Langerhans Cell Histiocytosis: manifestation in both Mastoid Cavities
Ardhaoui H*, Halily S, Abada R, Rouadi S, Roubal M and Mahtar M
Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University Hospital, Morocco
Submission:December 19, 2018; Published: January 11, 2019
*Corresponding author: Ardhaoui H, Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University Hospital, Morocco
How to cite this article: Ardhaoui H, Halily S, Abada R, Rouadi S, Roubal M, et all. Langerhans Cell Histiocytosis: manifestation in both Mastoid Cavities. Glob J Oto, 2019; 19(1): 556001. DOI: 10.19080/GJO.2019.19.556001
Abstract
IntroductionLangerhans’ cell histiocytosis (LCH) is a rare pathology, which may affect several organs with a variety of clinical presentations and prognosis. Temporal bone location is not rare but often misdiagnosed.
Case presentationAn 18 months female child was admitted to our ENT department with a two months history of left otorrhea, resistant to antibiotics, associated with episodes of right otalgia. Clinical examination found an inflammatory polyp in the left external auditory canal and an inflammatory tympanic membrane in the right ear. Temporal bone computed tomography identified a soft tissue density process occupying the whole mastoid cavity with diffusely destructive lytic lesions in both ears. Cortical mastoidectomy was performed for diagnostic purposes. Histopathologic examination of the tissue revealed Langerhans cell histiocytosis (LCH).
DiscussionLangerhans’ cell histiocytosis (LCH) represent a group of heterogeneous diseases which results from the clonal proliferation of Langerhans cells. The etiopathogenesis is still unclear. Diagnosis of temporal LCH is based on pathology examination and immunohistochemical findings. Treatment options for temporal bone LCH include surgery, radiotherapy, chemotherapy and steroid injections. The most relevant prognostic factors in LCH are age at presentation, multisystemic involvement and vital organ dysfunction.
Keywords: Langerhans’ Cell Histiocytosis; Temporal Bone; Mastoid Cavity
Introduction
Langerhans cell histiocytosis (LCH) is a group of chronic heterogeneous diseases, which may affect several organs with a variety of clinical presentations and prognosis. The pathogenesis is an abnormal polyclonal proliferation of Langerhans cells causing local or systemic effects. Otologic involvement can be seen in 15% to 61% of the patient [1]. This condition is more frequent in children and may range from a solitary to multifocal lesions. It might be either asymptomatic or revealed by numerous symptoms such as pain, swelling, pathological fractures in the site of involvement. When the disease is revealed by ontological symptoms with no other clinical findings, diagnostic errors might be frequent because of the similarity with other conditions, particularly mastoiditis. The most relevant prognostic factors are represented by age at presentation, multisystem involvement and vital organ dysfunction [2].
Case Presentation
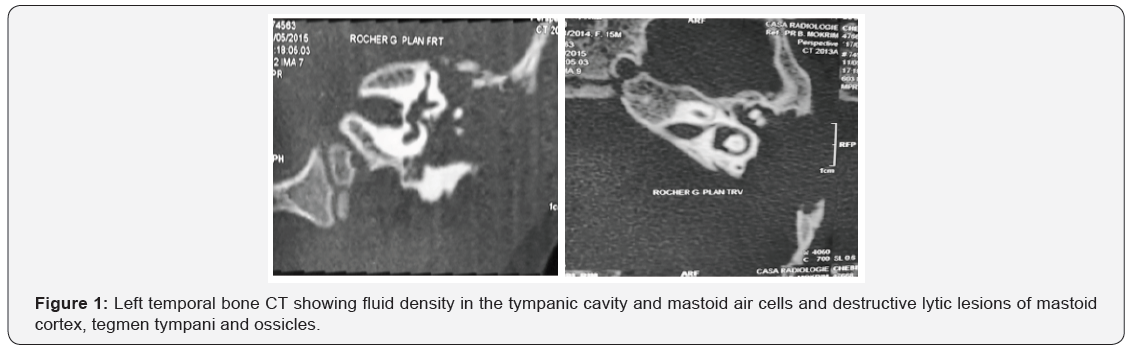
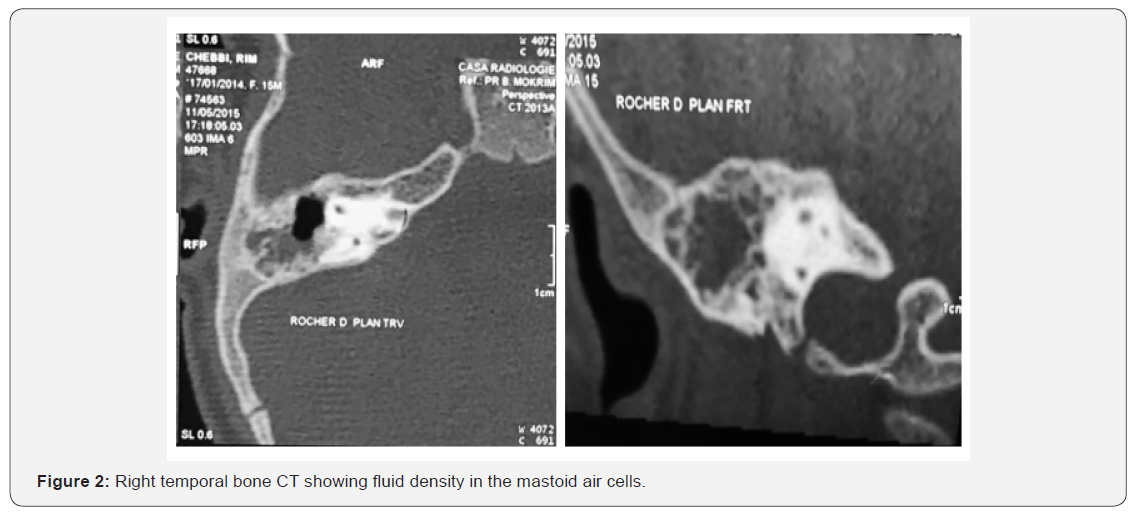
