Radio-Clinical Correlation in the Management of Patients Dizzying: Proposal of a Diagnostic Attitude
F Alloun1*, Y Malki2, A Matari3, H Ainouche4 and D Djennaoui5
1Service Otorhinolaryngology, CNEMPN, Algeria
1Service radiologie, HCA, Algeria
2Service épidémiologie, CRMC, Algeria
3Service ORL, CHU Mustapha, Algeria
Submission: January 02, 2019; Published: January 18, 2019
*Corresponding author: F Alloun, Service Otorhinolaryngology, CNEMPN, Algeria
How to cite this article: F Alloun, Y Malki, A Matari, H Ainouche, D Djennaoui. Radio-Clinical Correlation in the Management of Patients Dizzying: Proposal of a Diagnostic Attitude. Glob J Oto, 2019; 19(1): 556005. DOI: 10.19080/GJO.2019.19.556005
Abstract
Introduction: Diagnostic management of vertigo has attracted the interest of several authors around the world, given the errors and diagnostic impasses found. The main objective of our work is to analyze the contribution of a well-established clinical diagnostic protocol compared to that of imaging in the etiological diagnosis of vertigo whether acute or chronic, and this in order to justify indications of imagery in front of a vertigo.
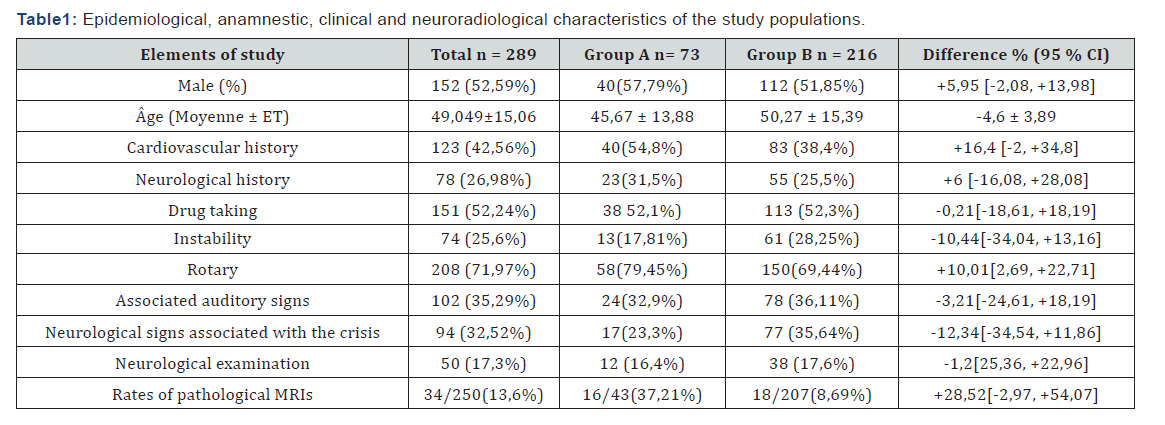
Materials and methods: It is a multicenter prospective clinical trial of a detailed and documented diagnostic protocol. The study populations are divided into two groups:
i. Group “A” with a number equal to 73 patients, benefiting from a detailed and documented clinical protocol.
ii. Group “B” with a number equal to 216 patients with imaging preceded by a succinical clinical examination.
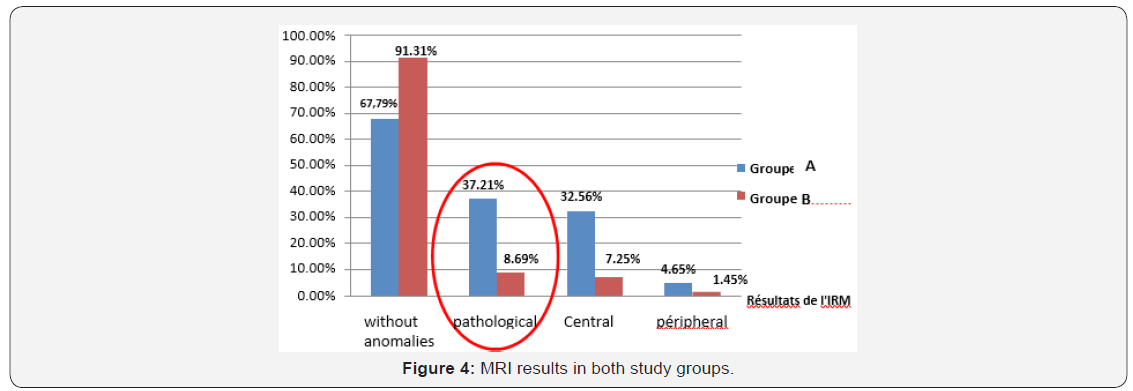
Results: The positive magnetic resonance imaging rate was four times higher in group “A”; 16 out of 43 MRIs made (37.2% of the MRIs requested were pathological) compared to the “B” group; 18 out of 207 made MRI (8.69% of pathological imaging in all requested MRI). The results of the factors predictive of a central MRI lesion are quite interesting.
