Orbital Blowout Fractures in Manitoba: Demographics and Surgical Outcomes
Reda Elgazzar1* and Justin Diamond2
1Associate Professor of Oral and Maxillofacial Surgeon, Department of Dental Diagnostic & Surgical Sciences, Dr. Gerald Niznick College of Dentistry, University of Manitoba & Health Sciences Center, Canada
2General Dental Practitioner, Winnipeg, Manitoba, Canada
Submission: April 08, 2019; Published: April 22, 2019
*Corresponding author: Reda Elgazzar, Associate Professor of Oral and Maxillofacial Surgery, Department of Dental Diagnostic & Surgical Sciences, Canada
How to cite this article: Reda E, Justin Diamond.Orbital Blowout Fractures in Manitoba: Demographics and Surgical Outcomes. Glob J Oto, 2019; 20(1): 556026. DOI: 10.19080/GJO.2019.20.556026
Abstract
Objectives: Orbital blowout fractures are one of the most common occurring facial bone injuries. An orbital blowout fracture can occur in isolation or as a more complex craniofacial fracture pattern. The aim of this study was to investigate the etiology, incidence, and surgical outcomes of pure orbital blowout fractures in Manitoba, Canada.
Materials and Methods: A retrospective chart analysis was done on all cases of orbital blowout fractures seen at the Health Science Center in Winnipeg, Manitoba, Canada during the 10 year period of April 1, 2004 to March 31, 2014.
Results: There were 254 cases involving orbital blowout fractures that were seen and treated at the period of study. Only 91 of the 254 cases were diagnosed as pure orbital blowout fractures. Men outnumbered women (3:1) in all age categories. Violent assaults and motor vehicle collisions (MVCs) were the leading etiology of injury. The most common associated, immediate symptoms involved in all cases were diplopia, ecchymosis, pain, restricted eye movement, enophthalmos and crepitus. Sub ciliary and transconjunctival approaches were found to be the most common surgical techniques used in this study. Nearly 80% of all cases in this study were repaired with titanium mesh implant material and another 10% having used Medpor porous polyethylene (PE). Postoperative complications, including diplopia, pain, blurred vision, V2 numbness, enophthalmos and chemosis, entropion & extropion, were reported in 24/91 (26.3%) patients; only 6/24 (25%) cases needed further surgery.
Conclusion: Consistent with other studies, titanium implant, followed by porous PE were found to be the most commonly used implants for surgical repair of pure orbital blowout fractures. Sub ciliary and transconjunctival surgical approaches as reviewed in this study showed acceptable long-term results and minimal post-operative complications.
Keywords: Orbital Blow-out Fracture; Surgical Approaches; Orbital Reconstruction; Surgical Complications
Introduction
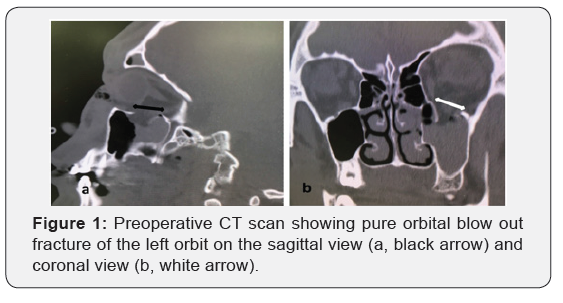
Orbital blowout fractures are one of the most common occurring facial bone injuries [1-4]. Pure orbital blowout fractures occur in the inferior (and medial) wall of the orbit caused by blunt trauma to the orbit (Figure 1). Cases of pure orbital blowout fractures have increased in the past 10 years. These injuries are usually caused by blunt force trauma in the periorbital region including violent assault, motor vehicle collisions (MVCs), falls, sports injuries, and blast injuries [1,2], [5-8]. Failure to immediately recognize, diagnose and treat these injuries can result in substantial cosmetic and functional problems, including diplopia, enophthalmos, movement limitation, and paresthesia [2]. Retrospective chart analysis done on all cases of orbital blowout fractures seen at the Health Science Center (HSC) in Winnipeg, Manitoba, Canada between April 1, 2004 and March 31, 2014 shows 254 noted cases involving fractures to the orbit. This included 91 cases of pure orbital blowout fractures. The two current theories regarding the mechanism of action for the “blowout” fracture are the buckling and hydraulic theories [2-4], [7,9,10].
