A Rare Case of Kicukhi - Fujimoto Disease Histiocytic Necrotizing Lymphadenitis- Case Report
Cristina Otilia Laza1*, Aftenie Cristian1, Laura Axinte1 and Luminita Micu2
1ENT/OMF Clinic, Europe
2Department of Anatomopathology, Europe
Submission: July 29, 2017; Published: August 09, 2017
*Corresponding author: Cristina Otilia Laza, ENT/OMF Clinic, SF Apostol Andrei, Constanta, Romania, Europe, Email: cristinaotilia@gmail.com
How to cite this article: Cristina Otilia Laza. A Rare Case of Kicukhi - Fujimoto Disease Histiocytic Necrotizing Lymphadenitis- Case Report. Glob J Oto 2017; 9(4): 555769. DOI: 10.19080/GJO.2017.09.555769
Abstract
We present a case of a 38-year-old men who was admitted in our clinic for multiple laterocervical bilateral masses with debut 3 weeks earlier, with fever, malaise. He describe a common cold at the beginning than, he accuse odynophagia and observe bilateral subangulomandibular masses. The lymph nodes continue to enlarge and more others appear day by day, even after a 5 days course of Claritromicine, and another 5 day with iv Ampiciline plus sulbactam and Gentamicine. In the clinic after lab test and imagistic we decide for an excisional biopsies of the cervical lymph nodes under general anesthesia The clinical aspect and CT scan /MRI was like an aggressive lymphoma . But morphologic and immunophenotypic findings were suggestive for Kikuchi Fujimoto disease (KFD). After the surgery his status improved day by day, till the final results were available our patient was free of lymph nodes, with normal lab test and feeling great.
Keywords: Lymphadenopathy; Necrotizing adenitis; Histiocitosis
Introduction
Cervical lymphadenopathy in a young adult can be caused by a lot of causes from viruses like HIV primary infection, EBV -Mononucleosis, Adeno-pharyngo-conjunctival virus or bacterial, parazitic or its part of leukemia or a lymphoma. One of the rarest causes is Kikuchi-Fujimoto disease -or histiocytic necrotizing lymphadenitis, a benign, and self-limited syndrome of unknown etiology. Typically is characterized by tender localized lymph- adenopathy, constitutional symptoms such as fever and night sweats. KFD patients are mostly young asian females, around 30 years age. Diagnosis is confirmed histopathologically. It is generally a self-limited disease that regresses spontaneously without any specific therapy. It is an under diagnosed condition with an excellent prognosis, making it imperative that it is differentiated from a malignant lymphoma. The awareness of this condition amongst clinicians and pathologists might help prevent misdiagnosis and inappropriate treatment.
Case Report
We present a young man 38 years old, who was admitted in our clinic for bilateral enlargement of the neck by later cervical lymphadenopathies. 3 weeks ago the illness starts suddenly with malaise, low fever, fatigue, pain in muscles of the limbs and neck. In anamnesis he didn’t have chronic diseases just an intermittent gastro-esophageal reflux, he quit smoking about a year ago, work as a cook. He reported than the treatments, and diagnosis, doctors who consult him. So first was diagnosed with Acute catarrhal pharyngitis with adenitis and 5 days was treated with-Claritromicine SR 500mg/day, AINS, antiseptics for the throat but the lymph nodes continue to enlarge and more others appear day by day. He start an IV course of Ampicillin -plus sulbactam and but with the same effect. In the clinic after lab test and imagistic we decide for an excisional biopsies of the cervical lymph nodes under general anesthesia (Figure 1).

a. Physical examination revealed and well-built young man now asthenic but oriented in time and space, with general status affected, fever 38,2 grade C .
b. Inspection and palpation -enlargement of the neck bilateral laterocervical like, proconsular neck in lymphoma .The masses were lymph nodes enlarged along the entire bilateral jugulocarotidian chains and spinal chains so levels I,III,III,IV and V ..The lymph nodes were non painfull, flexible mobile, ovular no more than 5 cm in diameter and nonfluctuant. The mouth and pharynx have different type of Candidiasis,also signs of reflux-the patient blame heart burn after Clarytromicine. There were no other lymph nodes palpable -in axilla or inghinal, no hepato or splenomegaly, no scleral icterus, or ecchymosis on the skin or petechias clinically signs of trombopenia.
