Prevalence of Haller cells on Computed tomography and correlation with Maxillary sinusitis: A Retrospective Study
Neha Koshal1, Deepa Jatti Patil2*, Gagan Puri3, Ajay Pal Kataria4, K Aravinda5 and Rajesh Gupta6
1Senior lecturer, Yamuna Dental College and Hospital, India IMDS, Reader, Yamuna Dental College and Hospital, India
2MDS, Professor and HOD, Yamuna Dental College and Hospital, India
3Senior lecturer, Yamuna Dental College and Hospital, India
4Professor MDS, Senior lecturer, Yamuna Dental College and Hospital, India
5,6Department of Oral Medicine, Diagnosis and Radiology, Swami Devi Dyal Dental College and Hospital, Swami Devi Dyal Dental College and Hospital, India
Submission: September 13, 2017; Published: September 22, 2017
*Corresponding author: Deepa Jatti Patil, Reader, MDS, Department of Oral Medicine, Diagnosis and Radiology, Swami Devi Dyal Hospital and dental college, Golpura, Panchkula, 125121, Haryana, India, Tel: 091-7696263934; Email: id-iafdeepa@gmail.com
How to cite this article: Neha K, Deepa J P, Gagan P, Ajay P K, K Aravinda, et al. Prevalence of Haller cells on Computed tomography and correlation with Maxillary sinusitis: A Retrospective Study. Glob J Oto 2017; 10(5): 555796. DOI: 10.19080/GJO.2017.10.555796
Abstract
Objectives: Haller cells (HC) are located in the medial orbital floor immediately lateral to the maxillary infundibulum. Its role in causing sinusitis is controversial. The purpose of this study was to demonstrate the prevalence of HC on Coronal Computed tomography (CT) images and association of HC with ipsilateral maxillary sinusitis and orbital floor dehiscence
Materials &Methods: Coronal CT images of 150 patients were retrieved and analyzed. The size of the HC, existence of maxillary sinusitis and orbital floor dehiscence was recorded on a data sheet. For descriptive statistical analysis, the Chi Square test & Pearson's coefficient was used
Results: Haller cells were seen in 30.39% of patients. There was no statistically significant association between the existence and size of Haller cells and maxillary sinusitis and orbital floor dehiscence
Conclusion: The present study has demonstrated the usefulness of Computed tomography on the depiction of complex sinonasal anatomy and its anatomic variations. The mere presence of HC cannot be attributed to maxillary sinusitis. Haller cells do play a pivotal role in ventilation and drainage of paranasal sinuses and endoscopic surgeries.
Keywords: Haller cells; Coronal CT images; Maxillary sinusitis; Orbital floor dehiscence
Introduction
Orofacial pain is a diagnostician's enigma. It is often distressing to the patient as it presents with various symptoms of pain and headache and is associated with myriad causes. Chronic sinusitis is one of them. The paranasal sinuses (PNS) are maintained in a state of health due to the physiological process of mucociliary clearance. This could be disturbed due to the anatomic variations of the PNS and osteomeatal complex (OMC) contributing to persistent sinusitis. Functional endoscopic sinus surgery (FESS) addresses these anatomical variations and restores the normal physiology of the paranasal sinuses. It is important to correctly identify these anatomic variations of the PNS for proper diagnosis and treatment [1,2]. Computed tomography (CT) scan is the method of choice for evaluation of paranasal sinuses and the coronal plane is the preferred imaging plane that best displays the ostiomeatal complex [3].
Apart from the sinuses, some anatomical variations like Haller cells (HC) are best seen on CT. These cells are frequently seen as incidental findings on CT examination of paranasal sinuses and can cause sinusitis. Although HC are anatomical variations in the development of the nose and paranasal sinuses, they have been held responsible for patient's symptoms and are thus clinically significant. Their prominent location on the medial portion of the orbital floor and lateral to the maxillary infundibulum disturbs the normal pattern of mucociliary flow& predisposes patients to recurrent maxillary sinusitis. HC can also pose difficulties during endonasal procedures [4-6].