The buckling theory, first described by Lefort, claims a force indirectly transmits pressure from the orbital rim along the bones to the floor of the orbit. This causes a rippling effect of the orbital walls causing the bones to distort and eventually fracture. From this, an anterior-posterior compression of the bones and subsequent inferior buckling (cracking) of the bones into the maxillary sinus [3,4,9]. The hydraulic theory argues that the direct transmission of pressure from the ocular globe and intraorbital content to the peri-ocular structures eventually transmits to the orbital floor, blowing it out [1,3,4,9]. Most fractures occur on the posterior medial region, where the bone is the thinnest. The increased intra-ocular pressure simultaneously fractures the bones and pushes the orbital contents into the sinus. Although the buckling theory has recently been criticized, recent studies have concluded that both theories remain valid [3,4]. The most common side effects of orbital blowout fractures include diplopia, enophthalmos, decreased extraocular movement, hypoesthesia (V2), and periorbital ecchymosis [9,7]. The aim of this study was to investigate the etiology, incidence, and surgical outcomes of pure orbital blowout fractures in Winnipeg, Manitoba, Canada over a ten-year period.
Materials and Methods
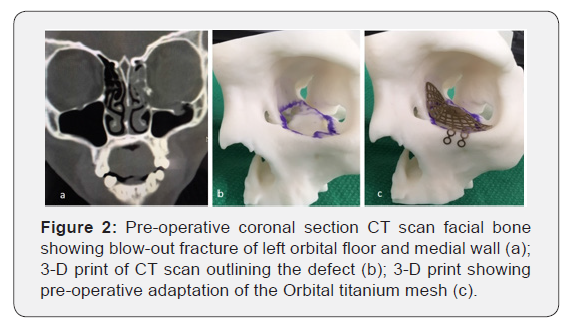
A retrospective chart analysis was done on all cases of orbital blowout fractures treated at the Health Sciences Centre in Winnipeg, Manitoba, Canada during the ten year period from April 1, 2004 to March 31, 2014. Analysis showed 254 cases involving trauma to the orbit. However, only 181 charts included sufficient relevant data for further study. To be included in this study, cases had to involve orbital floor and/or medial orbital wall fractures. Pure orbital blowout fractures traditionally involve only the floor of the orbit, but the medial wall was included due to the high degree of involvement in these injuries; this is attributed to the medial wall being extremely thin and fragile. Exclusion was determined for cases that had orbital rim or other orbital wall fractures, or cases that did not have orbital floor and/or medial wall fractures, or patients who did not require orbital surgical intervention. Analysis of pre-operative CT scans (Figure 2) and medical records, including intra-operative notes, showed that only 91 of those cases met these inclusion criteria. A data capture sheet was created for each patient, which included gender, age, etiology of injury, pre-operative symptoms, and surgical approach, implant material, post-operative sequela as well as post-operative complications. Minitab 18 statistical package was employed to compute the descriptive statistics and data analysis.
Results
Age and Sex
Of the 91 patients assessed, the age range was from 17-78 with an average age of 35.7 years. There was a 3:1 incidence of male to female, where 68/91 (75%) were male patients. Grouping the patients in ten-year age intervals (Figure 3), there were 23 (25%) patients under 25 years old, 32 (35.2%) patients between 26-35 years of age, 14 (15.4%) patients between 36-45 years of age, 14 (15.4%) patients between 46-55 years of age and 8 (8.8%) patients over the age of 55. Incidence of injury was the highest in patients from 26-35 years of age, with males in that group being the highest group affected.
