Epistaxis: What Do People Know And What Do They Do?
Ahmed H Saleem*1, Abdullah M Alahwal2, Ahmed A Al Sayed3, Manal I Bin Mani and Hani Z Marzouki4
1Department of Otolaryngology-Head and Neck Surgery, King Fahad Medical City and Research Center, Saudi Arabia
2Faculty of Medicine, King Abdulaziz University, Saudi Arabia
3Division of Otolaryngology - Head and Neck Surgery, Department of Surgery, Dalhousie University, Canada
4Faculty of Medicine, King Saud University, Saudi Arabia
5Department of Otolaryngology-Head and Neck Surgery, Faculty of Medicine, King Abdulaziz University, Saudi Arabia
Submission: January 15, 2018; Published: January 29, 2018
*Corresponding author: Ahmed Hussain S Saleem, Scholar at King Fahad Medical City, Riyadh, Saudi Arabia; P.O. Box: 56 Madinah, Saudi Arabia, 41411, Tel: +966502532000; Email: Ahmed.hs.saleem@gmail.com
How to cite this article: Ahmed H S, Abdullah M A, Ahmed A A S, Manal I B M, et al. Epistaxis: What Do People Know And What Do They Do?. Glob J Oto 2018; 13(2): 555857. DOI: 10.19080/GJO.2018.13.555857
Abstract
Aim: To assess the current knowledge of the first aid management of epistaxis and misconceptions among the general Saudi population.
Methods: A survey questionnaire was developed and was distributed via text message, email, social networks, various websites, and web forums among the Saudi population. Responses were collected over a period of 2 months. Knowledge was assessed based on correct responses to 6 main questions. Five to 6 correct answers was considered excellent knowledge, 3 - 4 as good knowledge, and 2 and below as poor knowledge.
Results: There were 1,760 individuals who responded to the survey, 577 (32.8%) were males. There were 828 respondents (47.0%) who received information on the first aid management of epistaxis, the most common source of information was through a relative or a friend (15.7%). Only 199 respondents (11.3%) will apply pressure to control epistaxis, 99 (5.6%) knows where to correctly press, and 84 (4.78%) will correctly tilt the head forward. There were 132 respondents (7.5%) who thought that patients should be brought to the ER in all cases of epistaxis. There were 1,111 respondents (63.2%) who have poor knowledge of first aid management of epistaxis.
Conclusion: There is poor knowledge of the first aid management of epistaxis in the surveyed Saudi population. Increased awareness and information dissemination programs on the first aid management of epistaxis can improve knowledge and recall among the general population.
Keywords: Epistaxis; General population; Knowledge; First aid; Saudi
Introduction
Epistaxis commonly referred to as "nosebleed" remains to be one of the most common ENT emergencies presenting to the Accident & Emergency Departments (AED) worldwide. In the United States, around 1.7% of all AED visits are due to epistaxis, and about 1 in 200 ED visits in the US is due to epistaxis. (1) The incidence usually is bimodal affecting mostly those younger and the older population (less than 10 years old and more than 70 years old) [1]. Epistaxis that occurs in children younger than 10 years usually is mild and originates in the anterior nose, whereas epistaxis that occurs in individuals older than 50 years is more likely to be severe and to originate posteriorly [2]. However, the incidence of epistaxis declines in adulthood, but approximately one-half of all adults with epistaxis had nosebleeds during childhood [3].
A multitude of causes of epistaxis in children has been reported from nose picking and idiopathic causes, to trauma, medications, nasopharyngeal mass, bacterial nasal colonization, and allergic rhinitis and to the less common cause such as ectopic intranasal tooth [4-10]. In adults, recurrent epistaxis is found to be related to trauma, bleeding disorders and neoplasia apart from the causes mentioned above similar to children [11]. Some studies tried to find association or a cause and effect between epistaxis and hypertension, but were not successful [12,13]. Treatment of epistaxis has undergone significant changes over the years from the uncomfortable posterior nasal pack to the newly developed packing devices, indigenous hemostatic agents and endoscopic surgical approaches [14].