c. Laboratory studies:
I. CBC- leucopenia with a total leucocyte count of 2600/μL and an ANC (absolute neutrophil count) of 500/μL, anemia, with hemoglobin of 12.6 g/dL
II. alanine aminotransferase - 116U/L and aspartate aminotransferase of 64U/L
III. PCR, fibrinogen high levels
IV. HIV 1, 2 negative
V. Ac EBV negative
VI. Ac Toxoplasma, toxocara -negative
VII. Ag HBS, Ac HBC -negative
VIII. RBW, VDRL
XI. Quantiferon test
X. Antinuclear antibody (ANA),
XI. Rheumatoid factor (RF),
XII. Anti-DNA antibodies were negative.
XIII . Complement levels normal limits.
d. Imagistic studies
i. Chest X-ray was normal
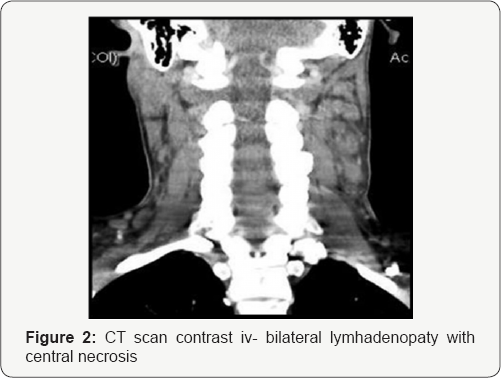
ii. CT scan with contrast iv of neck revealed symmetric lymphadenopathy in the neck involving lymph nodes on both posterior triangles (size max 3,.8 cm), bilateral entire internal jugular chains (size max5,.5 cm), nothing abnormal in the pharynx
iii. MRI-contrast showed mixed density of the masses suggestive for a central necrotic process.
vi. The clinical aspects, imagistic were of an aggressive lymphoma (Figure 2).
That's why we decide to perform under general anesthesia an excisional biopsy of lymph node. Histopathological exam and IHC established the diagnosis of KICUCHI FUJIMOTO disease showed reactive follicles, an expanded parafollicular area with clusters of large immunoblast-like cells, and histiocytes. Multiple areas showed necrotic foci with apoptotic debris but no granulocytes. Immunohistochemical staining showed showed CD3 positive T lymphocytes and CD20 positive B lymphocytes within the par cortical areas.
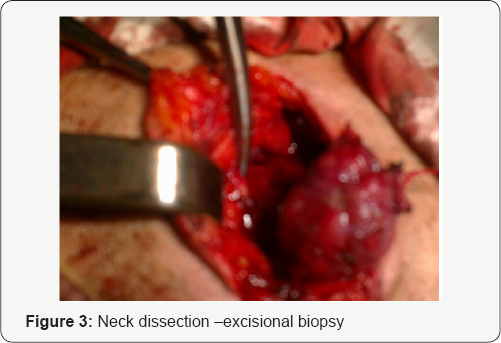
Remnants of residual follicular dendritic cell and increased plasmacytoid dendritic cells were also found within the follicles. These morphologic and immunophenotypic findings were suggestive of Kikuchi Fujimoto disease (Figure 3). After the surgery, the patient was healing quickly, progressive the rest of the lymph nodes tends to disappear without a specific treatment, the general status improve, and on the other side the lab test shows CBC- leucopoenia was replaced by a normal number of leucocytes, neutrophils level became also in limits. Till the anatomo-pathological and IHC results were available our patient was already healed without lymph nodes, no fever, good status. He was called for follow-up every month in the first year, at 2-3 month in the second year but no recurrence till now.
Discussion
Kikuchi-Fujimoto disease or histiocytic necrotizing lymphadenitis, is a rare, idiopathic, usually self-limited disease characterized by cervical lymphadenopathy and general symptoms Kikuchi and Fujimoto independently, as "a lymphadenitis with focal proliferation of reticular cells accompanied by numerous histiocytes and extensive nuclear debris." The incidence of KFD is unknown. The typical patient is a young Asian female. The prevalence of Kikuchi disease among patients with lymphadenopathy ranges between 0.5% in Saudi Arabia and 34,7% in Korea, with female to male ratio ranging from 1.26:1 to 1:4. It typically occurs in patients during third and fourth decade of life. This geographic predominance may be related to the presence of certain HLA alleles such as HLA class II alleles, HLA-DPA1 and HLA-DPB1, which are more prevalent in Asian KFD patients, are extremely rare or absent among Caucasians .Although more prevalent in Asia, KFD has been observed in patients of all ages, genders, and races It can involve both nodal and extranodal locations. The pathogenesis of Kikuchi disease is unknown; infectious and autoimmune etiologies have been proposed.
The clinical course and histology revealed an immune response of cytotoxic T cells and histiocytes to an unidentified infectious agent. Infectious agents such as:
- Yersinia enterocolitica,
- Brucella,
- Bartonella henselae,
- Entamoeba histolytica,
- Mycobacterium szulgai,
- Toxoplasma gondii were implicated but subsequent studies failed to support these findings .