Conclusion: The final interest is twofold: to have a diagnostic consensus and an impact on the health economy by reducing the systematic imaging practice in front of a case of vertigo.
Keywords: Central Vestibular Involvement; Examination; Vertigo; Videonystagmoscopy
Introduction
Vertigo is a frequent reason for consultation and, according to different authors, represents 2 to 3% of admissions. Of these, more than 15% have a pejorative etiological diagnosis [1]. Data from the recent literature concerning the management of vertigo diagnosis converge towards misuse of radiological investigations [2]. Vannuci et al preliminarily evaluated the diagnostic performance of a structured algorithm: STANDING (Spontaneous Nystagmus, Direction, head impulse test, standing) to differentiate central acute vertigo (AV) and peripheral acute vertigo [3]. The main objective of our work is to analyze the contribution of a well-established clinical diagnostic protocol compared to that of imaging in the etiological diagnosis of vertigo whether acute or chronic, and this in order to propose a diagnostic attitude and therefore, justify the indications of imaging in front of vertigo.
Materials and Methods
This is a multi-center prospective prospective clinical trial of a detailed and documented, three-year (2015- 2018) diagnostic protocol. This study involved 289 patients with true vertigo. Recruited patients were separated into two groups:
a. The group of patients with a detailed clinical protocol and documented “group A” (n = 73) including a detailed interview on 53 items, the study of oculomotricity, high frequency tests using videonystagmoscopy with video recording, a neurological and general examination as well as caloric tests. Imaging was requested only based on the results of the above examinations.
b. The group of patients with imaging preceded by a succinct clinical examination “group B” (n = 216). The data was collected on a pre-established form. The data capture and exploitation were carried out with the EPI info version 6.04 software for bivariate analyzes and possibly the SPSS or Epidata software for multivariate analyzes.
Results
The research, in the group “A” of a spontaneous and provoked nystagmus by the videonystagmoscopy, objectified the following results:
i. Spontaneous nystagmus was found in 5 patients (6.85%).
ii. The Dix and Hallpike test were positive in 29/73 patients (39.73%).
iii. The head shaking test (HST) revealed horizontal nystagmus in 25 patients (34.25%), including patients with spontaneous nystagmus who all had pathological HST.
iv. The head impulse test (HIT) revealed catch-up saccades in 11 patients (15.07%), always including patients with spontaneous nystagmus.
v. Gaze nystagmus was positive in 15 cases representing 20.54% of patients (Figure 1).
In the “A” group, 16 MRIs representing 37.21% of the MRIs made, objected to anomalies, divided into:



a. 2 MRI with peripheral involvement: a case of meningeal enhancement in the left ponto-cerebellar angle involving the acoustico-facial bundle (Figure 2), a case of vascularnervous conflict between the anterior inferior cerebellar artery (AICA) and the left vestibulo-cochlear nerve.
b. 14 MRIs with central lesions distributed as follows: 05 cases of multiple sclerosis, 03 cases of Arnold Chiari malformations (Figure 3), one case of ischemic lesion of the territory of the left posterior inferior cerebellar artery (PICA) causing a cerebellar ischemic stroke, a case of arachnoid cyst
In the “B” group, only 18 MRIs representing 8.69% of MRI scans, showed abnormalities (Figure 4). Our analytical study of the different clinical parameters and their possible correlations with a central attack on MRI made the following observations:
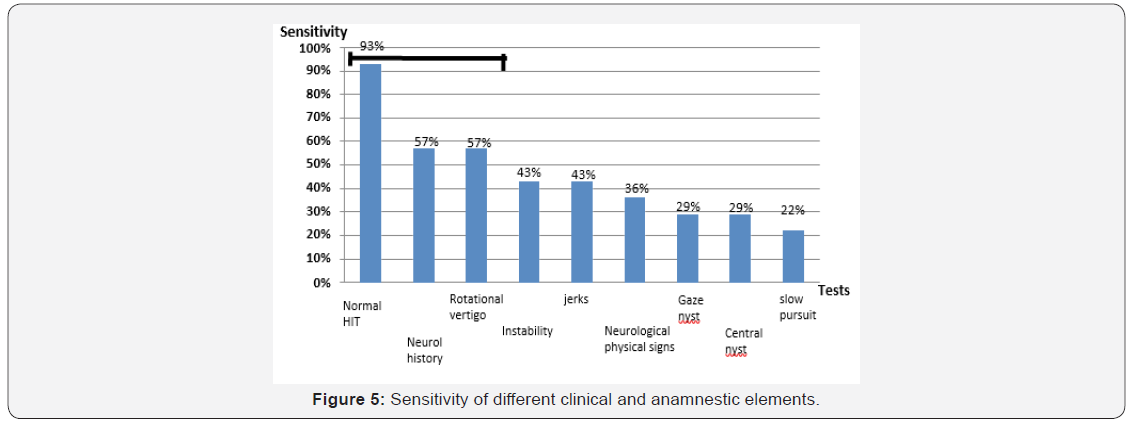
i. The most sensitive test is the normality of the HIT cephalic pulse test with sensitivity reaching 93% contrasting with low specificity (33%) (Figure 5)
ii. The most specific test is the slow continuation during oculomotricity examination with a specificity of 90% contrasting with low sensitivity (22%) (Figure 6).