The importance of anatomic variations as a predisposing cause of sinusitis has been stressed by several authors. They can compromise already narrowed drainage pathways and produce significant obstruction. But as emphasized by Stammberger and Wolf [7]; they do not represent diseases state as per se. A small number of studies have shown a considerable relationship between presence of HC, its size and sinusitis [4,5,8] whereas some studies have not found a significant association [9,10]. This study was performed to assess the prevalence of HC & whether any relationship exists with maxillary sinusitis as envisaged on coronal CT images. At the same time we would also determine the association between HC size with maxillary sinusitis and dehiscence of orbital floor.
Materials and Methods
This retrospective study was performed at an advanced digital imaging centre, Chandigarh. The CT image volumes of 150 patients were retrieved from the digital imaging and communications in medicine (DICOM) archive folder who visited the center between February 2014 to June 2014. Approval for the study was obtained from the institutional ethical board. CT images were acquired with Siemens Somatom definition- dual source 64 slice CT (4128 slices) with 9-inch field of view and a resolution of 750 micron. The kvp & mA was set at 120 & 90 respectively The study reviewed coronal views in bony window; window width 2000 and window level 400. The thickness of the slice was 0.75 at an interval of 0.5.The software used was Osirix -Mac pro database. Patients aged between 18-60 years were included in the study. The CT images retrieved were advised for various dentomaxillofacial indications, including maxillofacial lesions, dental implants and orthodontic treatment. Patients with history of trauma, surgery pertaining sinus tumor, sinonasal polyposis of the oral and maxillofacial region were excluded from the study.
