Cervical Actinomicosis - Difficulties in Diagnosis and Treatment- Case Report
Cristina Otilia Laza1*, Luminita Gentiana Micu2, Dorian Micu - Citosan3 and Curtali Licdan4
1ENT CLINIC, Romania
2Anatomo-pathology-department, Romania
3Anatomo-pathology, Romania
4Infectious Disease Clinical Hospital, Romania
Submission: September 18, 2017; Published: September 25, 2017
*Corresponding author: Cristina Otilia Laza-ENT Senior head and ne ck surgeon, ENT/OMF Clinic, SCJU SF, Apostol Andrei Constanta, b-dul Tomis 145, Constanta 900591, Romania, Tel: 40722840980; Email: cristinaotilia@gmail.com
How to cite this article: Cristina O L, Luminita G M, Dorian M, Curtali L. Cervical Actinomicosis - Difficulties in Diagnosis and Treatment- Case Report. Glob J Oto 2017; 10(5): 555797. DOI: 10.19080/GJO.2017.10.555797
Abstract
We present a case of a 54 -years old man with a third month history of slowly, painless enlargement on the right part of the neck.. He denied recent dental extraction or oral trauma, but he had positive history for pulmonary tuberculosis and he abuse alcohol and tobacco. Physical examination showed a no tender latero-cervical right mass with a bluish skin and multiple ulcerations with fistulous tract with a yellow purulent fetid discharge also with caseous granules yellow like sulphur draining from them. Biopsy revealed no malignancy or tuberculosis or mycosis, however Gram colour stains were positive for Actinomyces. A complete endoscopic examination -pan endoscopy on general anaesthesia before the debridement operation exclude a head and neck malignancy, because of the risk factors .Treatment start with iv penicillin ,and the surgical resection day by day of the necrotic tissue was removed .He still continue the treatment with oral penicillin and the evolution is slowly positive..
Keywords: Actinomyces Israelli; Sinus tract; Sulphur granules
Case Report
A 54 years old men was admitted in our Clinic with a tumoral laterocervical mass - 3 months old now, initially growing slow without pain or respiratory or deglution problems Progressively the mass grow and with increasing in volume subsequently change his colour- the skin was infiltrated with a red bluish colour, next multiple ulcerations appear in the skin one by one with a fistulous tract each one and granulous tissue surrounding the hole. A fetid yellow purulent discharge was draining trough the holes. In the pus, between granulation and blood with discover yellow like sulphur granules-with a caseum like aspect.
Symptoms
Patient was asthenic complaining of physical and mental fatigue, weight loss-12 kg in 3 months, anorexia; accuse local discrete pain, and sometimes odynophagia with referred otalgia on the same side every day the temperature was 37-37, 5 C maximum.
History
In anamnesis beside the evolution of the mass, we remark chronic intoxication with 2 packs of cigarettes / day, and alcohol abuse -He leaved in very bad condition in an old stable for cows, in his medical pass recognise pulmonary TB ,and was still in attention of an pneumologist for Chronic Bronchitis .
Physical examination: General status appear influenced, sub fever 37.2oC on the presentation in Emergency, underweight .
A. ENT exam
a. Inspection: on the right laterocervical region we observe an imprecise tumoral mass with no clear limits extended from the angle of the jaw till the cricoid cartilage .The mass was a diffuse irregular indurated tumour with red-purple skin, presenting large fistulous openings surrounded by granulous tissue, with a serous leaking yellow pus, containing fetid yellow granules with caseous aspect. Aerodigestive axis was shift to the opposite side just a little bite [1-6].
b. Palpation: cervical tumoral mass is with a hard consistency vaguely painful ,cervical lymph node are not palpable, laryngeal cracment currently normal, mandibular mobility normal, basilar edge of the mandible intact. Exploring the fistulous tracts with an instrument we discover that are shallow subcutaneously.
c. Ex. oral cavity: very bad oral hygiene, multiple cavities, periodontitis,tartrum, fetid halitosis, hairy tongue.
d. Bucopharyngoscopy, laryngoscopy: Pharynx, larynx with chronic catarrhal tabagic inflammation, no tumoral masses on the head and neck area
B. Laboratory tests
a) CBC anemia, mild leukocytosis,
b) inflammatory nonspecific tests-ESR, elevated fibrinogen- PCR-positive
c) some normal biochemical tests, like blood level of glucosis,with normal urinary tests, creatinine, ureea but with the liver destroyed by alcohol with enlargedement, all the test TGP, TGO, CK, LDH , are anormal- including of GGT -marker of alcoholism (Figure 1).

