Juvenile Hyaline Fibromatosis with Facial Involvement Rare Case Report
Waleed M Alshehri*1, Khalid Murrad2, Muath Hakami2, Mohamed Amir Mrad2 and Manea K Alanezi1
1 Department of Otolaryngology, King Faisal Specialist Hospital, Riyadh, Saudi Arabia
2 Department of Plastic Surgery, Saudi Arabia
Submission: August 31, 2018; Published: September 07, 2018
*Corresponding author: Waleed M Alshehri, Department of Otolaryngology, King Faisal Specialist Hospital, Riyadh, Saudi Arabia.
How to cite this article: Waleed M A, Khalid M, Muath H, Md Amir M, Manea K A. Juvenile Hyaline Fibromatosis with Facial Involvement Rare Case Report. Glob J Oto, 2018; 17(3): 555965. DOI: 10.19080/GJO.2018.17.555965
Abstract
Juvenile hyaline fibromatosis and infantile systemic hyalinosis are rare conditions of unknown origin characterized by delayed growth, gingival hypertrophy, papular skin lesions, and joint deformity. In this article, we describe the rare case of a patient with upper gingival hyperplasia who was referred to the plastic surgery for consultation and surgical intervention. The patient was treated surgically and histopathologic findings was consistent with the characteristics of juvenile hyaline fibromatosis.
Introduction
Hyalinosis (ISH) is an inherited autosomal recessive disorder that affects the connective tissue. Juvenile hyaline fibromatosis (JHF) equally affects both sexes and is commonly diagnosed during early childhood; however, fewer cases are reported in adult life [1,2]. The first case of JHF was diagnosed in 1873 and was named molloscum fibrosum by Murray [3]. Later, in 1972, the condition was renamed JHF by Kitano et al. [4]. The main clinical features of infantile systemic ISH included diffusely thickened, inflexible skin, papular skin lesions, hyperpigmentation over the metacarpophalangeal joints of the hands and malleoli, gingival hyperplasia, perianal nodules, limitations of joint motility, osteoporosis of bones, bone fractures, short stature, persistent diarrhea, and failure to thrive [5-7]. JHF is characterized by hypertrophy of the gingiva; joint deformity; flexion contractures; the presence of bone lesions, osteopenia, and hyaline material deposition in the extracellular spaces of the dermis and soft tissues; and stunted growth [2,8,9], with researchers identifying impaired collagen synthesis as underpinning the development of JHF [10]. Two forms of the disease exist: a localized form with very slow growth and a diffuse form with rapidly growing, large tumors [11].
Case Presentation
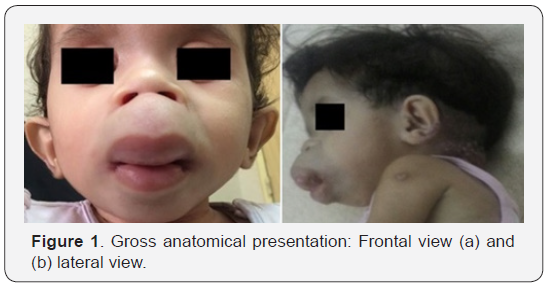
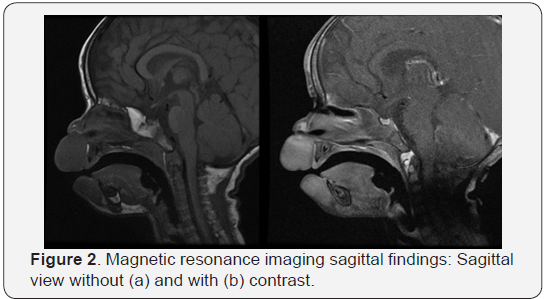
A 2-year-old girl presented to the outpatient clinic due to her failure to thrive, which was first document at an age of 11 months. The girl was conceived in a first-degree consanguineous marriage. The course of pregnancy was normal and her birth weight was 3200g. She was exclusively breast fed and refused all other formula or food. She exhibited delayed growth and development, was only able to sit, and could only say two words: “DA” and “MA.” Upon examination, her weight and height were below the third percentile for age, while her head circumference was in the 5th percentile for her age. The patient had dysmorphic features, including epicanthal folds and skin nodules in the upper lip with gingival hyperplasia (Figure 1) as well as mild bed sores affecting her back and buttocks with perianal erythematous nodules. There were no audible cardiac murmurs and organomegaly was detected. Stiffness contracture was observed on both the upper and lower limbs with a flexion deformity affecting both knee joints. Her hip joints were in an abduction position and were not dislocated. Skeletal survey revealed generalized osteopenia, dysplasia in both structures, and symmetrical erosions in the medial aspect of the proximal metaphysis of both tibias. Results of basic