Etiology
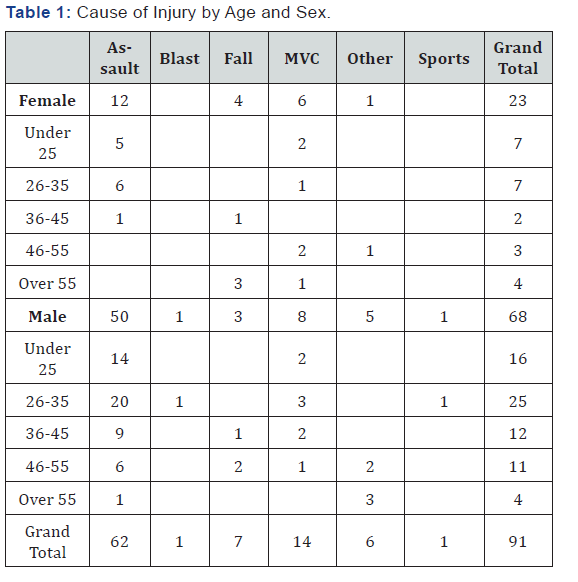
Out of the 91 cases, 62 (68%) were caused by violent assault (Table 1). This represented the highest incidence compared to any other cause for both male and female patients. Violent assault was also the most common cause of orbital blowout injuries in all but two age categories for both male and female patients. Motor vehicle accidents (MVC) were the second leading cause of injury, accounting for 14 (15.4%) injuries. Other causes included falls, which caused a further seven (7.7%) injuries, other non-identified causes, which caused six (6.6%) injuries, one sports-related injury (1.1%), and one (1.1%) blast injury.
Location of Injury
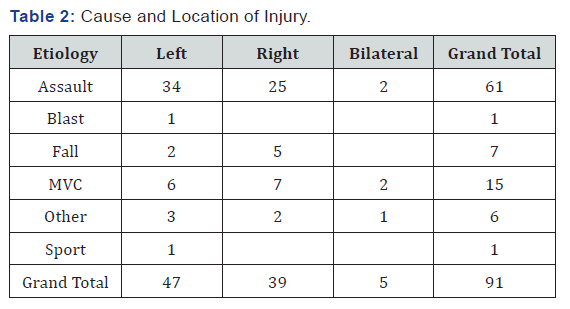
47/91 (51.6%) of cases included injuries on the left side. Another 39/91 (42.9%) of cases included injuries on the right side. Out of the 47 cases involving injuries on the left side, 34 were as a result of violent assaults. 24 cases of assault resulted in injury to the right side (Table 2). In other studies, injuries occurred at a higher prevalence on the left. These numbers relate to the higher prevalence of right-handed dominant populations. Although injuries on the left outnumbered those on the right in this study, the injuries on both the left and the right were more similar in this study than in others. In 5/91 (5.5%) cases, injuries occurred bilaterally.
Pre-Operative Ocular Symptoms
Pre-operative symptoms included diplopia in 62/91 (68.1%) cases, ecchymosis in 85/91 (93.4%) cases, pain in 73/91 (80.2%) cases, and crepitus in 6/91 (6.6%) cases. Enophthalmos was found in 17/91 (18.7%) cases and restricted eye movement in 29/91 (31.9%) of cases.
Surgical Techniques

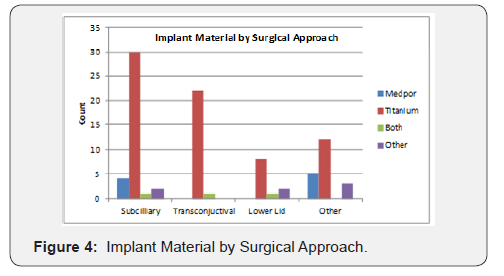
Treatment of facial trauma at the Health Sciences Centre is based on a rotation schedule between the plastic surgery and oral maxillofacial surgery departments. Case determination is assigned based on an on-call rotation, patient’s needs, and the nature of primary and associated injuries. Since the Health Sciences Centre is a level I trauma center, multiple specialists are often present upon first assessment and may even be present in the operating room. Plastic surgery teams were the primary surgical team in 39/91 cases. Oral maxillofacial surgery surgical teams were responsible for 51/91 cases. One patient chart was missing information on the primary care team. Treatment of pure orbital blowout fractures included surgery through sub ciliary incision in 37/91 (41%) patients, transconjunctival incision in 23/91 (25%) patients, and 31/91 (34%) of patients were treated by “other” approaches including Gilles approach, upper buccal sulcus incision, and existing lacerations (Figures 2 & 3), (Table 3). Treatment of 72/91 (79%) patients were repaired with titanium sheeting and screws, while only 9/91 (10%) were repaired with Medpor sheeting. Of the remaining cases, 3/91 (3%) were treated using both Titanium and Medpor combinations, and 7/91 (8%) were treated using other materials (Figure 4).
