Squamous Cell Carcinoma of External Auditory Canal
Gutiérrez Espinosa, César Alfonso1, Cortés Ponce, José Rosmal2*, Ruiz Gudiño, Clara2, Falcón García Juan Manuel2, Navarro Anaya German2
1Department of Otolaryngology and Head and Neck Surgery, Regional Hospital “General Ignacio Zaragoza“, Mexico
2Resident of La Salle University, Department of Otolaryngology and Head and Neck Surgery, Regional Hospital “General Ignacio Zaragoza“, Mexico
Submitted: September 27, 2017; Published: October 12, 2017
*Corresponding author: Jose Rosmal Cortes, Resident of La Salle University, Department of Otolaryngology and Head and Neck Surgery, Regional Hospital "General Ignacio Zaragoza”, Mexico City, Mexico, Mexico
How to cite this article: Gutierrez E, Cesar A, Cortes P, Jose R , Ruiz G, Clara, Falcon G J M, Navarro A, German. Squamous Cell Carcinoma of External Auditory Canal. Glob J Oto 2017; 11(1): 555805. DOI: 10.19080/GJO.2017.11.555805
Abstract
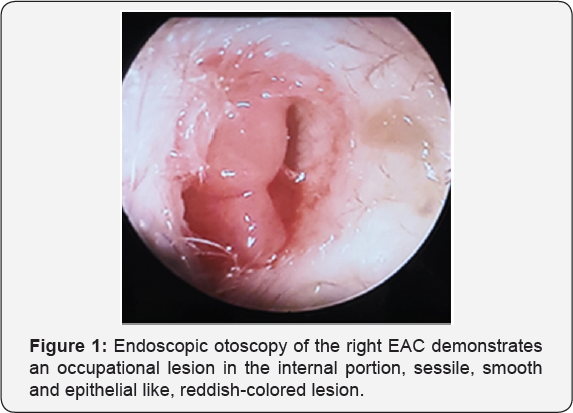
Squamous cell carcinoma of the external auditory canal has a low incidence, with a mean age of presentation of 40-60 years old. The characteristic clinical presentation is an occupational EAC lesion that is accompanied by chronic otalgia, purulent/hematic otorrhea and conductive hearing loss. We reported the case of a 75-years old female patient with one year of intermittent right ear purulent/ hematic otorrhea, and ipsilateral hearing loss, so she decided to search an otolaryngological evaluation, at exploration of the patient, she had a smooth, spherical, whitish lesion with epithelial features and no evaluable pedicle, that obstructed the 90% of the right EAC at the inner third, rest of the evaluation without alteration of the mandibular dynamics, cylindrical neck without palpable masses, mobile central trachea with crepitus, an incisional biopsy of the right EAC tumor was performed and the anatomopatologic reported was an in situ squamous cell carcinoma.
Introduction
Within the tumors of the head and neck, squamous cell carcinoma of the external auditory canal has a low incidence and prevalence, 1-6/1,000,000 habitatns per year [1-3]. Due to the lack of reported cases, it is a great challenge for the otolaryngologist to carry out a correct staging as well as an adequate therapeutic protocol, an overview of the literature refer it with a wide range of clinical presentation, being more common in patients of the fifth or sixth decade of life, with a broad clinical picture concordant with: otalgia, purulent or hematic otorrhea, conductive hearing loss, and also in some cases with facial palsy, temporomandibular joint dysfunction or preauricular tumor.
Case Report
75-year-old female patient with family history of cancer in two siblings, exposure to biomass smoke for more than 200 hours/ year since her childhood, traumatic history: a car accident suffered one year ago with concussion in right temporal region, without requiring hospital management without apparent complications, but since then, she started feeling intermittent singing and burning otalgia on the right ear and ipsilateral hearing loss, and three months later she also had intermittent right hematic otorrhea. She denied vertigo and/or hyperthermia. She received treatment on multiple occasions with topical and systemic antibiotic with mild improvement and post-term exacerbation of symptoms. At the physical examination, the right ear was reported as normoinsert not- painful-to-manipulation pinna, otoscopy shown an EAC obstructed in 90% in its internal third by a spherical, smooth, epithelial-like, reddish colored lesion, friable to manipulation, sessile, with grey foul-smelling otorrhea and pain with the manipulation of the canal and the lesion, tympanic membrane wasn't valuable (Figure 1), the left ear was normoinsert, not-painful-to manipulation pinna, permeable EAC, otoscopy with normal tympanic membrane, mobile to maneuvers of Toynbee and Valsalva, light cone present, hammer impression was observed, cylindrical neck without anormal masses, mobile central trachea with crackle, normal carotid pulses. Accumetry was performed with a 512 Hz tuning fork and reported as positive Rinne in left ear and negative Rinne in the right ear, Weber test was lateralized to the right, and with right elongated and left shortened Schwabach. No compromise of mandibular dynamics. Facial mimics and the rest of cranial nerves exploration remained normal [4-6].
