Predicting and Preventing TEF: Using X-ray Chest and Tracheostomy Tube Cuff Diameter Measurement
Nadeem Malik1, Montasir Junaid2 and Sadaf Qadeer3*
1,2Department of Otolaryngology-head and neck surgery, Armed Forces Hospital Southern Region, Khamis Mushayt, Saudi Arabia
3Department of Otolaryngology-head and neck surgery, Sir Syed College of Medical Sciences for Girls, Karachi, Pakistan
Submission:June 17, 2019;Published:July 02, 2019
*Corresponding author:Sadaf Qadeer, Department of Otolaryngology-head and neck surgery, Sir Syed College of Medical Sciences for Girls, Karachi, Pakistan
How to cite this article:Nadeem M, Montasir J, Sadaf Q. Predicting and Preventing TEF: Using X-ray Chest and Tracheostomy Tube Cuff Diameter Measurement. Glob J Oto, 2019; 20(3): 556038.DOI: 10.19080/GJO.2019.20.556038
Introduction
An abnormal communication between trachea and esophagus (trachea-esophageal fistula: TEF) may occur in critically ill patients who have been intubated for prolonged ventilatory support [1,2]. This particular type of acquired TEF is related to the cuffs of endotracheal and tracheostomy tubes. The first published report of TEF related to prolonged intubation was by d’ Avignon (1956) and Mounier - Kuhn (1958) [3,4]. Andrews and Pearson have reported the incidence of TEF to be 1.9 % in a cohort of 220 mechanically ventilated patients with cuffed tubes [1]. Prolonged intubation (mean 42 days) along with high cuff pressures (25cm H2O ->30 cm H2O) may cause obstruction of capillary perfusion in tracheal epithelium which leads to inflammation, ischemic necrosis, destruction of tracheal and esophageal tissue and eventually resulting in fistula formation [5,6]. In general, the cuff pressure should not exceed more than 20 cm H2O or cuff volume should not exceed 6-8ml [4, 7]. The cuff of tracheostomy tubes (TT) are no exception to this and behave in a similar fashion to the cuff of endotracheal tube (ETT). The site of TEF may differs slightly depending upon the position of the cuff, occurring more cranially in ETT but 1-2 cm caudal to tracheostomy stoma with tracheostomy tubes [8,9]. The diagnosis of tracheoesophageal fistulas may be challenging; a high index of suspicion should be maintained in patients who are on mechanical ventilation and show signs of difficulty in maintaining parameters of ventilator. Evidence of mediastinal or subcutaneous emphysema, abdominal distention, presence of food particles and feed in the tracheobronchial tree, persistent or recurrent pneumonic patches on x-rays are all the signs that should raise concern of physician for TEF [3,10,11]. The incidence of TEF associated with prolonged intubation has reduced (<1%) with the advent of high volume and low pressure endotracheal and tracheostomy tube cuffs [12,13].
The factors associated with the occurrence of tracheoesophageal fistula are the presence of high cuff pressure, high airway pressure, excessive motion of tracheal tube, prolonged duration of intubation, respiratory infections, hypotension, steroids, concomitant nasogastric tube, female gender, advance age and insulin dependent diabetes [5]. Here we will discuss an interesting finding that was noticed in the chest x-rays of a patient who developed a TEF. A progressive increase in tracheal diameter at the site of tracheostomy tube cuff was noted, coinciding with the progressive difficulty in mechanical ventilation and subsequent development of TEF. We consider this progressive increase in the tracheal diameter at the site of tube cuff an important sign, indicating progressive destruction of the tracheal wall and eventually leading to TEF. This may possibly be used to predict and thus prevent the development of TEF in critically ill patients in ICU using serial chest x-rays. Here we report the possible relationship between increasing tube cuff diameter and development of TEF, also using it to predict and prevent the development of TEF; this has not been reported in the literature before.