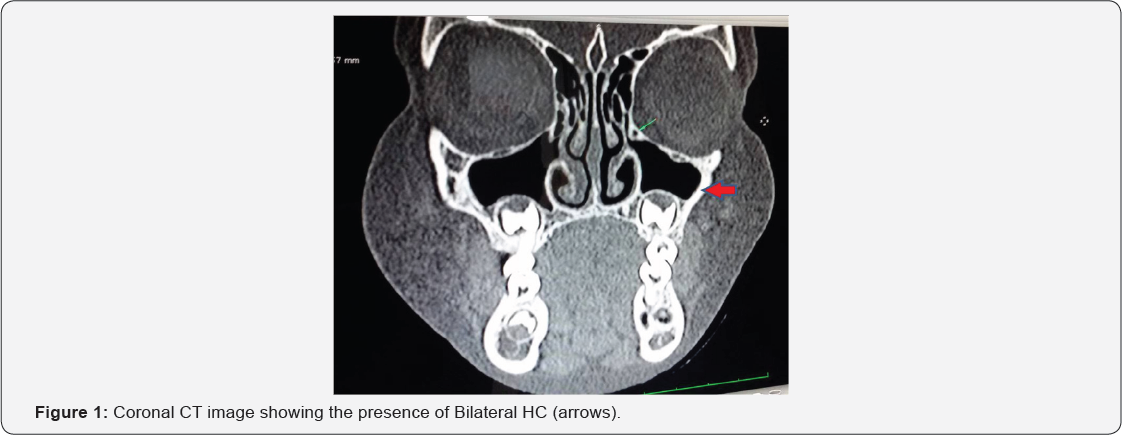
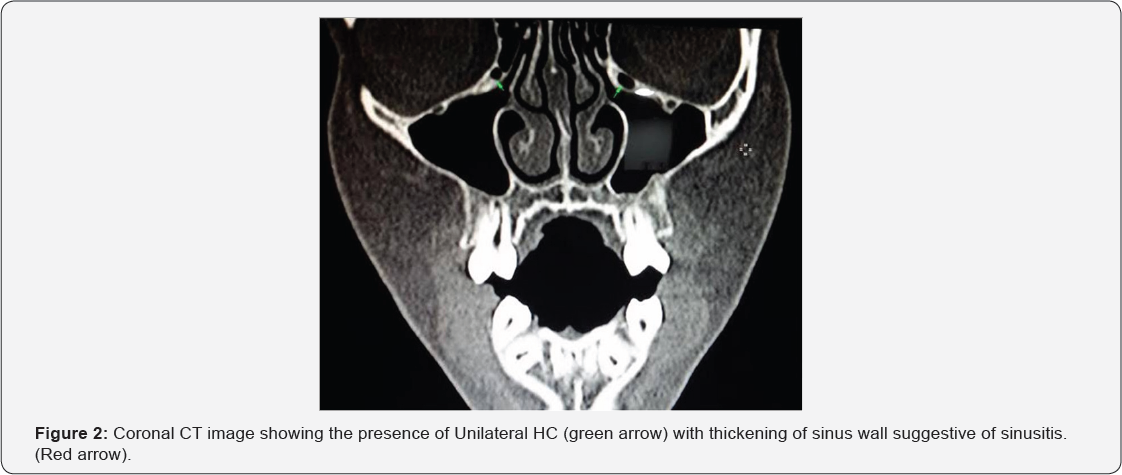
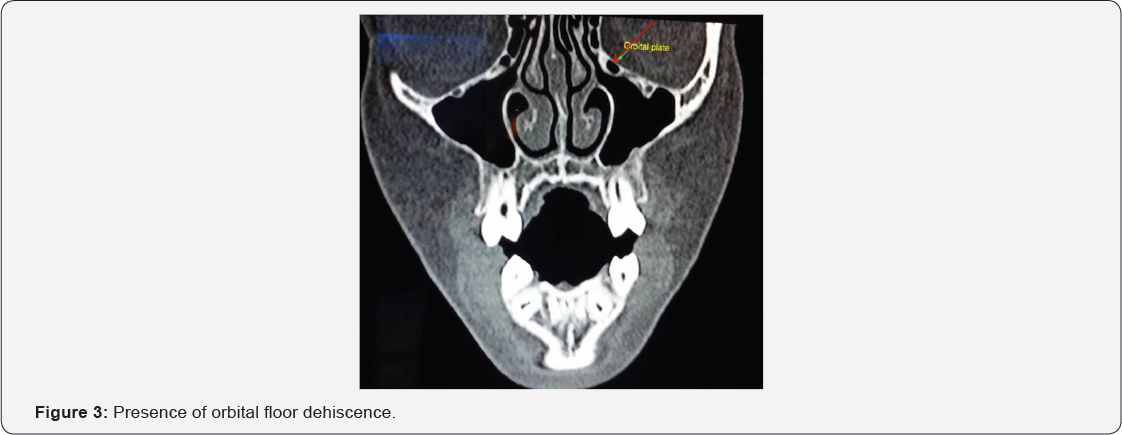
There has been a variation in the definition of Haler cell. Criteria for identification of Haller cells is adapted from Mathew et al. [9] Haller cells were recognized as air cells, of any size, located along the medial portion of the orbital floor and/or the lamina papyracea inferior to the bulla ethmoidalis, and continuous with the ethmoid capsule (Figure 1). Maxillary sinusitis was defined as radiographic evidence of thickening of sinus mucosa and/or fluid accumulation at any level (Figure 2) Dehiscence of the adjacent orbital floor was recognized as loss of bone density at any level. Whenever a clear decision between "very thin bony wall" and "total dehiscence" was not feasible, the results were accepted as dehiscence (Figure 3). The size of the Haller cell was measured at the maximum mediolateral dimension. The Haller cells were arbitrarily categorized based on the size into small (less than 2mm), medium (2-4mm) and large (greater than 4mm)
Statistical analysis
The findings were tabulated on a data sheet and results were analyzed on SPSS 18. For descriptive statistical analysis, the Chi Square test & Pearson's coefficient was used to evaluate the association of Haller cells with Maxillary sinus disease and orbital floor dehiscence. p value <0.005 was considered statistically significant.