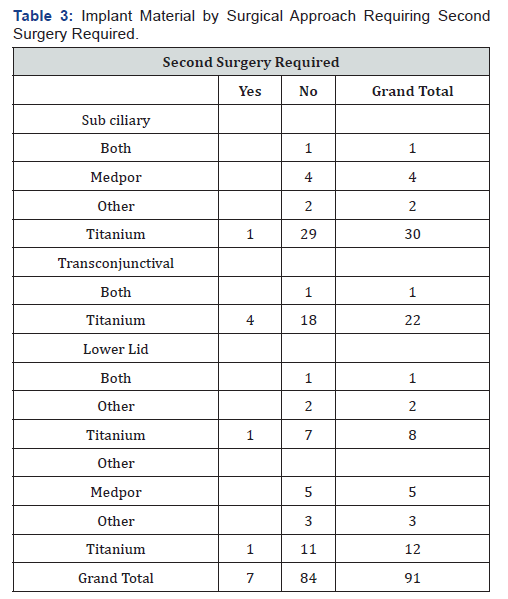
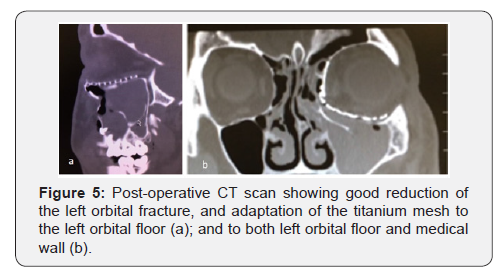
Post-Operative Symptoms and Complications
Post-operatively, all patients had CT scan (Figure 5 a & b) as well as examined clinically during their follow up periods to identify any patients’ complaints and complications. Postoperative sequela included diplopia, decreased extra-ocular movement, pain, blurred vision, enophthalmos, entropion, extropion, edema, subconjunctival hemorrhage, headaches, and V2 hypo/paresthesia. 24/91 (26.4%) patients suffered symptoms greater than two week post-operatively, all of them were treated with titanium implant (Table 3). 17/24 patients (71%) improved within few weeks postoperatively. 7/24 (29%) patients necessitated further surgery due to various reasons were mainly treated with titanium implants (Table 3). The 7/24 cases required a second surgery included: 3/7 to correct a mal-positioned implant, 1/7 to correct entrapment of orbital contents, 1/7 to correct upper lid ptosis, 1/7 to correct chronic epiphora and extropion. 1/7 to correct entropion. No postoperative loss of visual acuity or infection were reported.
Discussion
There are two categories of orbital blowout fractures, pure and impure based on the involvement of the orbital rim; the later involves the orbital rim [2,7]. An orbital blowout fracture can occur in isolation or as a more complex craniofacial fracture pattern [3,6]. Soft tissue injury may or maybe not be involved. Blowout fractures are purely internal fractures which are confined to the orbital walls and therefore do not involve the orbital rim.8 Pure orbital blowout fractures involve the medial wall of the orbit and the orbital floor and herniate (“blow-out”) the orbital contents into the adjacent sinuses [2,3,6,7]. These fractures involve the internal walls of the orbit with entrapment of soft-tissues, which limits ocular mobility and causes diplopia and enophthalmos [2,11]. Reviewing pure orbital blowout fracture treatment modalities at the Health Sciences Centre over the 10-year period, found 254 cases. Of those, 91 could be classified as pure orbital blowout fractures involving only the floor and/or medial wall of the orbit. These injuries were mostly caused by assault, motor vehicle collisions, falls, and sports injuries [4,7,12]. The main etiological factor for pure orbital blowout fractures was violent assault, corresponding with a recent rise in violent assault cases [4]. MVCs in this study were the second leading cause contributing to both pure and impure blowout fractures but presented roughly 1.5 times more as impure fractures. This can be a factor of high-energy collisions where there are a number of different systems involved with extensive, non-specific trauma. Other similar studies have made the connection between MVCs and impure fractures as well as links between low-energy injuries such as violent assaults and pure fractures [2]. While this study shows there are more impure fractures (20) than pure fractures (14) caused by MVCs (high-energy trauma) and more pure fractures (62) than impure fractures (55) caused by assaults (low-energy trauma) the incidence of cases are too similar to conclude that there is an association in this study. Although other studies have found evidence to support this association, these findings were not present in this study. Orbital blowout fractures caused by falls were most prevalent in women over the age of 55.
