Mandibular Metastasis Revealing a Clear Cell Renal Cell Carcinoma
H Ardhaoui*, S Halily, R Abada, S Rouadi, M Roubal and M Mahtar
Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University Hospital, Morocco
Submission: January 16, 2019; Published: January 22, 2019
*Corresponding author: H Ardhaoui, Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University Hospital, Morocco
How to cite this article: H Ardhaoui, S Halily, R Abada, S Rouadi, M Roubal, M Mahtar. Mandibular Metastasis Revealing a Clear Cell Renal Cell Carcinoma. Glob J Oto, 2019; 19(2): 556006. DOI: 10.19080/GJO.2019.19.556006
Abstract
Introduction: Renal clear cell carcinoma (RCC) has different manifestations, including uncommon metastasis and paraneoplastic syndromes. It is the most frequent kidney neoplasm, and the third most frequent neoplasm to metastasize to the head and neck region.
Case presentation: A Forty-five years old woman presented at our ENT department with a mandibular swelling associated with hematuria. Mandibular mass biopsy showed a metastatic location of clear cell renal cell carcinoma. CT scans showed an extensive right renal tumor, which has infiltrated the liver with a peritoneal carcinosis. After multidisciplinary team discussion, the consensus reached was that the patient had a very advanced metastatic renal cell carcinoma.
Discussion: Renal carcinoma is the third most common neoplasm that metastasizes to the oral cavity. It accounts for nearly 3% of all adult malignancies and is the most lethal urologic cancer. The focus in metastatic renal cell carcinoma treatment has increased the last two decades, mainly due to the progress of targeted therapies. Metastasectomy remains debatable as an option which might lead to a complete and durable regression. Clear cell renal cell carcinoma has a very poor long term prognosis, such as most patients die in one year after detection of metastasis.
Keywords: Renal Cell Carcinoma; Mandibular Metastasis
Introduction
Renal cell carcinoma (RCC) is the most frequent kidney neoplasm, with a high tendency to metastasize. It is the third most frequent neoplasm to metastasize to the head and neck region. It is the urological tumor with the highest mortality rate despite the increase in initial diagnoses from the widespread use of ultrasonography and CT due to the high rate of metastasis at the time of diagnosis. RCC has different manifestations, including metastasis in uncommon sites and paraneoplastic syndromes.
Case Presentation
A Forty-five years old woman presented at our ENT department with a four months history of painful swelling of her right hemi-mandible. The swelling made mastication difficult and resulted in occasional oral bleeding.

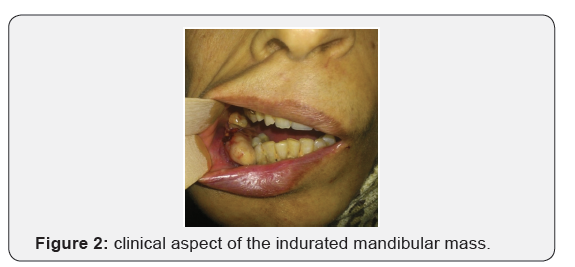
The patient also had an eight months history of hematuria and four episodes of urinary tract infection during the same period, which resolved with antibiotics prescribed by her primary care physician. She also lost fifteen kilograms during the last four months. Clinical examination revealed a 5 x 4 cm indurated mass occupying most of the Para symphyseal region of the right mandible with contact bleeding, and without infiltrating the buccal floor (Figures 1 & 2). There were no palpable cervical lymph nodes. An indurated, painful mass was also noticed in the right lumbar region with a diffuse tenderness of the abdominal wall. Abdominal ultrasound showed a peritoneal carcinosis due to solid –cystic mass, which has destroyed the right kidney and infiltrated the liver. Panoramic radiography showed an irregular opacity in the right Para symphyseal region, with moth-eaten appearance, suggestive of a malignant process. A mandibular mass biopsy was performed, and pathology confirmed a metastatic location of clear cell renal cell carcinoma. Abdominal and chest CT scan showed an extensive right renal tumor, infiltrating the liver with peritoneal carcinosis and several lung nodules. After multidisciplinary team discussion, the consensus reached was that since the patient had a very advanced metastatic renal cell carcinoma; no therapeutic plan was suggested. She was transferred to the palliative care unit and succumbed shortly after.