Results
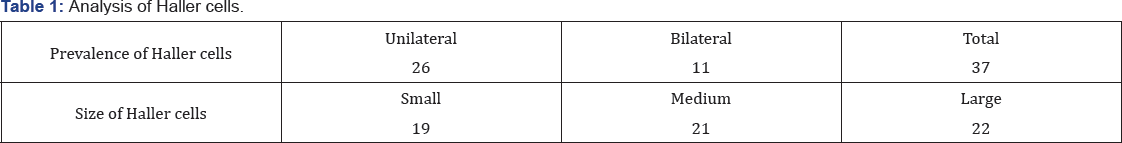
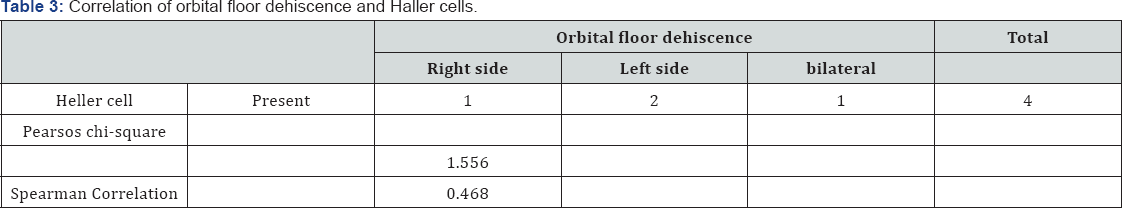
Out of 150 images 48 were discarded due to poor clarity. The results will be discussed for 102 images. The retrospective analysis included 43 females and 59 males with age ranging from 18 to 65 years (mean age 38 years). HC were recognized in 31 patients (30.39%); 11 (10.8%) bilateral and 26 (25.5%) unilateral; i.e HC were seen in 37 sides (36.3%). Total number of Haller cells were 62 in which 19 were small sized, 21 medium sized and 22 large sized (Table 1). Size of the haller cell varied from 0.8mm to 8.02 mm with a mean size of 3.72 mm. Two patients had three and one patient had four HC. HC concurring with ipsilateral maxillary sinusitis were encountered in 17 (45.94%) sides (8 on the right side and 9 on the left side (p value 0.639). No statistically significant association was seen between HC and ipsilateral maxillary sinusitis (Table 2). Concomitant presence of orbital floor dehiscence with HC was seen on the right and left sides in 01 and 02 patients, respectively and bilaterally in 01 patient. All the four had the presence of maxillary sinusitis. No statistically significant association was seen between HC and orbital floor dehiscence (Table 3). There was no statistically significant association between existence of HC, size of HC with maxillary sinusitis (> p.0.05).

Discussion
Albrecht von Haller an 18th-century Swiss anatomist in 1765 first recognized HC and was consequently named after him. They are alternatively called infraorbital ethmoid cells, as they arise from anterior ethmoid cells and are located in the medial orbital floor[11] . A diagnosis of a Haller cell cannot be made during transnasal endoscopy, because this cell is lateral to the lateral nasal wall. Because of structural superimposition, conventional radiology does not allow precise exploration of the region, especially of the anterior ethmoidal air cells, the frontal recess, and the upper two thirds of the nasal cavities, zones closely related to sinus physiopathology, and therefore interesting from the point of view of applied anatomy[12] . The revolutionary changes in the surgical treatment of sinusitis in recent years, particularly in endonasal endoscopic surgery, require the clinician to have a precise knowledge of nasal sinus anatomy and of the large number of anatomical variants in the region, many of which are detectable only by the use of CT [4].
