryngoscope 93: 1-8.
- Dedo HH, Izdebski K (1983) Problems with surgical (RLN section) treatment of spastic dysphonia. Laryngoscope 93: 268-271.
- Schiratzki H, Fritzell B (1988) Treatment of spasmodic dysphonia by means of resection of the recurrent laryngeal nerve. Acta Otolaryngol 449: 115-117.
- Mat Baki M, Wood G, Alston M, Ratcliffe P, Sandhu G, et al. (2015) Reliability of Opera VOX against multidimensional voice program (MDVP) Clin Otolaryngol 40(1): 22-28.
- Blitzer A (2010) Spasmodic dysphonia and botulinum toxin: Experience from the largest treatment series. Eur J Neurol 17: 28-30.
- Sheppert AD, Spirou GA, Berrebi AS, Garnett DJ (2003) Three-dimensional reconstruction of immune labelled neuro muscular junctions in the human thyroarytenoid muscle. Laryngoscope 113(11): 1973-1976.
- Rossi G, Cortesina G (1965) Morphological study of the laryngeal muscle in man; Insertion and courses of the muscle fibres, motor end plate and proprioceptors. Acta otolaryngol 59: 575-592.
- Rosen M, Malmgren LT, Gacek RR (1983) Three-dimensional computer reconstruction of the distribution of the neuromusclular junctions in the thyroarytenoid muscle. Ann. Otol Rhinol Laryngol 92: 424-429.
- Schonweiler R, Wohlfarth K, Dengler R, Ptok M (1998) Supraglottal injection of botulinum toxin Type-A in Adductor type spasmodic dysphonia with both intrinsic and extrinsic hyperfunction. Laryngoscope 108: 55-63.





