Case Report
A 68 years old female, resident of Saudi Arabia, was admitted to intensive care unit (ICU)via emergency room in an unconscious state. She was diagnosed of septic shock secondary to aspiration pneumonia. Her Glasgow Coma Scale was 4/15, endotracheal intubation was performed, mechanical ventilation (SIMV Mode) was initiated and patient was transferred to intensive care unit. Her past medical history was significant for diabetes mellitus, hypertension, epilepsy and atrial fibrillation. She had undergone multiple surgeries for cerebral meningioma excision. For the last five years, she was bedridden and on nasogastric feeding. In ICU, she required continuous inotropic support but there was no improvement in her condition. Tracheostomy was performed after 3 weeks of endotracheal intubation. The ventilatory management and tracheostomy care proceeded in an uneventful manner. As per institutional policy, the first change of tracheostomy tube was performed after 2 weeks post tracheostomy. One week after the change of tracheostomy tube (21 days post tracheostomy); air leak was noticed for the first time during mechanical ventilation. The patient was reviewed by otolaryngologist on-call, tracheostomy tube position was adjusted, and the cuff pressure was adjusted, but kept within permissible range, to prevent the air leak.
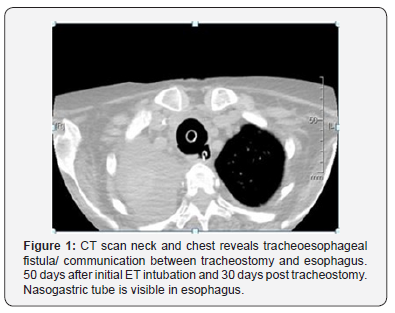
The air leak appeared again after 2 days (23 days post tracheostomy) and worsened to an extent that it was becoming difficult to maintain effective ventilation. Patient was also noticed to be developing significant abdominal distention, along with the air leak, required higher pressure settings for effective ventilation. A suspicion of Iatrogenic Tracheo-Esophageal Fistula was raised, and Thoracic surgery, Gastroenterology and Otolaryngology teams were consulted. The condition of the patient did not permit bronchoscopy and contrast swallow assessment so CT of neck and chest was organized. Overnight some bleeding was noticed from the oral cavity and tracheal stoma; this did not require any surgical intervention. The air leak worsened and became impossible to ventilate the patient. The tracheostomy tube was removed, and size 6 F cuffed endotracheal tube was inserted on 26 day post tracheostomy. CT scan of neck and chest (Figure 1) was performed and was highly suggestive of Tracheo-Esophageal fistula in the posterior wall of trachea. Unfortunately, the condition of the patient continued to deteriorate, and ventilation became progressively difficult. Endotracheal tube was changed again but with limited benefit. The patient expired 58 days after admission and 37 days post tracheostomy.
Patient’s medical file was reviewed retrospectively along with the radiological investigations. An interesting finding was noticed in the chest x-rays; there was a progressive increase in tracheal diameter at the site of tracheostomy tube cuff. These x-rays, shown in Figure 2, coincide with dates on which the air leak and progressive difficulty in mechanical ventilation was noticed.
Discussion
Patients admitted to ICU, intubated or tracheostomised for prolonged mechanical ventilation, are extremely unwell with nutritional and multi-system management issues. The development of TEF in such patients further complicates already complex management, significantly increasing the morbidity and mortality [14]. The incidence of cuff related TEF in such patients is around 1% [12,13]. History of traumatic intubation, high cuff pressure, high airway pressure, excessive cuffed tube movement, prolonged duration of cuffed tube placement, respiratory tract infections, hypotension, concomitant nasogastric tube, steroids, female gender, advanced age and insulin dependent diabetes are all important in contributing to development of cuff related TEF [5,15]. Our reported patient had all these contributing factors present.