CT scan with its excellent capability of displaying bone and soft tissue is the current diagnostic modality of choice for sinonasal disease. Frequently opacification of paranasal sinuses is observed on the standard plain film radiographs, but it lacks specificity as it could be due to of fluid (pus, mucous, blood etc.) thickened mucosa, tumor etc [13]. CT scan clearly shows the fine bony anatomy of the ostiomeatal complex ad recognizes the subtle anatomic variations and mucosal disease. The coronal plane is considered to be the best orientation for evaluation of the sinonasal tract as it clearly shows the ostiomeatal complex and the relationship of the brain to the ethmoidal roof and correlates closely with the surgical orientation [4,14]. Additionally, CT is extremely useful in the preoperative planning and in postoperative control in cases of endonasal interventions for providing important details on the normal anatomy and its variants [15]. Most recently, multiplanar and three-dimensional reconstruction has been utilized as a part of the routine in the study of paranasal sinuses, for providing higher quality diagnostic images and data than conventional CT, particularly in the identification of some anatomic variants [16].
Prevalence of Haller cells in the English literature is remarkably variable, ranging from 2.7% to 45.1% [4,17]. This variability could be due to the discrepancy in the description of HC. Kennedy and Zinreich [18] considered Haller cells as ethmoid cells projecting below the ethmoid bulla within the orbital floor in the region of the opening of the maxillary sinus. Bolger et al. [4] defined Haller cells as any cell located between the ethmoid bulla, the orbital lamina of the ethmoid bone and the orbital floor. Kainz et al. [8] recognized Haller cells as cells within the orbital floor. We adopted the definition by Mathew et al. [9] The inconsistency in the prevalence can be also accounted due to the sample size, patients' age group and race, narrow window setting and the CT techniques used [4].
In the present study a prevalence of 30.39% is seen which very high and comparable to other studies. Table 4 [9,14,15,16,19-32] summarizes the prevalence of HC as quoted by various authors. All of these studies were based on multislice CT except for the study by Mathew et al. [9] and Khojastepour L [31], et al which evaluated HC prevalence and clinical significance based on CBCT images. As demonstrated in Table 4, the prevalence of Haller cells is extremely inconsistent ranging between 2%- 70.3%. In the current study, the prevalence of Haller cell was 30.39%; which is almost similar to that obtained by [5,23]. The possible reasons for this discrepancy could be due to difference in interpretation of Haller cell, sample study or in the technique of CT scanning.
All detected HC in the study carried out by Wani et al. [26] were unilateral, while Fadda et al. [29] reported equal unilateral and bilateral HC. Earwaker demonstrated 4.6% HC were unilateral, and 3.3 % bilateral. HC were unilateral in 34.03% and bilateral in 65.97% of the cases as confirmed by Khojastepour L et al.[31] Mathew et al. [9] recognized 26% HC unilaterally and 34% bilaterally. Haller cells make up the posterior and superior wall of the ethmoid infundibulum. When the Haller cells become enlarged, they can cause obstruction of the ethmoid infundibulum and lead to maxillary sinusitis. In addition to distressing orofacial pain and sinusitis, numerous pathologies and symptoms associated with this entity include nasal obstruction, impaired nasal breathing, headache, chronic cough and mucoceles. Haller's cells can also restrict access to the maxillary sinus or the anterior ethmoidal cells during endonasal procedures, making it imperative for the surgeon to be aware of such variations that may incline the patient to increased risk of intraoperative complications [4,5,22].
As summarized in Table 4 the association of HC and sinusitis also varies. Its role in sinusitis is debatable with some authors reporting significant relationship and others finding no co-relation.The present study did not demonstrate a significant association between HC and sinusitis. Stackpole and Edelstein [5] and Yousem et al. established a significant increase in maxillary sinus mucosal disease in patients with medium or large Haller's cells (45.8%) vs. those with small cells (28.9%). They found Haller cells as important etiological factor in maxillary sinusitis certainly when the cells are large enough (greater than 6mm) to cause substantial narrowing of the maxillary infundibulum [5,32]. The present study found no significant association between the size of HC and maxillary sinusitis. However, in two patients with HC size more than 6 mm ipsilateral sinusitis was seen. Nitinavakarn et al. [10] however, confirmed no such association. A high rate of sinusitis quoted in other studies could be overrated because infectious sinusitis cannot be distinguished from allergic sinusitis on the basis of radiographic evaluation only [9].