hematologic and biochemical investigations were normal except for hypothyroidism. Her bone profile revealed normal calcium and phosphorus levels. Magnetic resonance imaging revealed a soft tissue mass that involved her upper lip measuring 21×36×26mm (anteroposterior × transverse × craniocaudally, respectively) in size. It exhibited an intermediate signal on T2 and a low signal on T1 imaging with homogeneous enhancement with contrast. A similar, but smaller, mass was observed to be involved with her lower lip. It measured approximately 16×22× 22mm in size (Figures 2 & 3). The underlying bone was intact with no erosive changes. Bilateral intra-articular lesions were observed within the temporomandibular joints with a high signal on T2 and a low signal on T1 imaging, with enhancement with contrast. The lesion on the right and left sides measured approximately 11× 16mm and 6×12 mm (anteroposterior × transverse), respectively. The patient underwent debulking of tissue under general anesthesia and was discharged one week later in a good condition (Figure 4). Histopathological examination of the excised nodule at the upper lip revealed an abundance of homogeneous, amorphous, eosinophilic extracellular matrix that contained spindle-shaped cells. Histo chemically, the homogeneous matrix of the lesion area was PAS-positive, while the Congo red stain was negative. Based on testing for the ANTXR2 gene and histopathological findings, a diagnosis of JHF was made.

Discussion
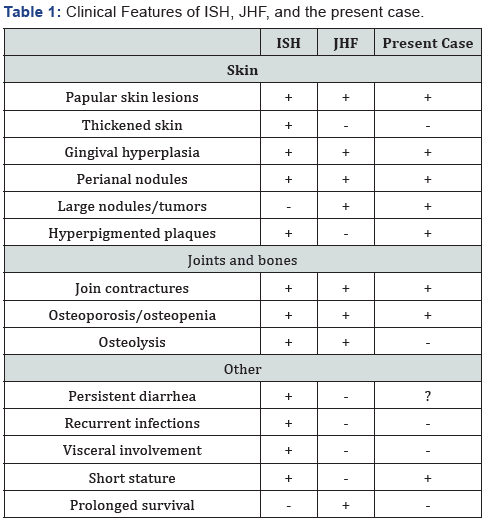
Juvenile hyaline fibromatosis is a rare familial disease characterized by abnormal hyalinized fibrous tissue growth that mainly affects the soft tissues in the head and neck [12]. JHF is more common among infants produced in a consanguineous marriage, with no predilection for any particular race or sex. Most cases generally exhibit normal mental development [13]. However, there are some reports of patients who are diagnosed at an older age, sometimes in the fourth or fifth decade of life [14]. The main clinical features of both ISH and JHF include papular and nodular skin lesions, gingival hyperplasia, joint contractures, and a variable degree of bone involvement (Table 1) [13]. No reported case of malignant transformation of JHF has yet been reported. The findings in the patient described herein are consistent with a mild form of the disease. In older children, gingival hyperplasia may cover part of the occlusal surfaces of the teeth, causing chewing problems [15]. Meanwhile, joint contractures are the primary cause of morbidity among patients with the condition. Progressive flexion contractures limit movement and may lead to individuals becoming wheelchair dependent in early adulthood. Big cutaneous lesions may result in the development of ulcerations and repeated infections or pain. It has been postulated that JHF may be a collagen metabolism disorder since abnormalities in collagen types III and VI have been reported in some patients. However, there are no consistent defects in collagen, and many affected persons exhibit normal collagen structure upon histological analysis [16]. In JHF, histopathological confirmation is used to definitively diagnose the patient. The course and severity of the disease differ across patients, with most patients surviving up until the fourth decade of life [17]. Different treatment modalities for JHF exist, but mainly focus on surgical excision of the lesion. Functional and cosmetic improvements are targeted by surgical approaches, such as in the presented case. Meanwhile, intralesional injections of steroids and proteolytic enzymes are also used for treatment, but are stymied by a high recurrence rate [18]. In conclusion, both conditions require a multidisciplinary approach, including surgical intervention, to restore function, enhance appearance, and help regain a sufficiently good quality of life.