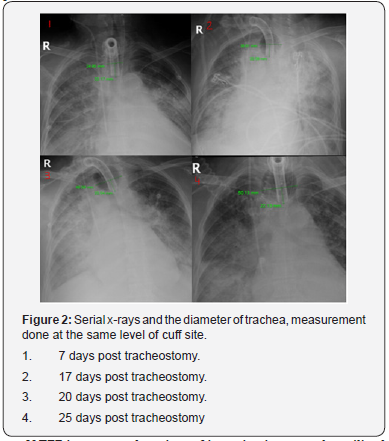
If TEF is suspected, variety of investigations may be utilized to confirm its presence. Although X-ray chest is not considered diagnostic for TEF but as it is performed regularly, at times every day, on patients admitted in ICU as it may provide important information. It provides information about the position of the cuffed tube, degree of distension of cuff, gaseous gastric distention and recurrent pneumonic patches [3]. These findings, although not diagnostic, may indicate the possible presence of TEF. We made an interesting and possibly important observation in the chest x-rays of our patient. We noticed a progressive increase in the diameter of tracheostomy tube cuff and adjoining trachea. Initially this increase was slow but later quite rapid and this related closely with the progression of her TEF related symptoms. This progressive increase in the cuff diameter was not due to any additional air insufflations by the medical staff. Possibly, as the capillary circulation was compromised due to cuff compression and poor hemodynamic status of the patient, there was ischemic tissue necrosis. This resulted in greater distension of the tracheostomy tube cuff as there was reduced tissue resistance. This cuff distension increased progressively as greater tissue destruction occurred. This is very effectively noted on the series of chest x-rays shown above.
The last chest x-ray (25 days post tracheostomy) shows a grossly distended tracheostomy tube cuff with a diameter of 50.13mm as compared to a diameter of 24.95 recorded 7 days post tracheostomy. On the 26th post tracheostomy day, patient could not be ventilated via tracheostomy tube due to unmanageable air leak and endotracheal tube was inserted. This proved effective as the cuff of endotracheal tube was positioned below the level of tracheostomy tube cuff and possible site of TEF. This progressive increase in the distension and diameter of tracheostomy tube cuff may be an important indicator of developing TEF. This finding has not been mentioned and used previously to predict and possibly prevent the development of TEF. We are reporting and mentioning the possible importance of progressive distension of tube cuff in relation to development of TEF for the first time in literature. Other investigations used in the diagnosis of TEF are bronchoscopy, esophagogram, esophagoscopy and echoendoscopic tracheobronchial examination [3,12], depending upon their availability and condition of the patient. In our patient, brochoscopy, considered as gold standard for diagnosis of TEF, could not be performed due to the rapidly deteriorating condition of our patient. C.T scan may also be helpful but only as an adjuvant investigation to confirm the clinical suspicion or diagnosis of TEF, but the diagnosis may be missed [16]. The condition of our patient allowed us to perform a CT scan only and this confirmed the suspicion of TEF.
The treatment of TEF will not be discussed here in detail but it involves non-surgical conservative and surgical management. These patients, especially the one in ICU, are critically ill and poor candidates for surgical intervention. Such patients are treated conservatively with an aim to prevent further deterioration of health and pulmonary functions, improve nutritional status and if condition allows an attempt to wean patient off ventilatory support [12,17]. Culture guided antibiotics may be required along with anti-reflux measures and medications. Naso-gastric tube should be removed, oral intake minimized and feeding gastrostomy or jejunostomy performed to improve nutrition and minimize contamination of lower trachea-bronchial tree with gastric and oral contents. If there is endotracheal or tracheostomy tube, then the cuff should be positioned below the TEF and cuff pressure kept at minimum possible while maintaining effective mechanical ventilation [3,4,5,12]. The surgical options are best considered for patients who are no longer on mechanical ventilation. Surgical options include stents, diversion procedures and layered fistula repair or layered fistula repair with muscle flap with or without resection of any tracheal stenosis [18-20]. The details of surgery are beyond the scope of this case report and not discussed here.
Conclusion
High index of suspicion for TEF should always be maintained in critical ICU patients who are on long term mechanical ventilation using cuffed endotracheal or tracheostomy tube. We recommend the use of serial chest X-rays and measurement of tracheal diameter at the level of cuff site to predict and prevent the formation of TEF. If progressive increase of diameter is noted, then it should be considered that further progression will result in the development of TEF. In such patients all possible steps should be adopted to prevent TEF and associated increase in morbidity and mortality. A large cohort study is required to support our recommendation of using serial chest X-ray to measure cuff and tracheal diameter for prevention and diagnosis of TEF.