Due to the high number of violent assaults (68.1%) and MVCs (15.4%), it was found that there was no significant observance of left sided injuries compared to other similar studies. In these studies, the number of left-sided injuries was more pronounced due to the high prevalence of right-handed individuals. It can be hypothesized that the nature and severity of the violent assaults as well as the significance of the highimpact, generalized trauma seen in MVCs, the number of leftsided pure orbital blowout fractures would have been reduced as the injuries would have been more extensive. A large majority of injuries to the left side of the face were excluded for including injuries to the orbital rim and other surrounding structures. The extensive analysis of orbital blowout fractures shows that the number of male patients out numbers female patients for almost every category, in multiple studies [2,3,13,8,12]. In this study, men outnumbered women 3:1. Age ranges for this study were from 17 to 78 years. While the age range is extreme, most studies show that the highest incidence of injuries occurs between the ages of 20-35 years [1-3,7]. Observed in this study, the age group with the highest incidence of injury was 26-35 in both genders. Historically the incidence of blowout fractures in those younger than 10 years is very low. This is presumably because a larger cranium and less pneumatization of the paranasal sinuses, especially the maxillary sinus in younger children [2].
The most frequent sequela (pre-operative symptoms) of pure orbital blowout fractures includes diplopia, enophthalmos, as well as limitation in extra-ocular movement, ecchymosis, and pain [2,4,9,10]. Restricted ocular movement causes diplopia from trapping of the orbital contents/extraocular contents or damage to the nerves innervating the extra-ocular muscles. Enophthalmos is usually seen associated with an enlarged orbital cavity after a blowout fracture. This can sometime be hidden initially due to swelling of the surrounding tissues [4]. The nature of this injury is of trauma origin. With the high incidence of violent assaults and MVCs causing trauma in this study, there are multi-system involvements in many of the cases. This led to many patients being admitted to the hospital with major facial trauma where the status of the orbit that could not be immediately assessed. In all cases, an initial, pre-operative CT scan was preformed to assess the status of the orbit and the orbital contents [7]. Management of patients falls into three categories: conservatively, closed reduction, and open reduction. Conservative treatment involved pain and symptom management without reduction or repair of injuries by active or surgical means. Closed reduction is the manipulation of bones without surgical means. Finally, open reduction is manipulation of the bones with or without an implant prosthetic by surgical means. Cases involving treatment without surgical intervention,conservative treatment, and those with closed reduction were excluded from the study. Cases of open reduction were included.
Kochhar and Byrne claim that the timing of surgery to repair complex midfacial fractures may vary; some surgeons prefer to wait for edema to subside before treatment, but others argue that it is best to restore bony architecture early. Additionally, in severe trauma situations, stabilization of the patient with life-threatening injuries takes priority [14]. Treatment of the injuries can be done immediately, within two weeks or after two weeks during a time of prolonged observation [3,4,9]. Immediate surgical treatment is recommended in cases of fractures characterized by orbital soft tissue entrapment with non-resolving oculocardiac reflex, early enophthalmos or hypo Globus associated with marked facial asymmetry [3,9,15]. Several studies also recommended early intervention in children with evidence of muscle entrapment which leads to fat ischemia and result in permanent diplopia [3,16]. Surgical repair within two-week time is justifiable for adults with symptomatic diplopia with positive force duction testing, evidence of muscle entrapment and little clinical improvement over that time. Surgical repair should be considered with increasing symptoms (V2 hypothesia) or orbital floor defect greater than 50% with concurrent enophthalmos [5,9,17].
