Extensive Temporal Bone Rhabdomyosarcoma in A Child with Epidural Invasion and Sigmoid Sinus Thrombosis
Hamida Ardhaoui*, S Halily, R Abada, S Rouadi, M Roubal and M Mahtar
Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University Hospital, Morocco
Submission: January 21, 2019; Published: January 28, 2019
*Corresponding author: Hamida Ardhaoui, Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University Hospital, Morocco
How to cite this article: Hamida A, S Halily, R Abada, S Rouadi, M Roubal, M Mahtar. Extensive Temporal Bone Rhabdomyosarcoma in A Child with Epidural Invasion and Sigmoid Sinus Thrombosis. Glob J Oto, 2019; 19(2): 556009. DOI: 10.19080/GJO.2019.19.556009
Abstract
We report a case of temporal bone embryonal rhabdomyosarcomea presenting as infectious mastoiditis in a four years old boy. The tumor first responded to multimodality chemotherapy then evolution had a turning point with epidural invasion of the cervical and dorso-lumbar spine.
Introduction
Rhabdomyosarcoma (RMS) is the most common soft tissue sarcoma in children and represents a high-grade neoplasm of skeletal myoblast-like cells [1]. About 90% of all RMS presentations are in individuals under 25 years of age, and almost 70% are in children under 10 years of age. The most common RMS location is in the head and neck region (35-40%), followed by the urogenital system, extremities, and torso [2]. Although this tumor arises primarily in the head and neck, origin in the mastoid region is particularly rare and may be easily misdiagnosed as an infectious mastoiditis [3].
Case Report

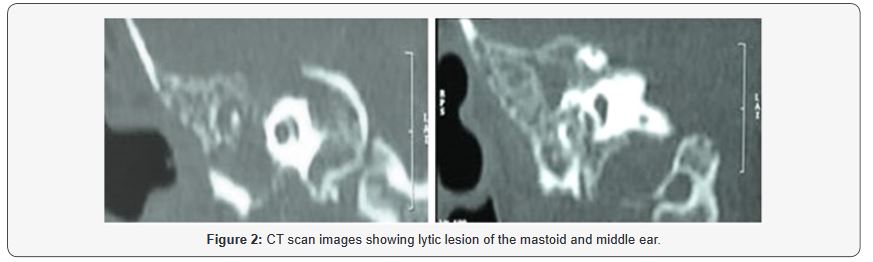
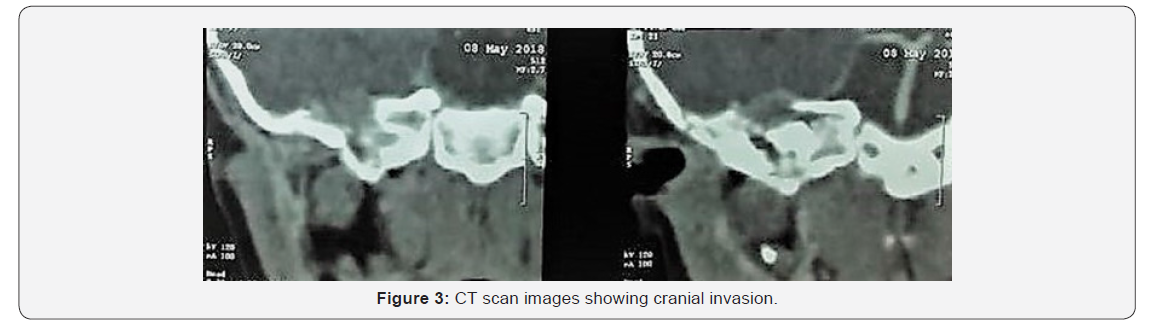
We describe a unique case of a rhabdomyosarcoma of the right temporal bone in a four-year-old boy, presenting with a six weeks history of right otalgia and otorhrea complicated two weeks later with facial palsy. A polyp mass was observed protruding through the external auditory canal (Figure 1). On physical examination, there was a stage 2 (House-Brackmann score) facial paralysis associated with right oculomotor palsy. Otherwise, his pupils were equal and reactive, visual acuity was intact, and he had no nystagmus. The rest of cranial nerve examination was normal. The patient was afebrile and hi neck was supple without lymphadenopathy. CT scan showed a lesion of tissue density of the middle and outer ear measuring 56 x 30 mm. This mass extends to the temporal lobe, the tent of the cerebellum, and the right ponto-cerebellar angle. It invades the cavernous and sigmoid sinus which is thrombosed, encompasses the internal carotid with lysis of the clivus and the great wing of the sphenoid (Figure 2). It also extends to the pre and retrostylian spaces, the para-pharyngeal space, the nasopharynx, the eustachian tube and the right choana. Lastly, on chest CT, there is a right Fowler nodule measuring 7.5 x 6 mm. Biopsy of the mass of the external auditory canal revealed an embryonic rhabdomyosarcoma. Patient was classified high risk as surgery was not possible giving the extensity of the tumor. Multidrug chemotherapy was administered using IVADo regimen (ifosfamide, vincristine, actinomycin D and doxorubicin). The evolution was marked six months later by the appearance of a flaccid motor deficit of the four limbs rapidly progressive in a context of apyrexia. Control CT showed the disappearance of the ear and cerebral mass with the appearance of cervical and dorsolumbar epiduritis (Figure 3). The cytological study of the cerebrospinal fluid confirmed the secondary invasion. The patient succumbed a few days after.