d) Bacteriological exam was possible colecting directly from proces granulated material and pus ,when order cultures on aerobic and anaerobic mediums ,also we ask for a mycological examination on specific mediums like Saboureaud [7].
e) Gram stain revealed -a highlights filamentous bacteria - Actinomyces. Israelli, and Bacteroides anaerobic germs.
f) Cultures of the pus on agar- blood medium in .aerobic and nonaerobic enviroment were negative.
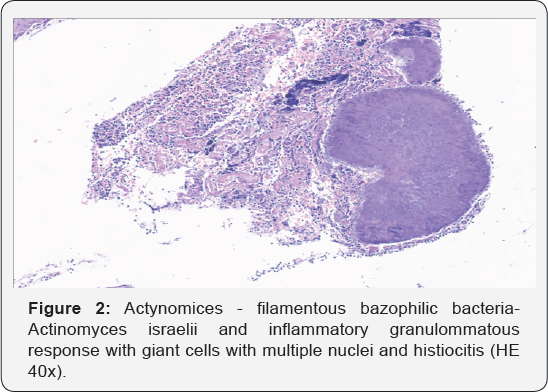
g) Biopy -for anatomopathology revealed -nonspecific granulommatous inflammation with abcess formation (Figure 2).
C. Imagistics:
a) X-ray of the chest
b) sechelar fibrosis on the superior lob of the left lung
c) Panorex - offers a lots of cavities , apical abscesses, granulomas-real dental status
d) CT scan of the neck coronal and axial, profile view -reveale a superficial infiltrative tumoral mass limited to the skin, subcutaneous tisue and platisma,also SCM and inferior part of the right parotid gland .Large vesels of the neck were normal also the lymph nodes, thyroid glands also pharynx and larynx were normal, without invasion [8].
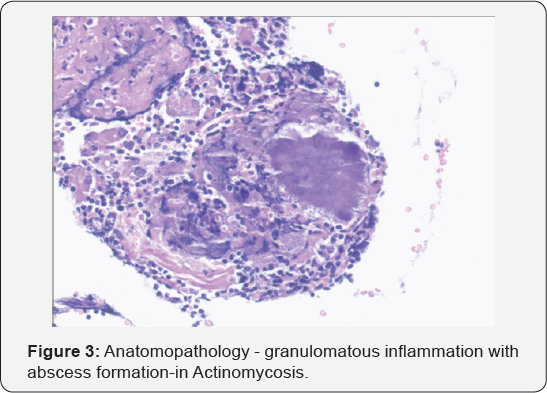
e) Endoscopy -Fibroscopy -no tumors in the pharynx , larynx, MLSS for the larynx is necessary in case of dysphonia,but mobility was normal, normal calibre, normal glotic space, difuse redness of the mucosa (Figure 3).
Differential Diagnosis
a. Considering risk factors other lesions were excluded mainly with biopsy:
i. Bacterial adenitis with spontaneous drainag.
ii. Chronic supurative adenitis -lymph node Tuberculosis -scrofulous type.

iii. Cat scratch diseases
iv. Sphyfilis third stage
v. ulcerated, infected Metastasis of an head and neck carcinoma (Figure 4).
vi. Fibrous dysplasia of the mandible
vii. Adamanytinoma of the mandible
b. Treatment: Medical treatment is simple but long- Penicillin G -20mil UI / day iv. associated with Metronidazole for six weeks, then we continuu with - po.Ospen -4 million UI / day . for six months. Surgical treatment- drainage, lavage with betadine, peroxide, local antibiotics, and resection of the necrotic tissue. Currently the patient is being treated orally with obvious but slowly improvement and is constantly seen by an ENT and Infectious Disease doctors [9].
Introduction
The term, 'Actinomycosis" comes from the Greek Mykes -micoza and aktino-after radial aspect of the germ in sulphide grains due to this structure ,as well as its slow-induced disease was long thought that is a fungal infection. In 1857 was made the first description of actinomycosis in humans after 1826 had been described in cattle. In 1877 Bollinger found germ granules Actinomyces bovis in - lumpy jaw disease. In 1878, Israel found sulphide granules in autopsy material, and human actinomycosis described in 1885 and found that the species are just host and without another pathogen they supraietuiesc not found in the soil and not the plants. In 1940 was established as the nature of the microbe and its characteristics and treatment. If before the disease was common and long-term complications and sequelae, today is a rarity often undiagnosed because of the difficulty of isolating the germ but the prognosis has improved and death is an exception [10-14].