Conflicts of Interest
The authors declare no potential conflict of interests with respect to the research, authorship, and/or publication of this article.
References
- Larralde M, Munoz SA, Calb I, Magariños C (2001) Juvenile hyaline fibromatosis. Pediatr Dermatol 18(5): 400-402.
- Altug HA, Gunal A, Günhan O, Sençimen M (2009) Juvenile hyaline fibromatosis of the mandible with bone involvement: Report of a rare case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108(5): 59-63.
- Murray J (1873) On three peculiar cases of Molluscum Fibrosum in Children in which one or more of the following conditions were observed: hypertrophy of the gums, enlargement of the ends of the fingers and toes, numerous connective-tissue tumours on the scalp, &c. Med Chir Trans 56: 235-254.
- Kitano Y, Horiki M, Aoki T (1972) Two cases of juvenile hyaline fibromatosis: some histological, electron origin, microscopic, and tissue culture observations. Arch Dermatol 106: 877-883.
- Landing BH, Nadorra R (1986) Infantile systemic hyalinosis: report of four cases of a disease, fatal in infancy, apparently different from juvenile systemic hyalinosis. Pediatr Pathol 6(1): 55-79.
- Glover MT, Lake BD, Atherton DJ (1991) Infantile systemic hyalinosis: Newly recognized disorder of collagen? Pediatrics 87: 228-234.
- Glover MT, Lake BD, Atherton DJ (1992) Clinical, histologic, and ultrastructural findings in two cases of infantile systemic hyalinosis. Pediatr Dermatol 9(3): 255-258.
- Hatamochi A, Sasaki T, Kawaguchi T, Suzuki H, Yamazaki S (2007) A novel point mutation in the gene encoding capillary morphogenesis protein 2 in a Japanese patient with juvenile hyaline fibromatosis. Br J Dermatol 157(5): 1037-1039.
- Uslu H, Bal N, Guzeldemir E, Pektas ZO (2007) Three siblings with juvenile hyaline fibromatosis. J Oral Pathol Med 36(2): 123-125.
- Lubec B, Steinbert I, Breier F, Jurecka W, Pillwein K, et al. (1995) Skin collagen defects in a patient with juvenile hyaline fibromatosis. Arch Dis Child 73(3): 246-248.
- De Rosa G, Tornillo L, Orabona P, D’Antonio A, Staibano S, et al. (1994) Juvenile hyaline fibromatosis: A case report of a localized form? Am J Dermatopathol 16(6): 624-627.
- Finlay AY, Ferguson SD, Holt PJA (1983) Juvenile hyaline fibromatosis. Br J Dermato 108(5): 609-616.
- Mancini GM, Stojanov L, Willemsen R, Kleijer WJ, Huijmans JG, et al. (1999) Juvenile hyaline fibromatosis: Clinical heterogeneity in three patients. Dermatol 198(1): 18-25.
- Goldblum JR, Weiss SW, Folpe AL (2014) Enzinger and Weiss’s soft tissue tumors. (6th edn.), Elsevier Saunders, Philadelphia, Pennsylvania.
- Çam B, Kurkcu M, Ozturan S, Haytac C, Uguz A, et al. (2015) Juvenile hyaline fibromatosis: a case report follow up after 3 years and a review of the literature. Int J Dermatol 54(2): 217-221.
- Kayashima KI, Katagiri K, Shinkai H (1994) Is juvenile hyaline fibromatosis a disease of type VI collagenosis?. In: Ishibashi Y, Nakagawa H, Suzuki H (Eds.). Electron microscopy in dermatology: basic and clinical research. Elsevier Science, Amsterdam, Netherlands, pp. 329.
- Gilaberte Y, Mediero GI, Barrantes VL, Zambrano A (1993) Juvenile hyaline fibromatosis with skull-encephalic anomalies: A case report and review of the literature. Dermatology 187: 144-148.
- Rega AN, De Sanctis N, Caracciolo G, Capobianco A, Monaco R, et al. (1998) Juvenile hyaline fibromatosis: A case report. J Pediatr Orthop B 7(3): 235-238.





