Discussion
The incidence of oral metastatic tumors is very low, accounting for approximately 1% of all malignant oral tumors. However, some sporadic cases have been reported in the literature. Renal carcinoma is the third most common neoplasm that metastasizes to the oral cavity, following lung and breast carcinoma. It accounts for nearly 3% of all adult malignancies and is the most lethal urologic cancer. Approximately onethird of patients present with metastatic disease and 40% to 50% will develop distant metastases (asynchronous metastatic disease) after the initial diagnosis [1]. RCC has various signs and symptoms, which makes it one of the most challenging diagnoses. Spread in RCC might be lymphatic, hematogenous or by direct invasion. This is why metastasis may occur in any site of the body [2]. In order of frequency, metastatic RCC affects paranasal sinuses, larynx, jaw, temporal bone, thyroid gland, and parotid gland [3]. Clear cell renal cell carcinoma (CCRCC) is a subtype of renal cell carcinoma typically characterized by malignant epithelial cells with clear cytoplasm. Clear cell tumors of the oral mucosa, jaws, and salivary glands constitute a heterogeneous group of lesions. They may originate from salivary gland, odontogenic tissue, or be metastatic. Metastatic tumors that may present in the mandible with clear cell features include the breast (33%), lung (18%), kidney (16%), thyroid (6%), prostate (6%) and colon (6%) [2].
Histologically, there is a big resemblance between the CCRCC and odontogenic carcinoma. Very frequently, pathologists encounter clear cells in many malignant neoplasms; their origin can’t be determined on the basis of conventional histopathology, making it a very challenging diagnosis. Immunohistochemical staining seems very helpful, showing a focal cytokeratin positivity and a strong reaction for Vimentin exhibited by RCC metastasis [4]. CCRCC has a very poor long term prognosis, such as most patients die in one year after detection of metastasis, which explains the important role of palliative therapies in order to, improve comfort and reduce morbidity. Surgical resection (total or partial nephrectomy) is the best treatment for localized primary tumors in patients with stage I through stage IV disease, but surgical outcome is strongly dependent on stage and grade of the disease. The rate of postoperative metastatic recurrence is 59% by 12 months, 83% by 24 months, and 93% by 36 months in metastatic RCC patients with larger renal or lymph node- positive tumors [5]. Radical nephrectomy combined with immunotherapy is proven to be the best option to significantly increase survival in patients with metastatic RCC compared to immunotherapy alone [6]. However, in patients with unresectable tumors or metastatic RCC, it might have limited clinical benefit. These patients, and those with recurrent disease following therapy, are candidates for additional chemotherapy.
The focus in metastatic renal cell carcinoma treatment has increased the last two decades, mainly due to the progress of targeted therapies. Metastasectomy remains debatable as an option which might lead to a complete and durable regression, at least for a minority of patients. Even if there is not a high level of evidence supporting its efficiency over time, this approach has obtained wide consensus both due to the fact that in some cases it increases survival and clinical regression of the disease, and because of the lack of more effective therapeutic alternatives [7]. In our case, the patient presented a large RCC metastasing to the liver, lungs and mandible. Multidisciplinary team discussion concluded that mandibular metastasis excision was not beneficial, and only palliative care could be provided.
Conclusion
This case illustrates the importance of considering unusual presentations of RCC which is the third most common neoplasm to metastasize to the head and neck region. Metastatic RCC should be included as a differential diagnosis for all oral and neck lesions for patients with history of RCC. Even if CCRCC has a very poor long term prognosis, palliative therapies are very important in order to improve patient’s quality of life and reduce morbidity.
References
- Will TA, Agarwal N, Petruzzelli GJ (2008) Oral cavity metastasis of renal cell carcinoma: a case report. Journal of medical case reports 2: 313.
- Ahmadnia H, Amirmajdi NM, Mansourian E (2013) Renal cell carcinoma presenting as mandibular metastasis. Saudi journal of kidney diseases and transplantation: an official publication of the Saudi Center for Organ Transplantation, Saudi Arabia 24(4): 789-92.
- Torres-Carranza E, Garcia-Perla A, Infante-Cossio P, Belmonte-Caro R, Loizaga-Iriondo JM, et al. (2006) Airway obstruction due to metastatic renal cell carcinoma to the tongue. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics 101(3): e76-78.
- Jain A, Shetty DC, Juneja S, Narwal N (2016) Molecular Characterization of Clear Cell Lesions of Head and Neck. Journal of clinical and diagnostic research: JCDR 10(5): Ze18-23.
- Saidi JA, Newhouse JH, Sawczuk IS (1998) Radiologic follow-up of patients with T1-3 a,b,c or T4N+M0 renal cell carcinoma after radical nephrectomy. Urology 52(6): 1000-1003.
- Flanigan RC, Salmon SE, Blumenstein BA, Bearman SI, Roy V, et al. (2001) Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med 345(23): 1655-1659.
- Antonelli A, Arrighi N, Corti S, Legramanti S, Zanotelli T, et al. (2012) Surgical treatment of atypical metastasis from renal cell carcinoma (RCC). BJU international 110(11 Pt B): E559-63.





























