Outcomes of Subtotal Extracorporeal Septoplasty in Deviated Noses
Irfan ul Shamas*
Consultant ENT JK Health Services, Kashmir University, India
Submission: February 12, 2019; Published: March 05, 2019
*Corresponding author: Irfan ul Shamas, Consultant ENT JK Health Services, Kashmir University, India
How to cite this article: Irfan ul Shama. Outcomes of Subtotal Extracorporeal Septoplasty in Deviated Noses. Glob J Oto, 2019; 19(4): 556016. DOI: 10.19080/GJO.2019.19.556016
Abstract
Grossly deviated nasal septum is a challenge for an operating surgeon. Endonasal approaches fail to correct high and caudal deviations of a deviated nasal septum completely. Correcting a deviated nasal septum is a pre requisite in any rhinoplasty procedure. Gubisch has first reported in 1995 about extracorporeal septoplasty (ECSP). To report my experience of 50 patients who underwent “subtotal extracorporeal septoplasty” this study was done from March 2015 to March 2018 in District Hospital Pulwama and Florence Hospital Srinagar. Patients pre and post-operative evaluation was done by photographs, NOSE question is and nasal endoscopy. There was significant aesthetic and functional improvement using this technique. Complications were not higher than endonasal conventional techniques except for tip and dorsal firmness for which a proper written informed consent was taken. On the basis of results obtained, this technique is highly recommended in cases of grossly deviated nasal septum with external nasal deformity.
Keywords: Extra Corporeal Septoplasty; Rhinoplasty; Deviated noses
Introduction
Septal deviations cause both functional and aesthetic impairment. Most of the rhinological practice revolves around the symptoms caused by deviated nasal septum. A cadaver study in United States in over 2000 cadavers has demonstrated deviated nasal septum in up to 75% population [1]. While most of the patients with deviated nasal septum pass on their life asymptomatically, however some patients need surgical correction of the septum to alleviate them of the symptoms associated with DNS (deviated nasal septum). Septoplasty ranks as the third most common head and neck operation in the United States, with around 260,000 cases being performed annually in the ambulatory surgery setting [2]. Dorsal and caudal deviations of septum are difficult to correct by conventional endonasal septoplasty. Extra corporeal septoplasty was first described by King [3], Ashley and Parret in 1950s however Gubisch [4] in 1995 published his experience on 1012 patients who underwent extracorporeal septoplasty (ECSP) with encouraging functional and aesthetic results. Subsequently the technique of ECSP became popular enough among rhinologists and plastic surgeons. Many surgeons were critical about this technique regarding stability at keystone area and difficulty in technique. Gubisch described the technique with areas of fixation at three points i.e. caudal end of the nasal bones, upper lateral cartilage and maxillary crest. He accomplished this by drilling a hole through nasal bones and the nasal spine and suturing the newly reconstructed neo septum.
Method
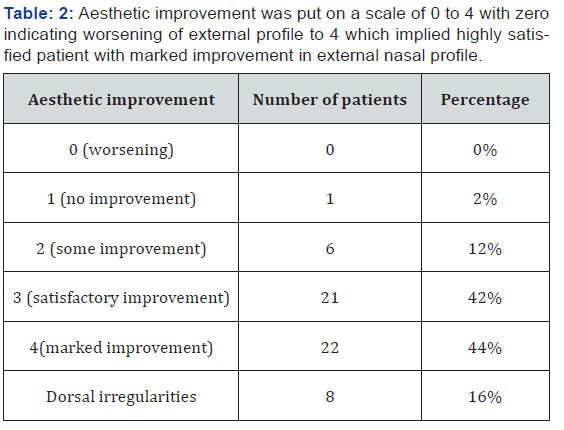
Fifty patients who underwent extra corporeal septoplasty (ECSP) from March 2015 to March 2018 by the author in District Hospital Pulwama (secondary care hospital) and Florence Hospital were included in this study. Patients with dorsal DNS and grossly impacted DNS with external nasal deviation were included this study. Patients with caudal and mild DNS with no external nasal deviation were excluded from this study. Patients who had underwent any prior septal surgery were also excluded from this study. Data analyzed included age, sex, symptomatology improvement (NOSE Score), aesthetic improvement and complications. NOSE is a questionnaire which serves to evaluate, from a subjective point of view, the obstructive nasal symptomatology. It is brief, valid, reliable, and responsive to any minimum change in the patient’s clinical status. It considers [5] parameters: nasal congestion, nasal obstruction, respiratory difficulties, sleep disturbances, and respiratory disturbances under physical exercise. The scale ranges from 0 where the parameter is considered nonrepresentative of a problem for the patient to 4, where nasal obstruction constitutes a severe problem. Patients compiled the NOSE scale before surgery and at 3 and 6 months after the date of surgery. Aesthetic improvement was put on a scale of 0 to 5 with zero indicating worsening of external profile to 4 which implied highly satisfied patient with marked improvement in external nasal profile.