An 18 months child was admitted to our ENT department with a two months history of left otorrhea resistant to antibiotics, associated with episodes of otalgia in the right ear. The previous medical history was generally unremarkable. Clinical examination found an inflammatory polyp of the left external auditory canal and an inflammatory tympanic membrane in the right ear. There was no facial paralysis or cervical lymphadenopathies. The rest of the clinical examination was normal. Temporal bone computed tomography identified a soft tissue density process occupying the whole mastoid cavity with diffusely destructive lytic lesions of mastoid cortex, tegmen tympani and ossicles in both ears more importantly in the left side. The intracranial structures were normal (Figures1,2). The patient was diagnosed with bilateral mastoitidis. An empiric systemic antibiotics and local ear drops were started. In the absence of clinical improvement after ten days of treatment, a left mastoidectomy was performed, for diagnostic purposes. Surgical exploration revealed a yellow tissue mass occupying the whole mastoid cavity. Histopathologic examination of this tissue concluded to LCH. Blood tests (full blood count, biochemistry, monoclonal gammopathy screening, erythrocyte sedimentation rate, C reactive protein), chest computed tomography, abdominal ultrasound, bone marrow aspiration biopsy, plain X-ray graphs of the long bones, were performed in order to seek a systemic involvement, and the results were negative. The patient was then transferred to the haematology department where chemotherapy was started. Nine months after the procedure, temporal bone computed tomography did not show evidence of recurrence and the two years follow up was clear.
Discussion
Langerhans’ cell histiocytosis represent a group of heterogeneous diseases which results from the clonal proliferation of Langerhans cells. The etiopathogenesis is still unclear. It is a rare entity with a male predominance. The incidence is around 5.4 per million with a peak among children aged between 1 and 4 years, but it can affect patients of any age [3]. Many authors have discussed the existence of immune, genetic or viral predisposing factors, but no conclusive proof has been determined. Clinical manifestation varies among patients and there is no pathognomonic feature. The involvement of the external and middle ear is not rare but often misdiagnosed because of the similarity of the otologic findings with those of other conditions such as mastoiditis, chronic otitis media, recurrent otitis externa or otitis media, stenosis and, less commonly, peri auricular or middle ear masses, and cholesteatoma [4]. In a study on patients diagnosed with temporal bone LCH, Saliba and al. reported that the clinical manifestations of temporal bone LCH was highly variable. The most common presentation was a temporal bone mass (70%), followed by otitis media and externa (60%). However, external auditory canal polyp, conductive hearing loss, headaches, and otalgia were less common [2]. Frequent upper respiratory infections (URTI) and enlarged cervical lymph nodes might be associated. Cervical lymph nodes might be affected either in a single, isolated organ disease or as part of a systemic disease.