Definition
Actinomycosis is an subacute-chronic granulomatous, suppurative infection characterized by multiple abscesses and external fistulas on the skin. Exploring the tracts with a special instrument we expressed pus with sulphide granules. Is produced by gram-positive, filamentous, nesporulati germs belonging to the genus Actimonyces, which led to the slowly progressive disease. Clinical manifestations take one of three forms:
a) cervicofacial (55%)
b) thoraco-pulmonary (15%),
c) abdominal -pelvine (20%). but can catch muscles, bones,CNS, or disseminate through the blood - basically can affect any organ.
Ethiology
a) Order -Actinomycetaes
b) Family -Actinomycetaceae
c) Genus -Actinomyces
d) Aspect: gram positive, non -acidic, nesporulated filamentous bacils, long time were clasified between bacteria and mycosis
Classification
i. Actinomices. Israelii
ii. A. naeslundii/v/scosus
iii. A. Odontolyticus
iv. A. Viscosus
v. A. Meyeri
vi. A. Gerencseriae
vii. A.turkensis
viii. Aeropaus,
ix. A.mayer
x. Propionibacterium
Particularities
a) Actinomices contain a nuclear membrane, lack chitin, gluten, mitochondria, prokaryotic -bacteria mural -they grow slowly in the presence of an acid microaerophilic environment.
b) A. Israelli is a common commensal of the mouth, colon and vagina in humans and other mammals can not be considered symbiotic organism that does not have a reciprocal relationship with the host.
c) Can not be considered parasite that normally does not produce bad host, but survives phagocytosis thus can be considered as Mycobacterium tuberculosis optional intracellular parasite.
d) It can not be considered opportunistic because they do not cause disease in immunosuppressed.
e) The seed is considered virulent, perhaps this other germs is necessary to initiate disease.
f) It has never been isolated from nature.
g) Not demonstrated transmission from human to human.
Germs Accompanying Actinomyces
a. Staphylococcus / Streptococcus
b. Enterobacteriaceae
c. Actinobacillus comitans
d. Eikenella corrodens HACEK
e. Fusobacterium
f. Bacteroides
g. Peptostreptococcus
h. Enterobacteriaceae
They increse week pathogenity of Actinomyces species
Epidemiology
a. Incidence is very low in developed countries is very low ,in urban but also rural areas
b. Still is the disease with most highest percent of wrong diagnosis.
c. Most patients are at middle age and is a small predominance of actinomycosis in men
Risk factors
a. Immunosuppressed conditions -HIV, post-transplant status, post-radio-chemotherapy
b. Infectious diseases with lesions in mouth : herpes simplex, Shingles (Herpes Zoster), thrush;
c. Lesions caused by low-hygiene of the mouth, decayed teeth, paradontosis
d. Oral trauma by dental interventions
e. Malignant tumours of the mouth
f. Osteoradionecrosis
Pathology
The entrance gate is represented by these lesions (the interruptions of the mouth mucosa), the germ is able to survive in the bacterial plaque, tonsils' crypts, saliva etc. Characteristics: the evolution of this infection is slow and chronic. First appear the painless, woody, fibrotic swelling(s). After a while it is established the mature lesion which is soft, fluctuant and festered, being surrounded with red-purple-ish skin. Lastly, appear several fistulas, with sulphur granules that accompany purulent discharge, fibrous tracks which appear, disappear and reopens spontaneously. The central necrosis is represented by neutrophils sulphur granules and it can be extended to deep tissue such as bones, central organs, cartilages.
Oral Actinomycosis
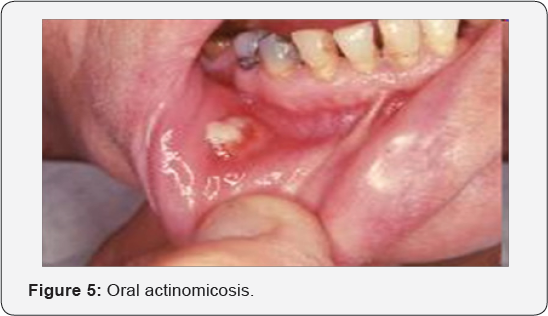
The mouth infection can be presented as an abscess or pseudotumour, periapical infection of the molars or premolars that is non-responsive to treatment. It can extend to gum's periosteal layer and inducing the painful periostitis or osteomyelitis. The saliva with Actinomyces can infect the salivary ducts and glands (Figure 5).