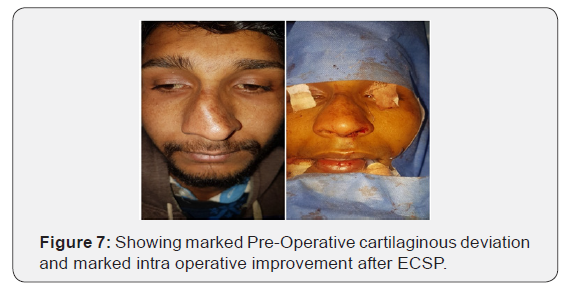
The extracorporeal septoplasty was always performed as follows. All operations were performed under general anaesthesia, and an open inverted-V approach (external) was used. The domes are divided in the midline, and the upper lateral cartilages were released by sharp dissection, exposing the septum on all sides. Then, the septum was released from the anterior nasal spine and the maxillary crest. The upper lateral cartilages were split from the septum by 11 number blades. The septum was released posteriorly by making a vertical fracture in ethmoidal bone few centimeters posterior to its attachment with the quadrangular cartilage. The septum was then removed enbloc for its extracorporeal straightening. This technique did not remove the entire septum but retained most part of the bony septum posteriorly and removal of only few centimeters of bony septum attached to the cartilage was removed making it a “subtotal extra corporeal septoplasty”. The septum removed is reconstructed on the table. Bilateral spreader grafts are placed on dorsal part of septum and fixed in place with 4-0 Polydiaxone sutures at two or three points. Lateral osteotomies are performed by external subcutaneous method and a medial osteotomy was performed on either side endonasally. Collumellar strut, tip work and rim grafts (if needed) were done in all cases before closure by 4-0 vicryl. A small ribbon pack was placed for 24 hours. An external splint by paper tape over the dorsum was kept for 10 days. Free diced cartilage or fascia over dorsum was not used in any case.
Results
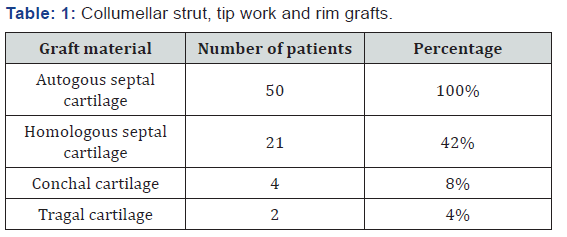
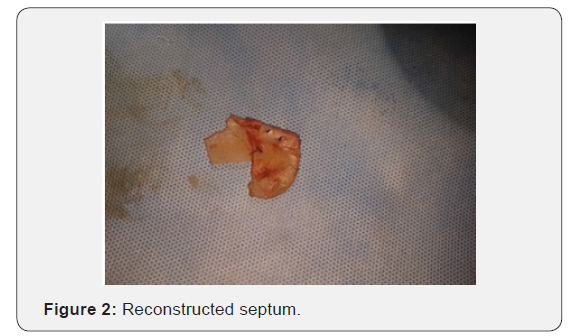
Fifty patients underwent extracorporeal septoplasty (ECSP) in District hospital Pulwama and Florence Hospital Srinagar for symptoms associated with deviated nasal septum and aesthetic improvement. All the patients were primary septorhinoplasties. A detailed consent with pre and post-operative photographs in all planes were taken. All patients underwent surgery under hypotensive general anaesthesia. Age of patients ranged from 17 to 46 years with an average age of 29 years. Males (n=30) outnumbered females(n=20) in the ratio of 3:2. Homologous septal cartilage (preserved in dilute absolute alcohol) was used in 16 patients besides autologous septal cartilage (Table 1). Improvement in symptoms were measured subjectively by using Nasal Obstruction Symptom Evaluation score (NOSE score). 42 patients had improvement in their NOSE scores with maximum improvement in patients(n=12) with severe nasal deviation before surgery. Eight patients had no improvement in their NOSE scores. Aesthetic improvement was put on a scale of 0 to 4 with zero indicating worsening of external profile to 4 which implied highly satisfied patient with marked improvement in external nasal profile (Table 2). Complications if any were noted. There were 3 (6%) patients who had septal perforation one was with saddling and was reoperated and other two patients had asymptomatic septal perforations. Four (8%) patients had infection of wound site which was managed by local care and systemic drugs. Seven (14%) patients had complaints of stiffness of dorsum and tip. Eight (16%) patients had synechiae post-surgery which were managed by release and spacing subsequently (Table 3). Dorsal irregularities were noticed in 8 patients (16%) (Figures 1 & 2).