Discussion
Age
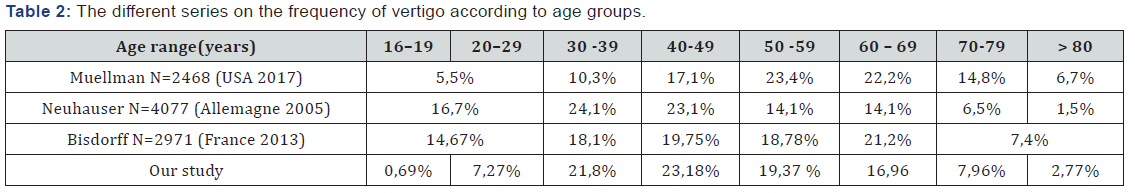
The aging of the population seems to be an important factor. Neuhauser et al (Germany 2006), on a larger population (n = 4077), show the same frequency peaks as ours [4]. Muellman (USA 2017), when he finds, rather peaks in the age group 50-69 years,which is also valid in the study of Bisdorff [5,6] (Table 2).
Etiology
Peripheral vestibular involvement was the most common cause of vertigo in most series (Table 3).

Predictive Factors
The rate of MRI positive four times higher in group “A” compared to group “B” motivated our choice of population “A” as a study model looking for clinical factors pejorative of an attack at the imagery, peripheral is so or especially central. Our study demonstrated a significant statistical relationship between the presence of neurological antecedents and central MRI (P = 0.03), consistent with literature data. Park et al, examining the records of patients with central vertigo, found that most patients (81%) complained of a neurological history of headache [7]. In our series (group A), 57% of central MRI lesions had a history of neurological symptoms. Our results are similar to those of Enass S. Mohamed who, on a series of 21 MRIs with central involvement, found 51.61% of neurological symptoms [8]. The symptom instability was found in 75% of central radiological findings by MRI in the study of H Amar [9]. He reported a statistically significant relationship (p = 0.002) between the instability symptom and the central MRI lesion, in contrast to the rotary-type vertigo (p = 0.844). The presence of oculomotricity saccades seems to have a better sensitivity and less specificity of a central MRI lesion compared to the slow continuation, sensitivity increasing from 43 to 22% and specificity from 86 to 90 %, approaching the results of the Ennas study [8] Won Gue Han [10] through a retrospective study, analyzed a series of 31 patients with vertigo of which he suspected the central origin and in whom a cerebral MRI was made. Among this series of 31 patients, 15 had perverted central nystagmus (14 had lower vertical nystagmus, and one case of superior vertical nystagmus). Among these 15 patients, 5 patients had a pathological MRI pathological, thus finding a sensitivity of 34%, close to that of our work where there is objectified at 29% [10].
Regarding the gauze nystagmus, among the few studies, that of Ennas (Egypt 2015), did not show a significant statistical relationship between gauze nystagmus and central MRI (p = 0.526). Our results concerning the head impulse test (HIT) were the most relevant. 91% of the MRI without central involvement had a pathological HIT and 93% of the MRI with central impairment had a normal HIT. DENewman Toker reported that 91% of central vascular lesions on MRI had a normal HIT (retained canal function), which is similar to our findings despite the fact that vascular lesions on MRI represented only 7% of all the central attacks of our series [11]. In his small series, Mc Dowell found that 100% of central lesions on MRI had a normal HIT [12].