In most of the cases, epistaxis usually occurs in an out-of- the-hospital setting. Thus it is very important for non- health professional people to understand and know some first aid measures for epistaxis. Unfortunately, these people have a very poor knowledge of first aid measures for epistaxis [15]. A survey conducted among 500 members of the public on how they would deal with a nosebleed revealed that only 50 of 443 responses (11.3%) have the knowledge on how to deal with epistaxis [16]. Other studies also showed very poor knowledge of the first aid treatment of epistaxis not only in the public but also among health professionals [16]. In one survey among health professionals, the commonest first aid measures for epistaxis was pinching the nose (94%), nasal packing (80.6%) and sitting leaning forward position (76.1%), and only 38.1% of respondents demonstrated the correct site for pinching the nose [17]. In the modern digital age, people usually use the internet as sources of information particularly YouTube, however studies showed that many videos on how to manage epistaxis were found to proffer inappropriate and dangerous "alternative" advice.
There were very few and recent studies that investigated on how lay people deal with epistaxis when it occurs to them or their family and relatives. For this reason, we conducted this study to assess the current knowledge of the first aid management of epistaxis and misconceptions among the general Saudi population.
Method
We conducted a descriptive study using a survey questionnaire that was developed to address the objectives of the study. The survey tool consisted of questions regarding the demographic profile of the respondents (age, gender, nationality, educational level, and place of residency) and questions on knowledge and sources of information about epistaxis. Identifiers such as name address and contact numbers of respondents were not asked to ensure confidentiality and protection of the respondents.
The survey tool was setup online using the surveymonkey. com (San Mateo, CA, USA) and was piloted on 10 respondents for clarity, errors, and technical issues before distribution. The actual survey was done by distributing the link to the survey monkey through text message, email, social networks, various websites, and web forums among the Saudi population along with the consent for participation in the survey/study. Responses were collected over a period of 2 months from September to October 2016. Data collected after the 2 months collection period were downloaded from the survey site as Microsoft Excel 2013 worksheet and was checked for completeness of data.
Assessment of knowledge of first aid management of epistaxis
Correct responses on six (6) questions regarding the first aid management of epistaxis including applying pressure on the nose, correct area of the nose where to apply pressure, duration of applying pressure, tilting the head, and packing and use of ice packs to control bleeding. Correct responses were given 1 point, and the sum of all responses was obtained. Five to 6 correct answers of 6 questions was considered excellent knowledge, 3 - 4 as good knowledge, and 2 and below as poor knowledge.
Statistical analysis was performed using the IBM Statistical Package for the Social Sciences Software (SPSS) version 23.0 (SPSS Inc., Chicago, IL, USA). Data is presented as numbers, means and percentages. Chi-square test (x2) was used for statistical significance between categorical variables and independent t-test for continuous variables. Factors that are correlated with knowledge of the first aid management of epistaxis was done using the chi-square test and the Pearson correlation test. A p-value of ≤0.05 was considered statistically significant. The study complied with all institutional ethical requirements and was approved by the Institutional Review Board of the College of Medicine, King Saud University, Riyadh, Saudi Arabia.