Discussion
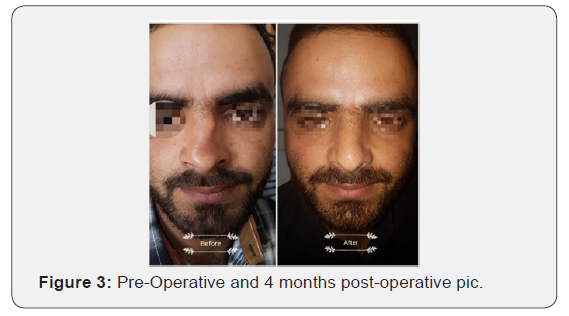

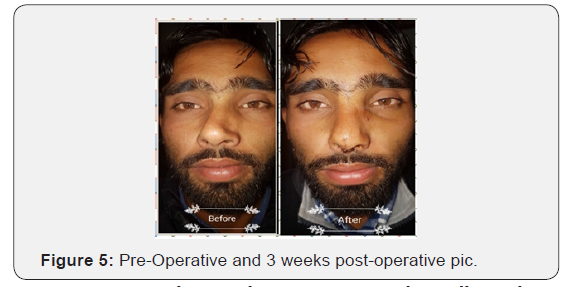
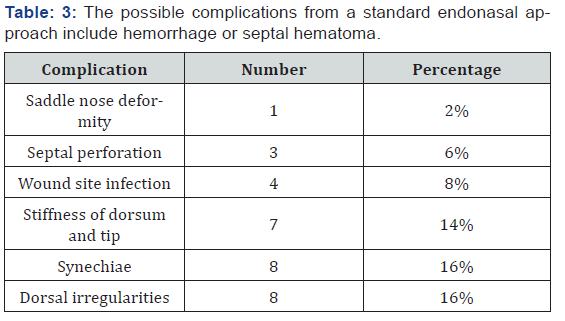
Extra corporeal septoplasty is a new and rapidly evolving technique. Extra corporeal septoplasty was first described by King [6], Ashley and Parret in 1950s however Gubisch [4] in 1995 published his experience on 1012 patients who underwent extracorporeal septoplasty (ECSP) with encouraging functional and aesthetic results. Subsequently the technique of ECSP became popular enough among rhinologists and plastic surgeons.However, there are not many studies about complications of the technique with a few modifications. The possible complications from a standard endonasal approach include hemorrhage or septal hematoma (6-14 %), cerebrospinal fluid leak (rare), infection (0.048-2.5 %), overcorrection (2 %), septal perforation (1-6.7 %), adhesions or synechiae (7 %), hyposmia (0.3 %), and aesthetic deformities (4 %-8 %). All these complications are also possible when performing the extracorporeal technique, but can be avoided by nasal splint, dosal free diced cartilage with or without fascia [5]. In my study there was supra tip depression, saddling with septal perforation in one pateint who was re operated. There were septal perforations in three patients (6%) which is comparable with endonasal techniques. There were minor wound site infections in four (8%) patients which was managed with local and systemic antibiotics and wound care. Stiffness of nasal dorsum and tip was a complication in [7] (14%) patients which is higher than in endonasal techniques. Because most of these patients were operated for cosmetic outcomes, this complication was ignored by these patients. Dorsal irregularities ware noted in 8(16%) patients which points towards future use of free diced cartilage in those cases where dorsal irregularities are expected or noticed in intra operative period (Figures 3-8).


Conclusion
Subtotal extracorporeal septoplasty can be done by more surgeons with improved cosmetic results in selected patients. Data reveals rates of complications are comparable with endonasal techniques and select patients have better cosmetic outcome.
References
- Aaronson NL, Vining EM (2014) Correction of the deviated septum: from ancient Egypt to the endoscopic era. Int Forum Allergy Rhinol 4(11): 931-936.
- Bhattacharyya N (2010) Ambulatory sinus and nasal surgery in the United States: demographics and perioperative outcomes. Laryngoscope 120(3): 635-638.
- King ED, Ashley FL (1952) The correction of the internally and externally deviated nose. Plast Reconstr Surg 10(2): 116-120.
- Gubisch W, Constantinescu MA (1999) Refinements in extracorporal septoplasty. Plast Reconstr Surg 104(4): 1131-1142.
- Senyuva C, Yu¨cel A, Aydin Y, Okur I, Gu¨zel Z (1997) Extracorporeal septoplasty combined with open rhinoplasty. Aesthet Plast Surg 21(4): 233-239.
- King ED, Ashley FL (1946) The correction of the internally and externally deviated nose. Plast Reconstr Surg 10(2): 116-120.
- Virendra Ghaisas, Sapna Ramkrishna Parab (2015) Role of Extracorporeal Septoplasty in Deviated Noses. Indian J Otolaryngol Head Neck Surg 67(3): 205-209.





