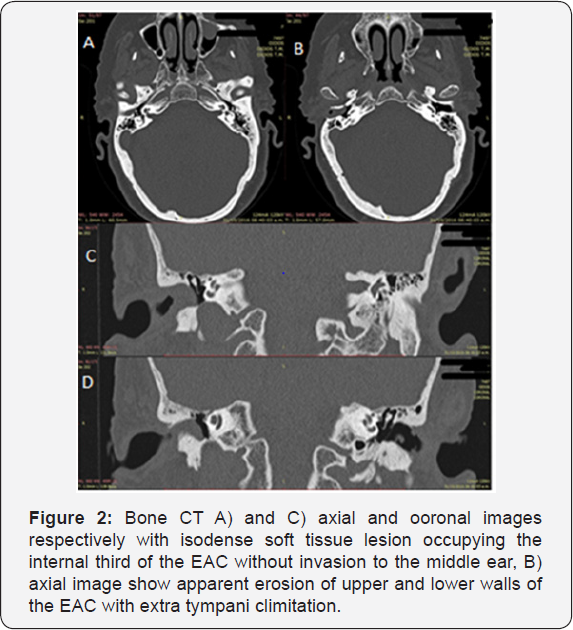

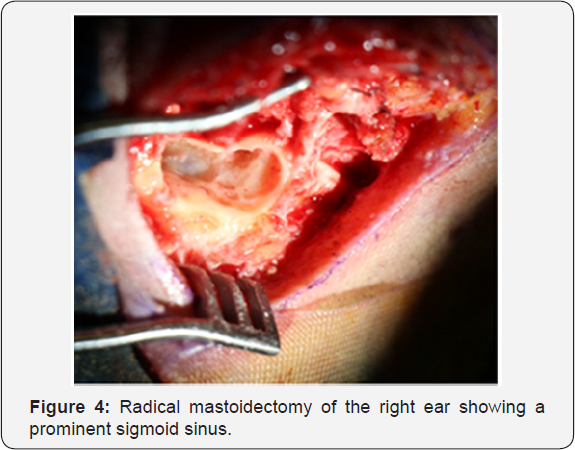
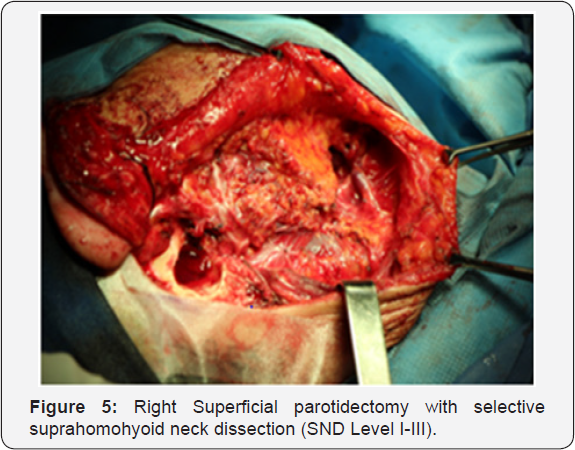
A computerized tomography (Figure 2) and simple and contrasted magnetic resonance imaging (MRI) were performed as diagnostic aids (Figure 3). In the tomography an isodense tumor at the expense of soft tissue was observed occupying the right CAE in its internal third of approximately 6*8*12 mm with apparent erosion in its previous wall, respecting the middle ear. In the MRI sequence T1 a homogeneous isointense lesion, brain tissue like, was identified occupying the internal portion of the right EAC without invasion ofthe middle ear. In the T2 sequence a communication from the extension pedicle to the anterior wall of the EAC was visualized, with no invasion of the parotid space, then at the office an incisional biopsy was performed under local anesthesia, taking an irregular light brown and soft edges, 0.6x0-4x0-3 cm out in size sample, with histopathological result of squamous cell carcinoma in situ. With this result, our patient was protocolized with the Pittsburgh TNM staging; a T2N0M0 score was given for which the treatment protocol was based on a stage II. It was decided to perform a lateral resection of the right temporal bone with radical mastoidectomy (Figure 4), to complement the surgical treatment a right superficial parotidectomy (Figure 5) and a selective suprahomohyoid neck dissection (SND level I-III) was also done [7-9].