Results
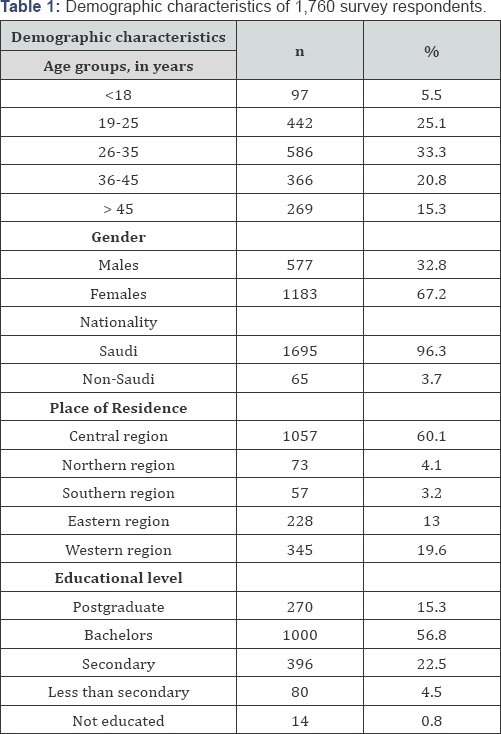
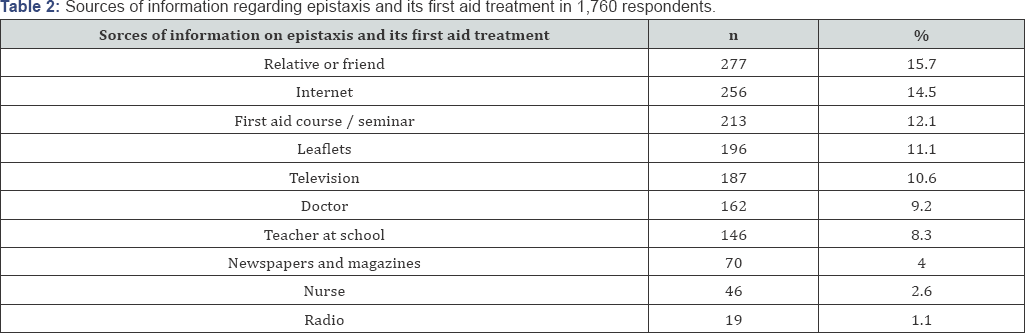
There were 1,760 individuals who responded to the survey, 577 (32.8%) were males and 1183 (67.2%) were females. Saudis constituted 96.3% of the respondents. There were 586 respondents (33.3%) who were aged 26-35 years old, and 442 respondents (25.1%) were aged 19 - 25 years old. There were 1000 respondents (56.8%) who had a Bachelor's degree in college, and only 14 (0.8%) were not educated. There were 1057 respondents (60.1%) from the Central region. Table 1 shows the detailed demographic profile of the respondents. There were 828 respondents who claimed that they received information on the first aid management of epistaxis. The most common sources of information include a relative or friend (15.7%), internet (14.5%), first aid course (12.1%), leaflets (11.1%) and television (10.6%) (Table 2).
Respondents who had a previous encounter with somebody who had epistaxis
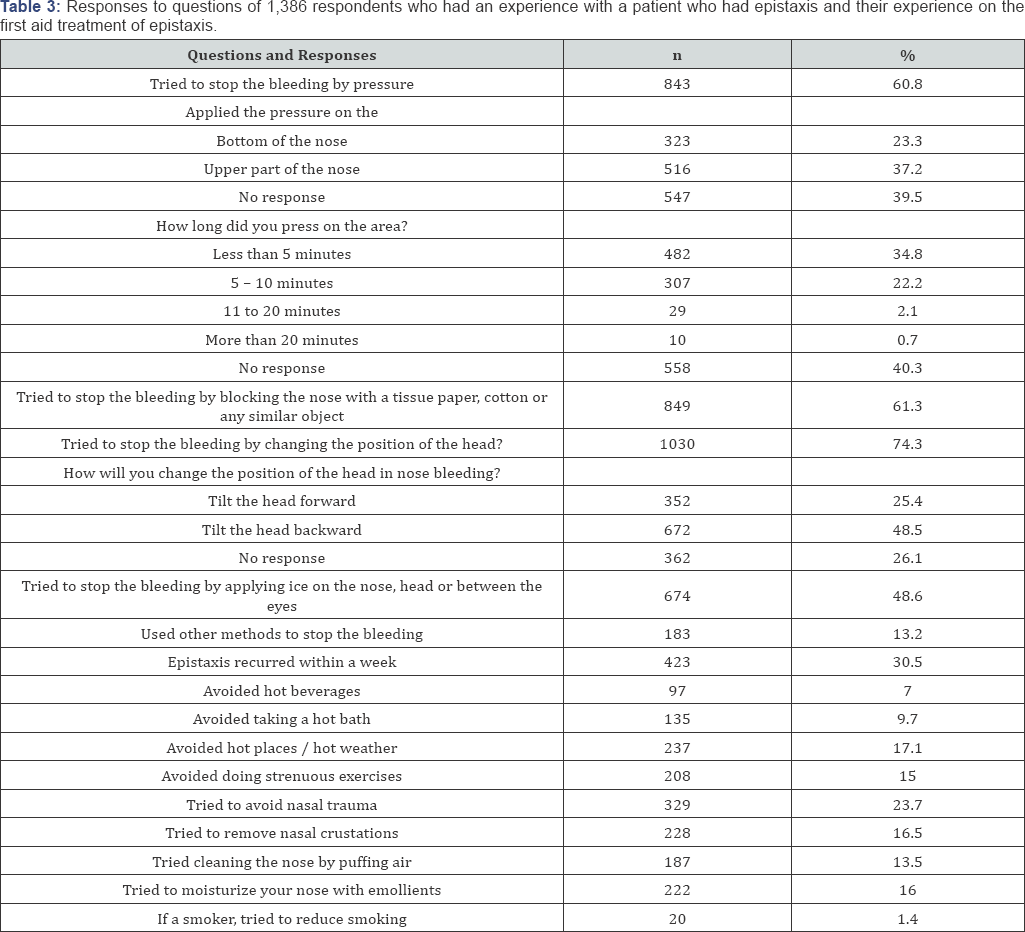
There were 1,386 respondents (78.8%) who have known somebody who had epistaxis. Of these respondents, 683 (49.3%) had received information on first aid management of epistaxis. Of the 1,386 respondents who claimed they have known somebody or have witnessed somebody who had epistaxis, 843 (60.8%) tried to stop the bleeding by applying pressure on the nose, 516 (37.2%) applied the pressure on the upper part of the nose, 482 (34.8%) said that they applied pressure for less than 5 minutes, 29 (2.1%) said that they applied pressure for 11 - 20 minutes, 307 (22.2%) for 5 - 10 minutes and 10 (0.7%) applied pressure for more than 20 minutes. There were 849 respondents (61.3%) who tried to control the bleeding by blocking the nose with a tissue paper, cotton or any similar object. There were 1,030 respondents (74.3%) who tried to