References
- Andrews MJ, Pearson FG (1971) Incidence and pathogenesis of tracheal injury following cuffed tube tracheostomy with assisted ventilation: analysis of a two-year prospective study. Ann Surg 173(2): 249-263.
- Reed MF, Mathisen DJ (2003) Tracheoesophageal fistula. Chest Surg Clin N Am 13(2): 271-289.
- Paraschiv M (2014) Tracheoesophageal fistula - a complication of prolonged tracheal intubation Journal of Medicine and Life 7(4): 516-521.
- Petre B, Oprea I, Denisa Ghinescu D, Bidilică M, Ovidiu Bratu O, et al. (2016) The incidence of tracheoesophageal fistulas and it major determinan factors, Romanian Journal of Military medicine 35(3): 35-38.
- Payne KD, Anderson W Mcd, Romero MD, Wissing DR, Fowler M (1990) Tracheoesophageal Fistula Formation in Intubated Patients Risk Factors and Treatment with High-Frequency Jet Ventilation Chest 98(1): 161-64.
- Epstein SK (2005) Late Complications of tracheostomy. Respir Care 50: 542-549.
- Akmal A Hameed, Hasan Mohamed, Motasem Al-Mansoori (2008) Acquired tracheoesophageal Fistula due to high intacuff pressure. Ann Thorac Med 3(1): 23-25.
- Stauffer JL, Olsen DE, Petty HT (1981) Complications and consequences of endotracheal intubation and tracheostomy: A prospective study of 150 critically ill adult patients. Am J Med 70(1): 65-76.
- Lizy C, Swinnen W, Labeau S, Poelaert J, Vogelaers D, et al. (2014) Cuff Pressure of Endotracheal Tubes After Changes in Body Position in Critically Ill Patients Treated with Mechanical Ventilation Cuff Pressure of Endotracheal Tubes After Changes in Body Position in Critically Ill Patients Treated with Mechanical Ventilation 23(1): e1-8.
- Hofmann HS, Rettig G, Radke J, Neef H, Silber RE (2002) Iatrogenic ruptures of the tracheobronchial tree. Eur J Cardiothorac Surg 21(4): 649-652.
- Couraud L, Ballester ML (1998) Tracheoesophageal fistula Delaisement C. Acquired and STI management. Semin Thorac Cardiovasc Surg 8(4): 392-399.
- Bolca C, Pãvãloiu V, Fotache G, Dumitrescu M, Bobocea A, et al. (2017) Postintubation Tracheoesophageal Fistula – Diagnosis, Treatment and Prognosis Chirurgia 112 (6): 696-704.
- Diddee R, Shaw IH (2006) Acquired tracheo-oesophageal fistula in adults. Contin Educ Anaesth Crit Care Pain 6: 105-108.
- Shwethapriya R, Shenoy A, Nittala A (2013) Tracheo-oesophageal fistula - A disastrous complication of endotracheal intubation. Ind J Resp Care 2(1): 237-239.
- Cooper JD, Grillo HC (1969) The evolution of tracheal injury due to ventilatory assistance through cuffed tubes: a pathologic study. Ann Surg 169(3): 334-348.
- Pickhardt PJ, Bhalla S, Balfe DM (2002) Acquired gastrointestinal fistulas: classification, etiologies, and imaging evaluation. Radiology 224(1): 9-23.
- Mathisen DJ, Grillo HC, Wain JC, Hildenberg AD (1991) Acquired nonmalignant tracheoesophageal fistula of management. Ann Thorac Surg 52(4): 759-765.
- Grillo HC, Moncur AC, McEnany MT (1976) Repair of inflammatory tracheoesophageal fistula. Ann Thorac Surg 22(2): 112-119.
- Gudovsky LM, Koroleva NS, Biryukov YB, Chernousov AF, Perelman MI (1993) Tracheoesophageal fistulas. Ann Thorac Surg 55: 868-885.
- Macchiarini P, Verhoye JP, Chapelier A, Fadel E, Dartevelle P (2000) Evaluation and outcome of different surgical techniques for postintubation tracheoesophageal fistulas. J Thorac Cardiovasc Surg 119(2): 268-276.





