There is no specific radiological finding for LCH. Computed tomography is considered the most accurate way to describe the lesions and their extent in the temporal bone. It is also a useful tool for monitoring disease activity and response to treatment. Generally lytic lesions diffusely destructive with indistinct margins are seen. It also demonstrates the typical ‘‘punched-out’’ radiolucent defects that distinguish them from other lytic lesions of the temporal bone such as cholesteatoma, solitary bone cyst, surgical defects, or chronic infections [5]. Final diagnosis of temporal LCH is based on pathology examination. Reactive infiltration of eosinophils granulocytes and immature Langerhans cells with abundant vacuolated cytoplasm, and vesicular oval nuclei can be seen. The diagnosis can also be made on the immunohistochemical findings. Detection of surface antigen protein S-100 and/or leucocytes adhesion molecules CD1 antigens, which is now used more often since it is a cost-efficient test [6]. There are several treatment options for temporal bone LCH, including surgery, radiotherapy, chemotherapy and steroid injections. They are used in different combinations or a single modality depending on the extent and severity of the disease [7]. Many authors agreed that the best therapeutic option is surgical removal when possible. In multifocal disease, inaccessible lesions to local treatment and when radiotherapy is not recommended, chemotherapy seems to be the best treatment. Many protocols exist and the duration of treatment varies according to the severity of lesions. Howarth et al. reported a spontaneous recovery in 3 of 188 cases with osseous LCH. The most relevant prognostic factors in LCH are age at presentation, multisystemic involvement and vital organ dysfunction. Many authors have reported a good prognosis in LCH affecting the temporal bone with a survival rate of over 90% in limited organ involvement and 65 to100% in multifocal disease [8].
Conclusion
Conclusion
References
- Fernandez Latorre F, Menor Serrano F, Alonso Charterina S, Arenas Jimenez J (2000) Langerhans’ cell histiocytosis of the temporal bone in pediatric patients: imaging and follow-up. AJR American journal of roentgenology 174(1): 217-221.
- Saliba I, Sidani K, El Fata F, Arcand P, Quintal MC, et al. (2008) Langerhans cell histiocytosis of the temporal bone in children. International journal of pediatric otorhinolaryngology 72(6): 775-786.
- Martini A, Aimoni C, Trevisani M, Marangoni P (2000) Langerhans cell histiocytosis: report of a case with temporal localization. International journal of pediatric otorhinolaryngology 55(1): 51-56.
- Azouz EM, Saigal G, Rodriguez MM, Podda A (2005) Langerhans’ cell histiocytosis: pathology, imaging and treatment of skeletal involvement. Pediatr Radiol 35(2): 103-115.
- Marioni G, De Filippis C, Stramare R, Carli M, Staffieri A (2001) Langerhans’ cell histiocytosis: temporal bone involvement. The Journal of laryngology and otology 115(10): 839-841.
- Lallemant B, Fayoux P, Nelken B, Leroy X, Vaneecloo FM (2003) [Management of head and neck Langerhan’s cell histiocytosis in children]. Annales d’oto laryngologie et de chirurgie cervico faciale : bulletin de la Societe d’oto-laryngologie des hopitaux de Paris 120(1): 30-39.
- Gulam I, Pegan B, Stancic V, Kruslin B (2001) Langerhans’ cell granulomatosis in an adult: a 22-year follow up. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery 258(4): 203-207.
- Mosnier I, Rondini Gilli E, Crosara PT, Belmatoug N, Cyna Gorse F, et al. (2004) Langerhans’ cell histiocytosis of the labyrinth in adults. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 25(1): 27-32.





