stop the bleeding by changing the patient's head position, 672 (48.5%) of which by tilting the head backwards. There were 674 respondents (48.6%) who tried to stop the bleeding by applying ice on the nose, head or between the eyes. There were 423 respondents (30.5%) who claimed that the bleeding (epistaxis) recurred within a week (Table 3).
There were 97 respondents (7.0%) who claimed that they avoided hot beverages, 135 respondents (9.7%) avoided taking a hot bath, 237 (17.1%) avoided hot places, 208 (15.0%) avoided doing strenuous exercises, 329 (23.9%) avoided any trauma to the nose, 228 (16.5%) avoided removing nasal crustations, and 187 (13.5%) avoided cleaning the nose by puffing air. There were 222 respondents (16.0%) who tried to moisturize their nose with emollients, and 20 (1.4%) tried reducing smoking.
Responses to questions when asked what they will do if they will experience or will have epistaxis themselves?
When all respondents were asked if in case they will have epistaxis, will they stop it or control it by pressure?, Only 199 respondents (11.3%) said they will stop the bleeding and will control the pressure. One-hundred six respondents said they will pressing on the top of the nose, whereas 93 respondents (5.3%) said they will press at the bottom of the nose. There were 99 respondents (5.6%) who claimed that they will press the nose for less than 5 minutes, and 93 (5.3%) for 5 - 10 minutes. Furthermore, there were 216 respondents (12.3%) who said that they will stop the bleeding by blocking the nose with a tissue paper, cotton or any similar object, 268 (15.2%) will try to control the bleeding by changing the head position (184 backwards and 84 forward), 197 (11.2%) will control the bleeding by placing ice on the nose, head or between the eyes, and 45 (2.6%) will try using other methods (Table 4).