Facial Actinomycosis
The cervico-facial actinomycosis is present in 55% of the cases. The lesions appear as o tumoral mass, woody at palpation, with sub acute clinical evolution and with low-fever. The most-involved areas are the submandibular zones, the cheeks, parotid glands, teeth and tongue. The cutaneous infection can extend to the orbit, sinuses, scalp and endocranial area. The cervical infection extends without specific boundaries and it can evolve without lymphadenopathy. It can invade the trachea, the larynx, the pharynx, the jawbone, producing the osteomyelitis.
Cervical and facial actinomycosis
The tumoral mass is hard, painless with the invasion of the skin, platysma muscle and other muscles, aero-digestive organs. The skin looks purple. The tumour looks fluctuant. Throughout the fistulas that appear later flows fetid pus, with sulphur granules, yellow, caseous, 2mm diameter, that represent the micelles.
Radiology
The X-ray of the mandible shows sub periosteal reaction or attenuation of the bone tissue, osteomyelitis, fistulas with the bone as the go-off point. CT, MRI- scattered superficial infiltration probably extended to larynx, pharynx, glands, jaw-bone.
Characteristic: the central necrosis, fistulas, fibrosis.
Diagnosis
Lab tests: Pus sample from the lesion with bacteriology, directly or Gram-stain, hematoxilin-eozine treated cultures exanimated at microscope. Suction-puncture under endoscopic observation for bacteriologic and mycologic exam. Biopsy from the lesions- granulomatous inflammation, festered. Bacteriological exam, cultures from sulphur granules or directly: the cultures are hard to be realised because they are mostly negative. PCR-Protein- chain reaction- amplification of 16S r RNA gene and sequencing. Dosing of specific monoclonal antibodies.
Imagistics: ultrasound of the neck-for the glands and lymph nodes. X-rays mandible ,PANOREX ,neck prophile-erosion of the cartilages,thyroid ,cricoid or cervical spine. CT scans, in complex lesions. MRI -with a better exposure of the soft tissue
Complications
a. Otitis acute ,suppurated
b. Mastoiditis acute suppurated
c. Keratitis
d. Sinusitis most frequent maxillary-odontogenic
e. Mumps-invasion of salivary glands
f. Meningitis
g. Cerebral abscess
h. Osteomyelitis of maxilla
i. Thrombophlebitis of the cavernous sinus
j. Bloodstream dissemination-Septicaemia
k. Larynx invasion with pericondritis - phlegmonous laryngitis with dyspnoea
l. Pharynx invasion with sore throat-
Lung actinomycosis
The primary actinomycosis involving the lung can appear as:
i. a chronic peripheral pulmonary segment condensation;
ii. a nodule or a mass with holes accompanied with periorificeal condensation and adjacent pleural thickening
iii. lymphadenopathy mediastinal
iv. the condensation can involve the pleura, pericardium, mediastinum or the thoracic wall.
v. The aspect is often wrongly believed to be carcinoma or other granulomatous infections like tuberculosis or sarcoidosis ,nocardiosis
Pelvic disease
i. Risk factor: intrauterine contraceptive device >1 year- months after extraction
ii. Symptoms: usual starts with fever, weight-loss, abdominal pain,vaginal abnormal bleeding or leakage.
iii. Endometritis -> mass/tubal or ovarian abscess.
iv. Diagnosis: ultrasound, bacteriological examination.
Abdominal actinomycosis
This form evolves very slow patients present fever, diarrhoea, weight-loss, constipation, abdominal pain. The infection starts with the lesion of the gastro-intestinal mucosa with a foreign object - fish-bone, chicken-bone, ulcerations typhoid fever or dysentery, or after a surgical intervention or other type of trauma. It can present itself as appendicitis, acute abdomen. It can disseminate with the help of the blood stream and can extend to liver or spleen.