Baino comments that medical treatment without surgery may be preferred in patients who present with weak enophthalmos (<2mm), a lack of marked hypo Globus, absence of muscle or soft tissue entrapment, good ocular mobility, a fracture involving less than 50% of the orbital floor, no diplopia, or a patient where surgical intervention is contraindicated.4 Surgical repair might be delayed due to the absence of clinical signs such as enophthalmos due to periorbital edema and hemorrhage. A study done by Hawes and Dortzbach in 1983 showed the usefulness of CT imaging in predicting post-injury enophthalmos, and they recommend surgical repair within two weeks’ time if greater than half of the orbital floor is depressed [9,18]. In this study the time from injury to surgery ranged between 0 – 24 days, with the average time, excluding outliers, being 6.9 days. Management of orbital injuries has become standardized over the past century. Surgical repair of the injuries was accomplished via three main surgical approaches: sub ciliary incision, transconjunctival incision, and sub-tarsal incisions. The specific treatment is individualized and dependent on the surgeon and the presentation of the injuries [4,7]. The specific technique is determined with attention to cosmetic and functional outcomes. Sub ciliary incisions are performed through in the lower eyelid 2 mm below the edge of the eyelid and there is little to no risk of the lower eyelid shortening or ectropion [19]. The trans conjunctional approach is cosmetically preferred and is performed by pulling the lower eyelid forward with the incision made without involving the skin or muscle. This approach is surgically similar in providing exposure and access to the orbital floor but has shown to be aesthetically superior to the other two approaches and has minimal complications but increased risk of entropion. This method minimizes scar formation but offers more limited access to the medial portion of the orbital floor [20].
The predominant surgical approach in this study was sub ciliary (40.7%), which was associated with 8.8% incidence of long-term complications of the overall cases in this study. Recently, transconjunctival approach has been used excessively at our center compared to the sub ciliary approach. One case treated via sub ciliary approach required a second surgery to remove the orbital floor plate due to a medial rectus entrapment. In this case, the patient experienced diplopia in all gazes, loss of balance, and limited extraocular movement. CT results confirmed the diagnosis and the titanium mesh orbital floor plate was removed immediately. Residual diplopia remained for roughly four months following the second operation but was only present in extreme gaze. It was determined in consultation with the oral maxillofacial team and ophthalmologists that no further intervention would be required. The transconjunctival approach was the second most used surgical approach, accounting for 23/91 (25.3%) of cases. 11/91 (12%) patients treated in this study by transconjunctival approach suffered from long-term complications. Most complications again involved residual diplopia, enophthalmos, decreased range of motion and V2 hypothesis. All patients reported an improvement in symptoms within the first four months after surgery. Sub-tarsal incision made up 11 (12%) cases in this study. As this approach leaves the patient with a less aesthetic appearance, recent trends have been to preform orbital surgery via the sub ciliary and transconjunctival approaches [7]. Two long-term complications were noted with lower lid incisions, representing 2.2% of all cases.
In addition to these surgical approaches, the 20 remaining cases in this study were treated by “other” surgical means. These include incisions via existing facial lacerations, upper buccal sulcus, bi-coronal, and Gillies incisions. Three of these cases involved long-term complications with one requiring subsequent surgery. All surgical approaches showed a relatively low level of complications [7,8]. Transconjunctival surgeries showed the highest level of post-operative complications, apparent in 12% of cases. The high reported failure rate for this technique can be attributed to the higher incidence of use, the larger size of bone defects presents in cases when titanium implants are preferred. Reconstruction materials can vary from autologous bone (from the ribs, mandible, calvarial or iliac bone), bio ceramics (hydroxyapatite), metals (titanium mesh), polymers and composites [4,5]. To date, there is no recognized consensus on the best choice of biomaterials/implants for orbital floor reconstruction. The choice for optimal repair is influenced, in part, by the clinical characteristics of the injury, cost, the patient’s clinical history, as well as the opinion and experience of the surgeon [4,5,8]. Wang et al. examined the success of titanium, PE and autologous bone, and found that all patients had good results. They concluded that porous PE and titanium would be most desirable, as they do not require a second surgery to harvest bone for re-implantation. In cases studied at HSC, titanium implant material was overwhelmingly the material of choice. 79.1% (72/91) of all cases were repaired using titanium mesh plates and screws.