Among the things that the respondents thought to exacerbate epistaxis include the following; drinking hot beverages (1.5%), hot baths (3.9%), exposure to hot places and hot weather (8.3%), strenuous exercises (8.9%), sneezing (3.8%), and smoking (4.3%). There were 121 respondents (6.9%) who thought that moisturizing the nose reduces the risk for epistaxis. There were 132 respondents (7.5%) who thought that patients should be brought to the ER in all cases of epistaxis irregardless of the duration of nosebleed, whereas 741 (42.1%) thought that patients should be brought to the ER when epistaxis lasts more than 20 minutes. Around 428 (24.3%) of respondents thought that one-quarter cup of blood constitute a heavy bleeding.
When respondents were asked about which platform would best serve to increase awareness of epistaxis, and which of the platform would reach them more effectively, 1,020 respondents (58.0%) said social media such as facebook and twitter, 915 (52.0%) through first aid seminars and conferences, followed by teachers (n=819, 46.5%) and television (n=780, 44.3%). Table 4 shows the responses of all the respondents on what are their measures and first aid treatment when they will have epistaxis themselves.
Knowledge of the first aid management of epistaxis
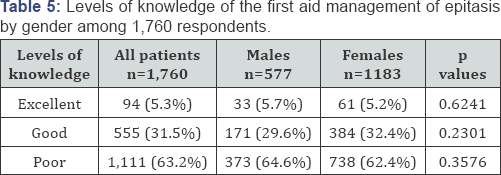
Of the 1,760 respondents, there were only 94 (5.3%) who scored excellent in knowledge of first aid management of epistaxis. There were 555 respondents (31.5%) who had good knowledge, and 1,111 respondents (63.2%) had poor knowledge of first aid management of epistaxis. The gender distribution of levels of knowledge of the first aid management of epistaxis is shown in Table 5. Knowledge is significantly correlated to "received information on first aid management of epistaxis" (r=0.126, p<0.001) and "knew someone managed of epistaxis" (r=0.342, p<0.001). Age, gender, nationality, place of residence and educational level are not correlated to knowledge of first aid management of epistaxis (p=0.069, p=0.787, p=0.444, p=0.653 and p=0.095 respectively). Logistic regression analysis of significant factors that affect the knowledge of the first aid management of epistaxis revealed "having received information on the first aid management of epistaxis" and "having known someone with epistaxis" as the most significant factors (beta = 0.101; t=4.459; p<0.001, and beta = 0.336; t=14.982, p<0.001 respectively).
Discussion
To our knowledge, this is the first study that investigated on the knowledge and misconceptions on the first aid management of epistaxis in Saudi Arabia. Our study confirms that the general public of Saudi Arabia has poor knowledge on the first aid management of epistaxis. Our results showed that 63.2% of the surveyed population had poor knowledge on the first aid management of epistaxis. Our results fared better compared to a similar study conducted by Strachan and England in 1997, in which they found that 88.7% of their surveyed population has poor knowledge on the first aid management of epistaxis. 15 However, the Strachan's study 15 was conducted among patients who were attending the ENT department; our study was conducted on the general population particularly on patients who were not attending any ENT consultation during the time of the survey, which would reflect a more valid result on the surveyed population, i.e. the general public. Another possible explanation for this is the significant advancement in technology and telecommunication methods and the easy access to information nowadays through the Internet and the different social media.