Discussion
Squamous cell cancer is an entity with slight incidence and prevalence and with lesser bibliography or guides well established for its treatment, Within patient staging, the University of Pittsburgh-modified TNM classification, suggested by Arriaga 1990, modified by Moody [10], has allowed a standardization of the classification, treatments and results of the patients. Surgical resection is a crucial in the treatment, an early surgical intervention is associated with an increased survival, depending of the clinical stage correlated with the therapeutic algorithms can give us the accurate management (Figure 6). Cure rates have been increasing sin 1970 due to the progress of imaging diagnosis and improvement in skull base microsurgery. Actually in the literature, Gidley reported a 5-year survival of 48% for T1 and T2 stages and 28% for T3 and T4 stages.

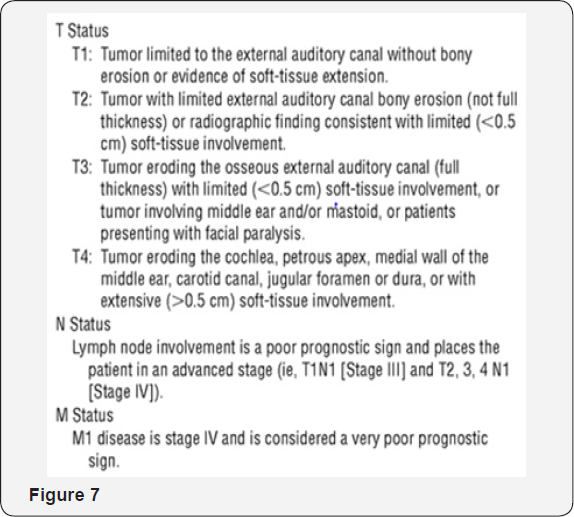
In a retrospective meta-analysis of 21 patients, Koller et al. [11] found that a temporal or subtotal stage-dependent lateral resection combined with parotidectomy as well as a neck dissection demonstrated a better 5-year survival prognosis. Recent reports recommend radical radiotherapy as monotherapy for T1 classification, and radiotherapy combined with surgery for T2 and T3 stages; Considering T4 as unrespectable (Figure 7). A study by Mazzoni et al. [12] had shown that patients with stage T1 and T2 have a better survival result at 5 years with lateral resection of temporal bone, whereas T3 and T4 have less favorable results, presenting local recurrence and involvement of lymph nodes.
Tumors with extension to periauricular soft tissue as well as parotid space had a better evolution compared to those that spread to the mastoid or to the rest of the divisions of the temporal bone. The possible reason is due to the routes of dissemination of the natural foramina of the bone. Within the dissemination pathways, we can mention the fissures and channels ofthe temporal bone such as branches for the auditory canal, canal of the posterior auricular nerve, canal of the auriculotemporal nerve, tympanic cord and vascular channels, among others. Resection of tumors involving periauricular soft tissue leads to more reliable tumor-free margins without the need to resect vital structures and a possible second reconstruction [13-15].
In cases of nodal affection, radical neck dissection is accepted within the literature, therefore is a different case for the N0 presentation, which remains controversial. Approximately 4.5 to 31.8% of nodes are positive for neck dissection. The case of micro metastasis with clinically negative neck is 17% [16]. Until day, there is no evidence in the literature that support the decision not to treat the neck, so a prophylactic dissection can be performed. The type of neck dissection is still controversial. An accepted choice is the dissection of levels Ib to III together with a block resection and superficial parotidectomy. The risk of metastasis at level IV is considered in cases of positive nodes at higher levels or in recurrent tumor after surgery and / or radiotherapy [17,18].
Conclusion
Nowadays, squamous cell carcinoma of the EAC still being a therapeutic challenge for the different specialists involved in its diagnosis and management, whether medical or surgical. Without specific treatment guidelines due to their low incidence, the attending physician must have an extensive knowledge of the literature as well as the anatomy and surgical techniques, have a good medical center with an adequate multidisciplinary team and offer the best therapeutic according on the needs of the clinical stage. A fundamental part of the diagnosis is based on the clinical presentation, although not specific, is a guideline. Persistent fetid otorrhea despite adequate medical treatment, together with progressive chronic otalgia and absence of clinical data on malignant otitis externa, we consider this enough reason to rule out oncological pathology of the EAC. The timely diagnosis as a therapeutic tool should not be underestimated, an early stage leads to a better survival, and therefore we consider that it is of vital importance to keep in mind the oncological pathology within the differential diagnosis of chronic otorrhea.