The lack of association between the presence of Haller cells and the ipsilateral maxillary sinusitis could also be explained on the basis of the accessory maxillary sinus ostia in the lateral nasal wall; these ostia have previously been described in 14% of patients 9, 21 and would enhance maxillary sinus ventilation by functioning as an alternative route of drainage even in the case of mechanical obstruction of the maxillary infundibulum by a Haller cell. Orbital floor dehiscence was seen in three patients and was not statistically significant with sinusitis, which is in contradiction to Mathew et al. who demonstrated a statistically significant relationship. Sebrechts et al. [32] presented three case reports of unilateral orbital cellulitis, resulting from isolated inflammation of Haller cells. Since there is no lymphatic drainage system in the orbit, they consequently assumed infection spreading through a dehiscence in the orbital floor, lamina papyracea or sutures in the medial orbital floor. It is therefore advisable to look for Orbital floor dehiscence as it may be obscured by hypertrophic mucosa of the inflamed HC.
Conclusion
The present study has demonstrated the usefulness of CT on the depiction of complex sinonasal anatomy and its anatomic variations. A high prevalence of HC is seen which is in collaboration with previously performed studies. Statistically significant relation was not observed between HC, their size and maxillary sinus disease in the present study. Nevertheless it is important to recognize their role in disrupting drainage and ventilation of paranasal sinuses and their potential impact on operative technique and surgical safety. The simple presence of variants does not mean a predisposition to sinus pathology, except when other associated factors are present. The major limitation of the study is its small sample size. Future studies with larger sample size and analysis of anatomical variations in patients with rhino-sinusitis should be carried out.
References
- Zinreich S, Kennedy D, Rosenbaum A (1987) Paranasal sinuses: CT imaging requirements for endoscopic surgery. Radiology 163: 769775.
- Levine HL (1990) FESS, evaluation of surgery and follow up of 250 patients. Laryngoscope 100: 79-84.
- Zinreich S (1993) Imaging of inflammatory sinus disease. Otolaryngol Clin North Am 26: 535-547.
- Bolger WE, Butzin CA, Parsons DS (1991) Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 101: 56-64.
- Stackpole SA, Edelstein DR (1997) The anatomic relevance of the Haller cell in sinusitis. Am J Rhinol 11: 219-223.
- Kantarci M, Karasen RM, Alper F, Onbas O, Okur A, et al. (2004) Remarkable anatomic variation in paranasal sinus region and their clinical importance. Eur J Radiol 50: 296-302.
- Stammberger H, Wolf G (1998) Headaches and sinus disease: the endoscopic approach. Ann Otol Rhinol Laryngol 97: 3-23.
- Kainz J, Braun H, Genser P (1993) Haller's cells: morphologic evaluation and clinico-surgical relevance. Laryngo rhino otologie 72: 599-604.
- Mathew R, Omami G, Hand A, Fellows D, Lurie A (2013) Cone beam CT analysis of Haller cells: prevalence and clinical significance. Dentomaxillofac Radiol 42: 20130055.
- Nitinavakarn B, Thanaviratananich S, Sangsilp N (2005) Anatomical variations of the lateral nasal wall and paranasal sinuses: A CT study for endoscopic sinus surgery (ESS) in Thai patients. J Med Assoc Thai. 88(6): 763-768.
- Proetz AW (1953) Essays on the applied physiology of the nose. 2nd edn. Annals Publishing Co, St. Louis, MI, USA.
- Meschan I (1951) An Atlas of Normal Radiographic Anatomy, Saunders, Philadelphia, USA, 239-240.
- Weir DG (1997) Infective rhinitis and sinusitis. In: IS Makay, TR Bull (ed.) Scott Brown Rhinology, Butterworth & Co. 6th Edition.