Another highlight of this study is that 828 respondents (47.0%) have received information on the first aid management of epistaxis, and around 78.8% have known somebody who had epistaxis. However, there were 475 respondents (57.4%) who still have poor knowledge of the first aid management of epistaxis and were able to answer 1 or 2 questions correctly indicating poor recall of any information about epistaxis or probably even misinformation about the first aid management of epistaxis. Many of these respondents (n=286, 30.9%) got their information on epistaxis through the internet. With the multitude of websites in the internet that proffer management advises on epistaxis, many of these internet sites may not be very useful and sometimes inappropriate for the management of epistaxis. This has been explained by Mugwe in 2014, wherein several internet sites particularly in YouTube suggests medical advice on how to manage epistaxis, but most of these sites are unreliable and are not evidence based [17]. Furthermore, it was found that recall with these procedures (first aid management of epistaxis) has been found to be very low among health practitioners, what more with ordinary individuals who are not health practitioners? This probably explains why despite the information that our respondents have received, there were still a significant number of respondents who scored poor and very low on the questions regarding management of epistaxis.
Among the respondents who have witnessed somebody with epistaxis, 60.8% claimed that they tried to stop the bleeding by applying pressure. However when they were asked if they (themselves) will have epistaxis, only 11.3% said that they will stop the bleeding by applying pressure. Furthermore, 22.2% of those who witnessed somebody with epistaxis said they applied the pressure correctly for 5-10 minutes. In contrast, only 5.3% will apply pressure on their nose for 5-10 minutes when they (themselves) will have epistaxis. The disparity in the percentages in the responses to questions between what they have observed and what they will do when they (themselves) will have epistaxis holds through with other questions. Percentages of correct responses were lower when they will have epistaxis themselves compared to when they observed what is done to somebody with epistaxis. The explanation is very clear. Respondents do not actually know or much more, not sure whether what they have observed what is being done to somebody who has epistaxis is "correct" or does not know / is not sure of what is the correct approach to management for epistaxis if they will have it themselves.
There were also a few of our respondents who thought that hot beverages, hot bath and hot weather can intensify nosebleeds. The explanation for these changes in humidity and temperature have an effect on the capillaries in the nose, particularly vasodilation which increases blood flow through all capillaries, including the nose, increasing the chance for a bleed, and also the mucous membranes of the nose becomes more sensitive to changes in humidity and weather (also in cold weather, nosebleeds are also very common). Information on these other factors that can increase the likelihood of a nosebleed such as changes in the weather may not be tackled that often during a doctor-patient conversation, and much less often in conversations among friends, relatives who are not health practitioners or even health related workers.
Another highlight of this study is, around 7.5% of our respondents thought that patients should be brought to the ER in all cases regardless of the duration of the nosebleed, and around 42.1% claimed that patients who bleed for more than 20 minutes should be brought to the ER. The knowledge of patients on when to go to the ER and have themselves treated for epistaxis is important because it can save them time and effort of rushing to the hospital when in fact they can simply manage epistaxis through simple and basic steps at home, unless they are the so called "blood thinners" (patients who are taking medicines like warfarin, clopidogrel and/or aspirin). Moreover, an increase in the knowledge of first aid management of epistaxis will greatly reduce the congestion in the ER particularly in cold and hot weather, and eventually save on the economics aspect of health care.
Overall, the general knowledge of our respondents on the first aid management of epistaxis is low, even though some of them claimed to have witnessed how epistaxis was managed. However, having witnessed someone being managed for epistaxis and having received a formal training or information on the first aid management of epistaxis are factors that can significantly improve their level of knowledge. This study showed that the level of education, gender and age may not significantly improve the knowledge of the first aid management of epistaxis. First aid management of epistaxis is more of a procedure that can be done at home. The procedure actually does not need someone to be highly educated, or be young to do it properly. All it needs is proper training and instruction on how to do it properly. Simple rationalization of why we have to press on that particular area of the nose, for how long makes a lot of difference.