Titanium has been used in craniofacial reconstruction and orbital floor repair for decades (Figure 4A). It is highly biocompatible and has high rigidity and strength, making it ideal for bone reconstruction. Titanium also has a high ability to be Osseo integrated into surrounding tissues and is particularly useful for large orbital floor fractures requiring significant rigidity and strength [4]. Titanium, as tested in other studies, has shown to be extremely safe and there have been minimal postoperative infections reported in patients treated with titanium implants. A report done in 2003 by Ellis and Tan showed that compared to cranial bone grafts, titanium mesh showed better overall reconstruction, while noting the existence of individual variability [4,21]. Despite its many advantages, there have been some reports of serious post-operative complications with titanium mesh implants. This material is non-absorbable and cannot be replaced by new soft or bone tissue, meaning the implant will essentially remain in situ indefinitely. Lastly, there is the associated cost of the custom-made titanium devices compared to other available materials [7,22].
Medpor sheeting is a porous ultra-high density polyethylene (PE) material. It is available commercially for nearly 20 years as sheets of various thickness (0.4-1.5mm) and sizes that are easily adapted by the surgeon for use in each case (Figure 4B). The presence of pores in the implant material promotes tissue ingrowth and implant vascularization while reducing foreign body reactions and capsule formation.4 A post-traumatic study by Lupi et al in 2004 has shown that porous PE sheets represent a stable platform for orbital soft tissue growth that did not result in implant migration, extrusion or enophthalmos [23]. While autogenous bone grafting is still considered the “gold standard” for orbital reconstruction and a metric to which all other materials are compared its major disadvantage is the potential morbidity associated with the donor site. Medpor has showed comparable results to autogenous bone grafting in a 2008 study by Wajih et al. [12] but was concluded that due to both the potential morbidity from the secondary (donor) site and longer operating times, Medpor would be a better implant choice. 13 A comparative study by Wang et al published in 2008 between titanium mesh implants and porous PE show both materials were found to be ideal for orbital floor repair. Titanium mesh was used in fractures with large defects that were not easy to fix without obvious enophthalmos, and porous PE could be used in fractures that needed to have orbital volume restored [24]. Similar to the results of titanium implants, porous PE has still been reported to have significant complications associated with its use in similar studies.4 Medpor was used in 9/91 (9.9%) of cases in this study. In three cases in this study, both Medpor and titanium mesh (Medpor Titan) were used for reconstruction of orbital defects [25].
Conclusion
Consistent with other studies, titanium implant, followed by porous PE were found to be the most commonly used implants for surgical repair of pure orbital blowout fractures. Sub ciliary and transconjunctival surgical approaches as reviewed in this study showed acceptable long-term results and minimal postoperative complications. Postoperative complications were reported in 24/91 (26.3%) patients. Patients with postoperative complications not showing acceptable improvements at two weeks post-operatively were reassessed and treated accordingly.
References
- Kwon JH, Kim JG, Moon JH, Cho JH (2008) Clinical analysis of surgical approaches for orbital floor fractures. Archives of Facial Plastic Surgery 10(1): 21-24.
- Shin JW, Lim JS, Yoo G, Byeon JH (2013) An analysis of pure blowout fractures and associated ocular symptoms. J of Craniofac Surg 24(3): 703-707.
- Ethunandan M, Evans B (2011) Linear trapdoor or “white-eye” blowout fracture of the orbit: not restricted to children. Brit J of Oral and Maxillofac Surg 49(2): 142-147.