According to Kattah and Toker [11] the HINTS acronym used by the Anglosaxon (Head-Impulse- Nystagmus-Test-of-Skew) representing the association: Normal cephalic pulse test (HIT), nystagmus changing direction, vertical misalignment of the ocular axes, appears to be more sensitive than MRI for acute stroke within 24 to 48 hours after onset of symptoms [13]. Vannucci et al [3] still in the emergency, tested the performance of an algorithm in 98 patients called STANDING (Spontaneous Nystagmus, Direction, head impulse test, standing) looking for a central spontaneous nystagmus, its direction, a normal cephalic pulse test (HIT) and / or an inability to stand up, to differentiate the central causes from the peripheral causes. The test had a very high sensitivity at 100% and a specificity of 94.3% for central vestibular involvement. However, still in our study, HINT or STANDING triads were not decisive in the diagnosis of a central MRI lesion, because contrary to the studies mentioned above, our work was interested in all vertigo whether acute or chronic. This allows us to suggest a triad of tests, low sensitivity certe for some of them but of good specificity, whose association would present an aid in the diagnosis of a central attack on MRI.
We immediately notice:
a. Except for the normality of the Cephalic Pulse Test (HIT) (93%), the other elements have low sensitivity for central MRI involvement.
b. The specificity for central MRI is quite high for elements such as instability-type vertigo, pathological slow continuation, neurological physical signs
Conclusion
Our study compared to that of the literature has consolidated the role of a careful clinical examination with adequate material (videonystagmoscopy) in the etiological diagnosis of vertigo and being done, decreased indications of imaging Regarding the predictors of a central cause, our results concerning the sensitivity and specificity of some clinical tests for central MRI are quite interesting. We hope to expand our series, to consolidate our results.
References
- Newman Toker DE, Hsieh YH, Camargo CA, Pelletier AJ, Butchy GT, et al. (2008) Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample. Mayo Clin Proc 83(7): 765-775.
- Batuecas Caletrío Á, Yáñez González R, Sánchez Blanco C, González Sánchez E, Benito J, et al. (2014) Peripheral vertigo versus central vertigo. Application of the HINTS protocol. Rev Neurol 59(8): 349-353.
- Vanni S, Pecci R, Casati C, Moroni F, Risso M, et al. (2014) Standing, a four-step bedside algorithm for differential diagnosis of acute vertigo in the emergency department. Acta Otorhinolaryngol Ital 34(6): 419- 426.
- Neuhauser HK, von Brevern M, Radtke A et al. (2005) Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology 65(6): 898-904.
- Muelleman T, Shew M, Subbarayan R, Shum A, Sykes K, et al. (2017) Epidemiology of Dizzy Patient Population in a Neurotology Clinic and Predictors of Peripheral Etiology. Otol Neurotol 38(6): 870-875.
- A Bisdorff, G Bosser, R Gueguen and P Perrin (2013) The epidemiology of vertigo, dizziness, and unsteadiness and its links to co-morbidities. Front Neurol 4: 29.
- MK Park, KM Kim, N Lee, HH Jung, SW Chae, et al. (2014) The usefulness of magnetic resonance imaging for acute isolated vertigo patients in the emergency department. Int Adv Otol 10(2): 162-166.
- Enass S Mohamed (2016) Predictors of central vestibular disorders from videonystagmography tests. The Egyptian Journal of Otolaryngology 32(3): 202-209.
- H Ammar, R Govindu, R Fouda, W Zohdy, E Supsupin, et al. (2017) Dizziness in a community hospital: central neurological causes, clinical predictors, and diagnostic yield and cost of neuroimaging studies. J Community Hosp Intern Med Perspect 7(2): 73-78.
- Won Gue Han, Hee Chul Yoon, Tae Min Kim, Yoon Chan Rah, June Choi, et al. (2016) Clinical correlation between perverted nystagmus and brain MRI abnormal findings. J Audiol Otol 20(2): 85-89.
- Newman Toker DE, Kattah JC, Alvernia JE, et al. (2008) Normal head impulse test differentiates acute cerebellar strokes from vestibular neuritis. Neurology 70: 2378-2385.
- McDowell T, Moore F (2016) The under-utilization of the head impulse test in the emergency department. Can J Neurol Sci 43(3): 398-401.
- Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman Toker (2009) HINTS to diagnose stroke in the acute vestibular syndrome. Threestep bedside oculomotor examination more sensitive than early MRI diffusion- weighted imaging. Stroke 40(11): 3504-3510.





