- Scribano E, Ascenti G, Cascio F, Racchiusa S, Salamone I (1993) Computerized tomography in the evaluation of anatomic variations of the ostiomeatal complex. Radiol Med 86: 195-199.
- Lloyd GA (1990) CT of the paranasal sinuses: study of a control series in relation toendoscopic sinus surgery. J Laryngol Otol 104: 477-481.
- Miranda CMNR, Maranhao CPM, Arraes FMNR, Padilha IG, Farias LPG, et al. (2011) Anatomical variations of paranasal sinuses at multislice computed tomography: what to look for. Radiol Bras 44: 256-262.
- Perez-Pinas I, Sabate J, Carmona A, Catalina-Herrera CJ, Jimenez- CastellaJ (2000) Anatomical variations in the human paranasal sinus region studied by CT. J Anat 197: 221-227.
- Kennedy DW, Zinreich SJ (1988) The functional endoscopic approach to inflammatory sinus disease: current perspective and technique modifications. Am J Rhinol 2: 89-96.
- Lloyd GA, Lund VJ, Scadding GK (1991) CT of the paranasal sinuses and functional endoscopic surgery: a critical analysis of 100 symptomatic patients. J Laryngol Otol 105: 181-185.
- Yousem DM (1993) Imaging of sinonasal inflammatory disease. Radiology 188: 303-314.
- Earwaker J (1993) Anatomic variants in sinonasal CT. Radiographics 13: 381-415.
- Wanamaker HH (1996) Role of Haller's cell in headache and sinus disease: a case report. Otolaryngol Head Neck Surg 114: 324-327.
- Tonai A, Baba S (1996) Anatomic variations of the bone in sino nasal CT. Acta Otolaryngol 525: 9-13.
- Zinreich SJ, Albayaram S, Benson ML, Oliverio PJ (2003) The ostiomeatal complex and functional endo-scopic surgery. In: Som PM, Curtin HD, editors. Head and neck imaging. 4th ed. Mosby Inc., St Louis, USA, pp. 149-173.
- Elsherif AA and Elsherif A (2006) Some anatomic variations of the paranasal sinuses in patients with chronic sinusitis: A correlative CT study to age and sex. AAMJ 4(3): 1-15.
- Wani AA, Kanotra S, Lateef M, Ahmad R, Qazi SM, et al. (2009) CT scan evaluation of the anatomical variations of the ostiomeatal complex. Indian J Otolaryngol Head Neck Surg 61: 163-168.
- Alkire BC, Bhattacharyya N (2010) An assessment of sinonasal anatomic variants potentially associated with recurrent acute rhinosinusitis. Laryngoscope 120: 631-634.
- Mamatha H, Shamasundar NM, Bharathi MB, Prasanna LC (2010) Variations of ostiomeatal complex and its applied anatomy: a CT scan study. Indian J Sci Technol 3: 904-907.
- Fadda GL, Rosso S, Aversa S, Petrelli A, Ondolo C (2012) Multiparametric statistical correlations between paranasal sinus anatomic variations and chronic rhinosinusitis. Acta Otorhinolaryngol Ital 32: 244-255.
- Al-Abri R, Bhargava D, Al-Bassam W, Al-Badaai Y, Sawhney S (2014) Clinically significant anatomical variants of the paranasal sinuses. Oman Med J 29: 110-113.
- Khojastepour L, Mirhadi S and Mesbahi SA (2015) Anatomical Variations of Ostiomeatal Complex in CBCT of patients Seeking Rhinoplasty. J Dent Shiraz Univ Med Sci 16(1): 42-48.
- Sebrechts H, Vlaminck S, Casselman J (2000) Orbital edema resulting from Haller cell pathology: 3 case reports and review of literature. Acta Otorhinolaryngol Belg 54: 39-43.





