- Baino F (2011) Biomaterials and implants for orbital floor repair. Acta Biomaterialia 7(9): 3248-3266.
- Zunz E, Blanc O, Leibovitch I (2012) Traumatic orbital floor fractures: Repair with autogenous bone grafts in a tertiary trauma center. J of Oral and Maxillofac Surg 70(3): 584-592.
- Shamir D, Ardekian L, Peled M (2008) Blowout fracture of the orbit as a result of blast injury: case report of a unique entity. J of Oral and Maxillofac Surg 66(7): 1496-1498.
- Brady SM, Mcmann MA, Mazzoli RA, Bushley D, Ainbinder DJ, et al. (2001) The diagnosis and management of orbital blowout fractures: Update 2001. The Am J of Emerg Med 19(2): 147-154.
- Burnstine MA (2002) Clinical recommendations for repair of isolated orbital floor fractures. Ophthalmol 109(7): 1207-1210.
- Cruz AAV, Eichenberger GCD (2004) Epidemiology and management of orbital fractures. Current Opinion in Ophthalmology 15(5): 416-421.
- Waterhouse N, Lyne J, Urdang M, Garey L (1999) An investigation into the mechanism of orbital blowout fractures. Brit J of Plastic Surg 52(8): 607-612.
- Wajih WAS, Shaharuddin B, Razak NHA (2011) Hospital Universiti Sains Malaysia experience in orbital floor reconstruction: autogenous graft versus medpor. J of Oral and Maxillofac Surg 69(6): 1740-1744.
- Hupp J, Tucker M, Ellis E (2013) Contemporary Oral and Maxillofacial Surgery, (6th Edn),. Mosby, Vital Book file 496.
- Kochhar A, Byrne PJ (2013) Surgical management of complex midfacial fractures. Otolaryngologic Clinics of North America 46(5): 759-778.
- Sires BS (1999) Orbital trapdoor fracture and oculocardiac reflex. Ophthalmic Plastic & Reconstructive Surg 15(4): 301.
- Bansagi ZC, Meyer DR (2000) Internal orbital fractures in the pediatric age group. Ophthalmol 107(5): 829-836.
- Hawes MJ, Dortzbach RK (1983) Surgery on orbital floor fractures. Ophthalmol 90(9): 1066-1070.
- Vaibhav N, Keerthi R, Nanjappa M, Ashwin DP, Reyazulla MA, et al. (2015) Comparison of ‘sutureless’ transconjunctival and subciliary approach for treatment of infraorbital rim fractures: a clinical study. J of Maxillofac and Oral Surg 15(3): 355-362.
- Santosh BS, Giraddi G (2011) Transconjunctival preseptal approach for orbital floor and infraorbital rim fracture. J of Maxillofac and Oral Surg 10(4): 301-305.
- Ellis E, Tan Y (2003) Assessment of internal orbital reconstructions for pure blowout fractures: Cranial bone grafts versus titanium mesh. J of Oral and Maxillofac Surg 61(4): 442-453.
- Hughes C, Page K, Bibb R, Taylor J, Revington P (2003) The custommade titanium orbital floor prosthesis in reconstruction for orbital floor fractures. Brit J of Oral and Maxillofac Surg 41(3): 209.
- Lupi E, Messi M, Ascani G, Balercia P (2004) Orbital floor repair using Medpor porous polyethylene implants. Invest Ophthalmol Vis Sci 45(E): 4700.
- Wang S, Xiao J, Liu L, Lin Y, Li X, et al. (2008) Orbital floor reconstruction: a retrospective study of 21 cases. Oral Surg, Oral Med, Oral Path, Oral Rad, and Endodontology 106(3): 324-330.
- Mathog RH (1998J) Surgery of traumatic defects of the orbital floor. Archives of Otolaryngology-Head & Neck Surgery 124(12): 1402.
- Tabrizi R, Ozkan TB, Mohammadinejad C, Minaee N (2010) Orbital floor reconstruction. J of Craniofac Surg 21(4): 1142-1146.





