Discussion
RMSs that arise in the temporal bone are rare, accounting for 5 % of malignant tumors of the temporal bone. Horn and Enter line classified the histological variants of RMS as embryonal, botryoid, alveolar and pleomorphic types. Approximately 60% of all newly diagnosed rhabdomyosarcomas are of the embryonal type [4]. Histopathological examination and immunohistochemistry studies including Desmin, musclespecific actin (MSA), Myogenin, MyoD1, and striated muscle actin are the gold standard tests for diagnosis of RMS [5]. In a 2018 review by Thao N. and al. The most commonly reported symptoms at presentation were the presence of a mass in the mastoid area (86.0%) and cranial nerve dysfunction (83.7%). Interestingly, 18.6% of patients received antibiotics at presentation for a presumed infection. They suggest that patients with symptoms atypical of infectious mastoiditis, such as a mass over the mastoid and/or cranial nerve dysfunction, and those who lack the typical symptoms of mastoiditis, such as fever, swelling, or pain, should undergo biopsy with microbiological and/or pathological analysis of specimens in addition to detailed imaging [3]. Despite the multimodality therapy, rhabdomyosarcomas of the middle ear and mastoid, which are close to the meninges and related to the risk of intracranial spread, have a poorer prognosis than those located elsewhere in the head and neck [6]. The Oberlin criteria for stage IV RMS, which is a predictor of overall survival (OS), give 1 point for each of the following: age <1or >10 years, presence of bone or bone marrow metastases, >3 sites of DMS, and unfavorable primary site location. A score of <2 is associated with a more favorable prognosis [7].
The Intergroup Rhabdomyosarcoma Study Group (IRSG) conducted four clinical trials aiming to define the optimal therapy for children and adolescents with middle ear RMS. The group reviewed 179 patients with middle ear RMS and noted in their phase IV pilot study improvements in survival through dose intensification of alkylating agents along with radiation therapy [8]. In our case, the patient was treated using the IVADo regimen which proved in a pilot study by the European Pediatric Soft Tissue Sarcoma Study Group to be effective against pediatric soft tissue sarcoma with acceptable toxicity [9]. As for local control, complete resection of primary tumor is desirable if it can be achieved with minimal morbidity and negative microscopic margins. When up-front resection would result in significant morbidity, biopsy alone is recommended. Adjuvant radiotherapy is recommended for all patients except those with completely resected (margin-negative) RMS [8]. Surgery was not performed in this case because of the impossibility of complete resection of the tumor and infiltration of dangerous anatomical structures. In his review, Rudzinski et al. [10] found that the 5-year event free survival for embryonal RMS is 43% (95% CI 29–56%) [11]. whereas, in another review paper overall survival for high-risk group is approximately 30% and has not improved over the last 25 years [12].