Treatment: Treatment is not only surgical and also drug- related therapy is required.
a. Medical treatment: Long-term high-dose of antibiotics-ex. G-Penicillin i.v. 18-24M IU per day 2-6 weeks and continue cu per os Penicillin/Amoxicillin 6-12 months, fluoro-quinolone, tetracycline, macrolides. Treatment of other infections related to actinomycosis: cephalosporins, metronidazole-specific for anaerobic germs
b. Surgical treatment: under local or general anasthesia -local debridement, resection of the necrotic areas, washout of the tract with, betadine, peroxide, sol with antibiotics till the complete healing
Conclusion
a. Since the first description of human actinomycosis in 1878 by Israelli until present time, a lot of knowledge has been gaining about germ, disease incidence, diagnosis and treatment.
b. Actinomycosis is a chronic granulomatous inflammatory disease, suppurative. May include a wide variety of human organs. Beside this case last year I had the surprise to discover a patients with clinical and CT scan-aspect of tumoral rhinopharyngeal mass -suspect of malignancy but the biopsy -anatomophatologic,IHC, revealed Actiomycosis. At infectious disease department Actinomyces Israelii was identified ,After 3 month of treatment the mass disapeared and till now the cavum remain clear.
Another strage case was a lady with hypertrophied lingual tonsils,also with a very white tongue ( pseudomembranous candidiasis) Also in Infection Disease department A Israelli was discovered and after 2 month of treatment the tongue was clean and the lingual tonsils with a smaller size, but in this case very complex it was just a temporary diagnosis for her sufferance finaly after repeted biopsies, -MLSS-laser CO2, diode, KPT, coblation reduction of the tonsils,and after diverse treatments and diagnosis like Sjogreen, Tuberculosis, LED it proved to be an autoimmune disorder.
c. The most common pathogens known are Actinomyces. Israelli, and a bacterium Gram-positive difficult to identify which typically colonize the mouth, colon and genital tract.
d. Actinomycosis can affect individuals of any age usually immunocompromised persons.
e. There are three main clinical forms; Cervicofacial, thoracopulmonary and abdominopelvic, the most common being cervicofacial takes the form that can mimic neoplasia.
f. A final diagnosis is made by the mycological identification of the germ in the sulphur grains or cultures . It is difficult to diagnose only on clinical and radiological findings.
g. Even the symptoms are non-specific, actinomycosis should be considered in the differential diagnosis of a tumoral mass.
References
- Funke G, von Graevenitz A (1995) Infections due to Actinomyces neuii (former "CDC Group 1 coryneform” bacteria). Infection 23(2): 73-75.
- Siqueira JF, Rocas IN (2003) Polymerase chain reaction detection of Propionibacterium propionicus and Actynomyces radicidentis in primary and persistent endodontic Infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96: 215-222.
- Perlow H, Wigton T Yordan EL (1991) Disseminated actinomycosis pelvic Presenting as metastatic carcinoma: association with the progestasert intrauterine device. Rev Infect Dis 13(6): 1115-1119.
- Cintron JR, del Pino, Duarte B (1996) Abdominal actinomycosis. Dis Colon Rectum 39(1): 105-108.
- Henderson SR (1973) Associated with Pelvic actinomycosis year intrauterine device. Obstet Gynecol 41(5): 726-732.
- Koshi G, Lalitha MK, Samraj T (1981) Brain abscess and other protean Manifestations of actinomycosis. Am J Trop Med Hyg 30(1): 139-144.
- Maxon S (1998) Actinomycosis - in Textbook of Pediatric Infectious Diseases. WB Saunders Co; Philadelphia, USA, 1587-1590.
- Robinson JL Vaudry WL, Dobrovolsky W (2005) Actinomycosis -presenting as osteomyelitis in the pediatric population. Pediatric Infect Dis Journal 24(4): 365-369.
- Russo (1995) Agents of actinomycosis. In: Mandell G, Bennett J, Dolin R, eds. Principles and Practice of Infectious Diseases. 4th edn. Churchill Livingston, USA 2280.
- Belmont MJ, Behar PM, Wax MK (1999) Atypical presentations of actinomycosis. Head Neck 21: 264-268.
- Allen HA, Scatarige JC, Kim MH (1987) Actinomycosis: CT findings in six patients. AJR Am J Roentgenol 149: 1255-1258.
- Silverman PM, Farmer JC, Korobkin M, Wolfe J (1948) CT diagnosis of actinomycosis of the neck. J Comput Assist Tomogr 8: 793-794.
- Nagler R, Peled M, Laufer D (1997) Cervicofacial actinomycosis: a diagnostic challenge. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83: 652-656.
- Ermis I, Topalan M, Aydin A, Erer M (2001) Actinomycosis of the frontal and parotid regions. Ann Plast Surg 46: 55-58.





