The limitation of this study is its descriptive nature. Since we have conducted this study in a survey format, we were not able to assess the authenticity of the responses and not just mere "guesses" made by the respondents. However, being the first study to describe how the lay individuals think, know, and what they do in cases of epistaxis, the results of this study can serve as a background for further studies that can be conducted in this matter. Furthermore, the results of this study reflect how the "ordinary" people who are not medically-inclined perceive and think of epistaxis. For local authorities and administrators of health institutions, the highlights of this study can serve as a basis for implementation of information campaigns, workshops, training and seminars to increase the knowledge of the general population on the first aid management of epistaxis. In the long run, there will be a great ease in the burden of health economics and future planning, and will definitely decrease the morbidity of epistaxis.
Conclusion
There is a high percentage of poor knowledge of the first aid management of epistaxis in the Saudi population. Health care institutions, health administrators together with the health care authorities of the general population should work hand in hand to increase not only awareness and knowledge among those who have received information of epistaxis but also enhance recall and retention of the first aid management of epistaxis. This in turn will decrease the morbidity of epistaxis and will be a very big help to the economic planning and aspects of the health care industry.
References
- Pallin DJ, Chng YM, McKay MP, Emond JA, Pelletier AJ, et al. (2005) Epidemiology of epistaxis in US Emergency Department5s, 1992 to 2001. Ann Emerg Med 46(1): 77-81.
- Bernius M, Perlin D (2006) Pediatric ear, nose, and throat emergencies. Pediatr Clin North Am 53(2): 195.
- Paranjothy S, Fone D, Mann M, Dustan F, Evans E, et al. (2009) The incidence and aetiology of epistaxis in infants: a population-based study. Arch Dis Child 94(6): 421.
- Burton MJ, Doree C (2004) Interventions for recurrent idiopathic epistaxis (nosebleeds) in children. Cochrane Database of Systematic Reviews 1.
- Brown NJ, Berkowitz RG (2004) Epistaxis in healthy children requiring hospital admission. Int J Pediatr Otorhino 68(9): 1181-1184.
- Bilgen C, Karci B, Uluoz U (2002) A nasopharyngeal mass: leech in the nasopharynx. Int J Pediatr Otorhino 64(1): 73-76.
- Whymark AD, Crampsey DP, Fraser L, Moore P, Williams C, et al. (2008) Childhood epistaxis and nasal colonization with Staphylococcus aureus. Otolaryngology Head Neck Surg 138(3): 307-310.
- Schlosser RJ (2009) Epistaxis. N Engl J Med 360: 784-789.
- Douglas R, Wormald PJ (2007) Update on epistaxis. Current Opinion in Otolaryngology & Head & Neck Surgery 15(3): 180-183.
- Verma RK, Bakshi J, Panda N (2012) Ectopic intranasal tooth: an unusual cause of epistaxis in a child. Ear, Nose & Throat Journal 91(6): 242-244.
- Gifford TO, Orlandi RR (2008) Epistaxis. Otolaryngol Clin North Am 41: 525-536.
- Sarhan NA, Algamal AM (2015) Relationship between epistaxis and hypertension: A cause and effect or coincidence? Journal of the Saudi Heart Assoc 27(2): 79-84.
- Lavy JA, Koay CB (1996) First aid treatment of epistaxis - are the patients well informed? J Accid Emerg Med 13(3): 193-195.
- Strachan D, England J (1998) First aid treatment of epistaxis - confirmation of widespread ignorance. Postgrad Med J 74: 113-114.
- Middleton PM (2004) Epistaxis. Emerg Med Aust 16(5-6): 428-440.
- Mugwe P, Kamau KJ, Nyambaka OK (2014) Knowledge, Attitude and Practice in First Aid Management of Epistaxis by Accident and Emergency Clinical Staff at Kenyatta National Hospital. East Cent Afr J Surg 19: 17-21.
- Haymes AT, Harries V (2016) "How to stop a nosebleed": an assessment of the quality of epistaxis treatment advice on You Tube. J Laryngol Otol 130(8): 749-754.





