Conclusion
This case emphasizes the importance of investigating patients with non-resolving ear infections, polyps or cranial nerve dysfunction. Additionally, it highlights the spread of rhabdomyosarcoma through cerebrospinal fluid pathways after intracranial extension thereby making cranio-spinal screening important. Besides, diffuse leptomeningeal spread is poorly controlled by chemotherapy and usually bears a poor prognosis.
References
- Skapek SX, Ferrari A, Gupta AA, Lupo PJ, Butler E, et al. (2019) Rhabdomyosarcoma. Nat Rev Dis Primers 5(1): 2.
- Ireneusz Dziuba, Paweł Kurzawa, Michał Dopierała, Larque AB, Januszkiewicz- Lewandowska D (2018) Rhabdomyosarcoma in children - curr ent pathologic and molecular classification Pol J Pathol 69(1): 20-32.
- Thao N Do, Amy M Linabery, Richard J Patterson, Albert Tu (2018) Cranial Rhabdomyosarcoma Masquerading as Infectious Mastoiditis: Case Report and Literature Review. Pediatr Neurosurg 53(5): 317-321.
- Rafiqahmed Vasiwala, Ismail Burud, Siew Kheong Lum, Rajveer Singh Saren (2015) Embryonal rhabdomyosarcoma of the middle ear presenting with aural polyp and facial nerve palsy. Med J Malaysia 70(5): 314-315.
- Xinxin Zhang, Kun Ma, Jaling Wang, Wenming Wu, Lin Ma, et al. (2014) A Prospective Evaluation of the Combined Helical Tomotherapy and Chemotherapy in Pediatric Patients with Unresectable Rhabdomyosarcoma of the Temporal Bone. Cell Biochem Biophys 70(1): 103-108.
- Jinwei Hu, Shunli Liu, Jianhua Qiu (2002) Embryonal rhabdomyosarcoma of the middle ear. Otolaryngol Head Neck Surg 126(6): 690-692.
- Mohan AC, Venkatramani R, Okcu MF, Nuchtern JG, Vasudevan SA, et al. (2018) Local therapy to distant metastatic sites in stage IV rhabdomyosarcoma. Pediatr Blood Cancer 65(2).
- DS Hawkins, JR Anderson, CN Paidas, Wharam, Qualman SJ, et al. (2001) Improved outcome for patients with middle ear rhabdomyosarcoma: a children’s oncology group study, J Clinic Oncol 19(12): 3073-3079.
- Borinstein SC, Steppan D, Hayashi M, Loeb DM, Isakoff MS, et al. (2018) Consensus and Controversies Regarding the Treatment of Rhabdomyosarcoma. Pediatr Blood Cancer 65(2): e26809.
- Rudzinski ER, Anderson JR, Chi YY, Gastier Foster JM, Astbury C, et al. (2017) Histology, fusion status, and outcome in metastatic rhabdomyosarcoma: A report from the Children’s Oncology Group. Pediatr Blood Cancer 64(12): e26645.
- Cianni Bisogno, Andrea Ferrari, Christophe Bergeron, Scagnellato A, Prete A, et al. (2005) The IVADo regimen-A pilot study with ifosfamide, vincristine, actinomycin D, and doxorubicin in children with metastatic soft tissue sarcoma study group. Cancer 103(8): 1719-1724.
- Hajime Hosoi (2016) Current status of treatment for pediatric rhabdomyosarcoma in the USA and Japan Pediatrics International 58(2): 81-87.





























