Allergic Fungal Rhinosinusitis in Children: Short Communication
Luis Seguias*
1Pediatric Coordination of Care Program Director, University of Florida, USA
2Audiology and Speech Pathology Programme, School of Health Sciences, University Sains Malaysia, 16150 Kubang Kerian, Kelantan, Malaysia
Submission: July 04, 2019; Published: July 16, 2019
*Corresponding author:Luis Seguias, Pediatric Coordination of Care Program Director, University of Florida, Gainesville, Florida, USA
How to cite this article: Luis Seguias. Allergic Fungal Rhinosinusitis in Children: Short Communication. Glob J Oto, 2019; 20(3): 556040. DOI: 10.19080/GJO.2019.20.556040
Introduction
Allergic rhinitis (AR) and its co morbidities like asthma, sinusitis, and otitis media with effusion have a profound impact on the daily lives of children. Many of the problems go completely unnoticed as children often fail to share them at home or at school. It may result in day – time fatigue, as well as sleeplessness and impairment of cognition and memory. This may significantly affect the learning process and thus impacts on school performance and all these aspects upset the family [1]. Children with AR are often embarrassed in school and have decreased social interaction that significantly hampers the process of learning and school performance [2]. The adverse effects of some medications used for treatment often compoundthese problems [3]. The risk factors of allergic rhinitis include the following dust, moulds, weather changes, pollen, pets and exposure to tobacco smoking.
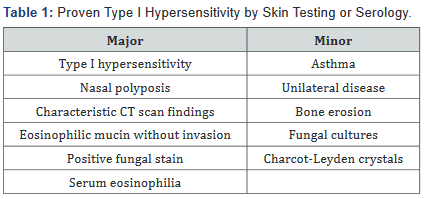
Clinical manifestations can include rhinorrhea, nasal obstruction, headaches, itchy eyes and anosmia. Nasal polyposis is a very common finding ~ 90% cases [6]. In approximately 50% of children with AFRS accumulation of mucin can experience sinus expansion resulting on facial dysmorphia and proptosis [7]. It is not rare to have radiological evidence of orbital erosion in severe cases [8]. Demographically, boys are more commonly affected than girls and African American children often present earlier and with more severe disease [9]. Patients with it commonly are immunocompetent, and up to 50% of patients have comorbid allergic rhinitis or asthma [4]. Bent and Kuhn Diagnostic Criteria[10] is the most accepted by the experts and include characteristic CT imaging findings, evidence of eosinophilic mucus with positive fungal stain, and proven type I hypersensitivity by skin testing or serology (Table 1). Patients must meet all the major criteria for diagnosis, while the minor criteria serve to support the diagnosis and describe individual patients but are not used to make a diagnosis. The histopathologic findings in AFS are critical to the diagnosis. Most of the surgical specimens demonstrated allergic mucin rich on eosinophils along with thecharacteristic Charcot-Leyden crystals. Fungi can be isolated from the mucin but does not invade the nasal and sinusal mucosa. Fungal cultures should be interpreted with caution. AFRS often is associated with dematiaceous fungi, being the most common isolation Aspergillus species [11].
Treatment of AFRS typically includes endoscopic sinus surgery to enlarge the sinus ostia and remove eosinophilic mucin. Saline irrigations are routinely used postoperatively to prevent mucin accumulation. Recent data supports the use of a short course of postoperative oral corticosteroids in the management of postoperative AFRS [12]. Leukotriene modifiers and anti-inflammatory macrolide antibiotics are often employed to try to reduce steroid requirements, but it is unknown if these improve outcomes or reduce the need for revision surgery. A recent meta-analysis reported no statistically significant benefit of systemic or topical antifungal therapy over placebo in the treatment of chronic sinusitis [13]. Complications from allergic fungal sinusitis are exceedingly rare but bacterial superinfection can lead to infectious sinusitis and less commonly to orbital abscess and cavernous sinus thrombosis. In summary, although AFRS is uncommon in the pediatric population a good clinician should be able to distinguish it from bacterial sinusitis, because management of the two differs considerably, and morbidity can be significant if treatment of AFRS is delayed.
References
- Safirstein BH (1976) Allergic Bronchopulmonary Aspergillosis with Obstruction of the Upper Respiratory Tract. Chest Journal 70(6): 789-790
- Schubert MS, Goetz DW (1998) Evaluation and treatment of allergic fungal sinusitis. I. Demographics and diagnosis. J Allergy Clin Immunol 102(3): 387-394.
- Ferguson BJ, Barnes L, Bernstein JM (2000) Geographic variation in allergic fungal rhinosinusitis. Otolaryngol Clin North Am 33(2): 441- 449.
- Manning SC, Holman M (1998) Further evidence for allergic pathophysiology in allergic fungal sinusitis. Laryngoscope 108(10): 1485- 1496
- Tyler, Matthew A. and Luonga Amber U (2018) Current understanding of allergic fungal rhinosinusitis. World J Otorhinolaryngol Head Neck Surg 4(3): 179-185.
- Campbell JM, Graham M, Gray HC, Bower C, Blaiss MS, et al. (2006) Allergic fungal sinusitis in children. Ann Allergy Asthma Immunol 96(2): 286-290.
- McClay JE, Marple B, Kapadia L, Biavati MJ, Nussenbaum B, et al. (2002) Clinical presentation of allergic fungal sinusitis in children. Laryngoscope 112(3): 565-569.
- Bozeman S, Richard de Shazo, Stringer S, Wright L (2011) Complications of allergic fungal sinusitis. Am J Med 124(4): 359-368.
- Wise SK, Venkatraman G, Wise JC, DelGaudio JM (2004) Ethnic and gender differences in bone erosion in allergic fungal sinusitis. Am J Rhinol 18(6): 397-404.
- Glass Daniel , Amedee Ronald G (2011) Allergic Fungal Rhinosinusitis: A Review. Ochsner J 11(3): 271-275
- Katzenstein AL, Sale SR, Greenberger PA (1983) Allergic Aspergillus sinusitis: a newly recognized form of sinusitis. J Allergy Clin Immunol 72(1): 89-93.
- Gan EC, Thamboo A, Rudmik L, Hwang PH, Ferguson BJ, et al. (2014) Medical management of allergic fungal rhinosinusitis following endoscopic sinus surgery: an evidence-based review and recommendations. Int Forum Allergy Rhinol 4(9): 702-715.
- Sacks PL IV, Harvey RJ, Rimmer J, Gallagher RM, Sacks R (2012) Antifungal therapy in the treatment of chronic rhinosinusitis: a meta-analysis. Am J Rhinol Allergy 26(2): 141-147.





