Viruses such as
- Epstein-Barr virus,
- herpes virus,
- cytomegalovirus,
- parvovirus,
- paramyxovirus,
- parainfluenza virus,
- Rubella,
- hepatitis-B,
- human immunodeficiency virus (HIV),
- human T-lymphotropic virus type-1 (HTLV-1), and the
- Dengue virus have all been suggested as probable etiologies of KFD, but never convincingly demonstrated.
- On the other hand, some authors hypothesized that KFD may reflect a self-limited autoimmune condition induced by virus-infected transformed lymphocytes
- Kikuchi disease has similar histologic features with SLE. In addition, both diseases share gender and age distribution.
This is because, histo-pathologically, findings of tubule- reticular structures in the lymphocytes and the endothelial cells in patients with SLE are similar to those found in patients with KFD. The onset of KFD could be acute or subacute, evolving over two to three weeks. And can have nodal and extranodal involvement. The most common presentation is acute cervical lymphadenopathy typically unilateral, with cervical involvement in 70% to 98% of cases. Most frequent jugular lymph nodes and posterior cervical chain are involved but any lymph node region can be involved including the axillary (14%) and supraclavicular (12%) nodal chains, or can be a generalized lymphadenopathy
a) low-grade fever and flu-like prodromal
b) fatigue and
c) weight loss
d) sore throat
e) night sweats
f) joint pain was reported in 7% of the cases,
g) skin rash (10%), maculopapular, morbilliform,urticarial or disseminated erythema
h. hepatosplenomegaly,
a. Physical examination general status, temperature, pale skin, or sweat, warm and red. Inspection and palpation -must consider all the lymph nodes chains including axillary and inguinal. Usually the lymph nodes are ovalar, nontender most of the time , they never suppurate. On palpation are ferms and nonfluctuants ENT ex
- Anterior rhinoscopy
- Posterior rhinoscopy
- Bucopharyngoscopy
- Indirect laryngoscopy
- Flexible naso-pharyngo-laryngoscopy.
Examination of the skin for rush or ecchymosis on the skin or petechial lesions signs of leukemia eye exam - scleral icter Palpation of the abdomen for hepatomegaly, splenomegaly
b. Laboratory studies
- CBC- leucopenia with granulocytopenia, atypical lymphocytes, anaemia
- PCR, LDH
- AST, ALT, GGT,
- IDR at PPD, Quantiferon test.
- sputum, cultures
- Ac anti EBV Ig A, M, G
- Ac anti Toxoplasma, Toxocara
- HIV 1,2
- Ag HBS, Ac HBC
- Kweim test
- RBW-/VDRL
- Antinuclear antibody (ANA),
- rheumatoid factor (RF),
- Anti-DNA antibody was negative.
- Complement levels normal limits
- Imagistic studies
- RX thorax -look for tuberculosis; sarcoidosis lymph nodes in the mediastinum, malignancy, or other possible disease are reasonable.
- CT contrast neck
- MRI neck
This disorder does not have a characteristic radiological appearance [1-4]. The findings of CT and MRI (magnetic resonance imaging) in KFD can be variable and mimic not only lymphoma but more other nodal diseases with necrosis such as metastasis and tuberculosis. Kikuchi disease is definitive diagnosed by excisional lymph node biopsy-histological exam. The histology of the lymph node typically follows three phases:
a) proliferative phase with folliwlar hyperplasia and paracortical expansion of lymphocytes (B and T), monocytes, and histiocytes; followed by a
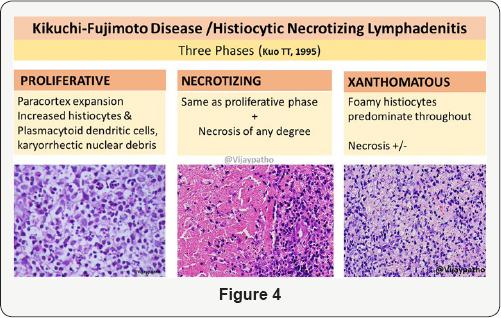
- necrotizing phase that shows extensive necrosis with distorted lymph node architecture without neutrophilic infiltrate and with histiocytes dominance; and the
- last phase, the xanthomatous phase or foamy cell phase, with the resolution of necrosis
b) Immunohistochemical staining showed
- CD3 positive T lymphocytes and
- CD20 positive B lymphocytes within the paracortical areas (Figure 4).