References
- David Lobo, José L, Llorente, Carlos Suarez (2008) Squamous Cell Carcinoma of the External Auditory Canal. Skull Base 18(3).
- Gidley P (2009) Managing malignancies of the external auditory canal. Expert Review 9(9): 1277-1282.
- (2015) Cummings Otolaryngology-Head & Neck Surgery (6th edn). In Paul W Flint, Bruce H Haughey, Valerie Lund, John K Niparko, K Thomas Robbins, et al. (Eds.). elsevier, USA. pp. 3624.
- Kazuhiko Ogawa, Katsumasa Nakamura, Kazuo Hatano, Takashi Uno, Nobukazu Fuwa (2007) Treatment and Prognosis of Squamous Cell Carcinoma of the External Auditory Canal and Middle Ear: A Multi- Institutional Retrospective Review of 87 Patients. International Journal of Radiation Oncology Biology Physics 68(5): 1326-1334.
- Koppany Visnyei, Rupinder Gill, Efat Azizi, Bruce culliney (2012) Squamous cell carcinoma of the external auditory canal: A case report and review of the literature. Oncology Letters 5(5): 1587-1590
- Michael Sand, Daniel Sand, Dominik Brors, Peter Altmeyer, Benno Mann, et al. (2008) Cutaneous lesions of the external ear. Head and Face Medicine Sitio 4: 2.
- Kazuhiko Ogawa, Katsumasa Nakamura, Kazuo Hatano, Takashi Uno, Nobukazu Fuwa (2007) Treatment and Prognosis of Squamous Cell Carcinoma of the External Auditory Canal and Middle Ear: A Multi- Institutional Retrospective Review of 87 Patients. International Journal of Radiation OncologyBiology Physics 68(5): 1326-1334.
- (2015) Bailey's Head and Neck Surgery-Otolaryngology I-II (5th edn). In Jonas T Johnson, Clark A Rosen (Eds.). CRC Press, USA.
- Ting Zhang, ChunFu Dai, ZhengMin Wang (2013) The misdiagnosis of external auditory canal carcinoma. European Archives of Oto-Rhino- Laryngology 270(5): 1607-1613.
- Moody, Stephanie A, Hirsch, Barry E, Myers, et al. (2000) Squamous Cell Carcinoma of the External Auditory Canal: An Evaluation of a Staging System. American Journal of Otology 21(4): 582-588.
- Kollert M1, Draf W, Minovi A, Hofmann E, Bockmuhl U (2004) Carcinoma of the external auditory canal and middle ear: therapeutic strategy and follow up. Laryngo-rhino-otologie 83(12): 818-823.
- Mazzoni, G Danesi, E Zanoletti (2014) Primary squamous cell carcinoma of the external auditory canal: surgical treatment and longterm outcomes. ACTA Otorhinolaryngologica Italica 34: 129-137.
- Ito M, Hatano M, Yoshizaki T (2009) Prognostic factors for squamous cell carcinoma of the temporal bone: extensive bone involvement or extensive soft tissue involvement? Acta oto-laryngologica 129(11) 1313-1319.
- Zhiye Wang, Meizhu Zheng, Shuang Xia (2016) The contribution of CT and MRI in staging, treatment planning and prognosis prediction of malignant tumors of external auditory canal. Clinical Imaging 40(6): 1262-1268.
- Jason A Beyea, Aaron C Moberly (2015) Squamous Cell Carcinoma of the Temporal Bone. Otolaryngol Clin North Am 48: 281-292.
- Prabhu R, Hinerman RW, Indelicato DJ, Morris CG, Werning JW (2009) Squamous cell carcinoma of the external auditory canal: long-term clinical outcomes using surgery and external-beam radiotherapy. American journal of clinical oncology 32(4): 401-404.
- Takenaka Y, Cho H, Nakahara S, Yamamoto Y, Yasui T, et al. (2015) Chemoradiation therapy for squamous cell carcinoma of the external auditory canal: A meta-analysis. Head Neck 37(7): 1073-1080.
- Chen WY, Kuo SH, Chen YH, Lu SH, Tsai CL, et al. (2012) Postoperative intensity-modulated radiotherapy for squamous cell carcinoma of the external auditory canal and middle ear: treatment outcomes, marginal misses, and perspective on target delineation. International Journal of Radiation Oncology Biology Physics 82(4): 1485-1493.





