c. Differential diagnosis
- Non Hodgkin lymphoma,
- Systemic Lupus Eritematous
- Hodgkin lymphoma,
- Toxoplasmosis,
- Metastasis from an epidermoid carcinoma of the pharynx, larynx etc,
- Infectious Mononucleosis,
- AIDS - acquired immunodeficiency syndrome,
- Benign lymphoreticulosis-cat-scratch disease, and
- Myeloproliferative syndrome- lymphadenopathy
Kikuchi-Fujimoto disease is typically a self-limited disease that rarely requires specific treatment and resolves within one to four months. The course of cervical lymphadenopathy is benign and resolves spontaneously. However, a recurrence is possible in 3-4% of cases. No hereditary risk has been documented in KFD. Few cases of complication from heart failure, infection, meningitis and macrophage activation syndrome have been reported, a few deaths. The treatment is mainly supportive including analgesics (NSAIDs) and antipyretics to alleviate lymph node tenderness and fever [5-11]. Corticosteroids, Immunoglobulins, and hydroxychloroquine have been used in recurrent or severe forms of disease with neurological extranodal involvement. Patients diagnosed with KFD and positive laboratory test results for SLE and later developed clinically SLE. It this case is recommended o long -term follow up, with periodic repeated lab test for SLE. ANA, rheumatoid factor, and anti-ds DNA were negative in our patient .After surgery he was better and better day by day, lymph nodes decreased in size progressive, without a specific treatment.
Conclusion
- Cervical lymphadenopaties may be caused by a lots of bacteria, viruses, parasitis but can be a lymphoma, leukemia or metastazis
- Also very rare in our region KICUKHI-FUJIMOTO disease or histocitic necrotizing lymphadenitis must be included in differential diagnosis of a polyadenopaty with central necrosis.
- In our patient the aspect was 99% of an aggressive non Hodgkin lymphoma like Burkitt,
- Excisional biopsy with histopathological exam and IHC staines are the ones capable for the real diagnosis because prognosis and treatments are completely different
- We consider the presentation of our patient with such a rare disease in our area but also in men, necessary to be known by specialists and pathologist and include in differential diagnosis of lymphadenopathies on the neck with necrosis
- Our patient had transaminitis and granulocytopenia with neutropenia that improved as the size of lymph nodes decreased. This gives an insight into the natural course of the disease.
- No recurrence appear in 2 years of follow -up-now at 6 month
- KFD is a benign, self-limited, condition with an excellent prognosis. Probably is under diagnosed.
- Unfortunately, the etiologies, pathogenesis, still remain enigmatic and further research is required to answer these questions.
References
- Bosch A Guilabert (2004) Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. The American Journal of Clinical Pathology 122(1): 141-152.
- A Parappil, E Pathan, SK Surrun (2004) Pyrexia of unknown origin: Kikuchi-Fujimoto disease. Clinical Infectious Diseases 39(1): 138-143.
- A Lim, W Issing (2012) Kikuchi-Fujimoto disease: a case report and literature review. Case Reports in Otolaryngology.
- DF Scully, C Walsh, D Kane (2013) Kikuchi-Fujimoto disease-an unusual mimicker? New Zealand Medical Journal 126(1383): 85-88.
- MJ Bennie, KM Bowles, SC Rankin (2003) Necrotizing cervical lymphadenopathy caused by Kikuchi-Fujimoto disease. The British Journal of Radiology 76(909): 656-658.
- SY Kwon, TK Kim, YS Kim, KY Lee, NJ Lee, et al. (2004) CT findings in Kikuchi disease: analysis of 96 cases. The American Journal of Neuroradiology 25(6): 1099-1102.
- ARA Amir, SS Amr, SS Sheikh (2002) Kikuchi-Fujimoto's disease: report of familial occurrence in two human leucocyte antigen-identical nontwin sisters. Journal of Internal Medicine 252(1): 79-83.
- RF Dorfman (1987) Histiocytic necrotizing lymphadenitis of Kikuchi Fujimoto. Archives of Pathology and Laboratory Medicine 111(11): 1026-1029.
- K Rezai, S Kuchipudi, VJ Loew, BE Sha (2004) Kikuchi-Fujimoto disease: hydroxychloroquine as a treatment. Clinical Infectious Diseases 39(12): 124-126.
- M Noursadeghi, G Pasvol (2006) Successful treatment of severe Kikuchi's disease with intravenous immunoglobulin. Rheumatology 45(2): 235-237.
- K Takada, K Suzuki (2001) Immediate remission obtained by minocycline in a patient with histiocytic necrotizing lymphadenitis. Internal Medicine 40(10): 1055-1058.





























