Diagnosis and Treatment of Carotid Body Tumor-Case Report
Cristina Otilia Laza1, George Mincu1, Radu Baz2, Adrian Traian Creanga3, Marius Militaru4 and Anca Hancu5
1ENT surgeon, University Ovidius, Europe
2Radiodiagnosis and imagistic, Europe
3OMF surgeon, Europe
4C-Vsurgeon, Europe
5Neurology, Europe
Submission: July 08, 2017; Published: July 20, 2017
*Corresponding author: Cristina Otilia Laza, ent/omf clinic-scju constanta, University Ovidius, Constanta -B-Dul Tomis 145, Europe,Email: cristinaotilia@gmail.com
How to cite this article: Cristina O L, George M, Radu B, Adrian T C, Marius M, et al. Diagnosis and Treatment of Carotid Body Tumor-Case Reports. Glob J Oto 2017; 9(1): 555753. DOI: 10.19080/GJO.2017.09.555753
Abstract
Carotid body tumors are rare benign tumors of the neck but dangerous because their vascular nature and position between Internal and External carotid arteries quite sitting on the carotid bifurcation. Carotid body tumours are paragangliomas, tumors, originating from paraganglionic bodies of autonomous nerve system of the embriological neural crest and increasing gradually. Despite their gradual developing nature, slow and painless it is critical to reach early diagnosis and tailor surgical plan for carotid body tumors due to their potential of being malignant and local aggressive development, with invasion of the essential vessel like ICA or compression neural tissues-last 4 cranial nerves.
Optimal management of cervical paragangliomas should include a thorough preoperative evaluation, accurate definition of the surgical anatomy, and exclusion of synchronous paragangliomas. A combined therapeutic approach by a multidisciplinary team including surgeons and interventional radiologists provides safe and effective management of cervical paragangliomas with very low morbidity and excellent outcomes. In this article, we present a case of carotid body tumor and importance of team effort to obtain the best informations, imaging, for the best surgical results also seen as common effort -always a team-ENT, vascular surgeon, interventional radiologist and maxilla, complications, and follow-up.
Keywords: Carotid Body Tumor; Paraganglioma; Angiography; Angio CT; Angiography; Embolization; Radiotherapy
Abbreviations: CBTs: Carotid Body Tumors; COPD: Chronic Obstructive Pulmonary Disease; PG: Paraganglioma; VMA: Vanillyl-Mandelic Acid; CBTs: Carotid Body Tumors; CTA: Computed Tomography Angiography; DSA: Digital Subtraction Angiography; MIBG: Metaiodobenzylguanidine
Case Report
We present a case of a 46 years old lady presenting with a left laterocervical mass located below the angle of the mandible, at the anterior border of the sternocleido-mastoid muscle, with normal skin covering the mass. The tumor located at the anterior border of SCM, ovalar, with maximum diameter of 4-4,5 cm. It was not visible pulsatile but on palpation the mass was elastic but irregular and pulsation were important, also it was not so mobile like a branchial cyst because was fixed in a vertical line. Our lady on anamnesis recognize that the mass is old - more than 10 years and because most of the doctors appreciate that is a benign branchial cyst, the single risk being just infection, he postpone as much as she can .In the last month she observe suddenly what is growing faster and she fell pulsation on is lying on left side also accuse a discomfort on deglutition [1].
We admit the patient in our clinic, and thinking of a vascular mass first I inspect the bucopharynx because glomus jugularae if his descent in the parapharyngeal retrostilian space is visible behind the posterior pillar like a pulsatile mass, but the pharynx was clean also mobility of the tongue, soft palate, deglutition and position of the vocal cords [2]. Otoscopy microscope-endoscope -there were no symptoms like deafness or pulsatile tinnitus - a normal ,mobile eardrum with a bluish inferior mass inferior inside -but after immitance audiometry no sign of glomus tympanicum were found (Figure 1).
Laboratory Test
a. CBC, inflammatory nonspecific test like PCR
b. Metabolic balance, hepatic and renal functions
c. Also we dose urinary vanil-mandelic acid, urinary cathecolamines
d. EKG -cardiologic exam
a. Imagistic
i. X-ray lung.
ii. Echography of the neck to reveal the cystic or solid structure of the mass, no lymph nodes were discovered also normal salivary and thyroid glands.
iii. Echo Doppler reveals the vascular nature of the mass.
iv. An angio CT scan with spiral enhance and 3D reconstruction was perfect for the diagnosis and plan for the surgery-is clear presence of a vascular tumor located between the ICA and ECA sitting on the carotid bifurcation [3] (Figure 2).

We also insist for an AngioMRI to locate exactly the superior limit, hoping that was not yet in the foramen jugularae. We ask a cardiovascular surgeon to consult our patient and he confirm the presence of a carotid body tumor, and he conclude that is small, only there are problems we can call for him [4]. Also because in the parapharyngeal space is so difficult to operate especially in this case when is so important to control the large vessels, we invite an OMF surgeon to assist us in case that a mandibulotomy will be necessary.
After consulting of an ATI doctor we were prepared with all, including lots of units of blood in case of haemoragy. Under general anesthesia we use a cervicotomy along the anterior margin of SCM, and step by step we isolate the large vessels, carotid bifurcations and we succeed to dissect in an periadventicial plane and isolate the ICA, but we ligate some branches of the ECA, and finally we remove the entire tumor without mandibulotomy or haemoragy or damage of a nerve. We consider that we can classify our tumor in type 2 Shamblin [5]. The evolution was normal, no complaining, no nerves damaged, no neurological complication; the scar was clean and linear.
Anatomophatology
The carotid body tumor was reddish-brown, oval structure, located if is normal on the posteromedial aspect of the carotid artery bifurcation, but now on the bifurcation quite same times invading also the ICA, ECA. The healthy gland measures 3-5 mm in diameter and weighs less than 15 mg on average, but our tumor was large 4,6 cm larger diameter and 3 cm small one [6]. The tumor was located within the periadventitial tissue so the dissection was possible respecting this plane, without damages of vessel or nerves.
The gland is highly vascular and receives its blood supply from feeder vessels running through the Mayer ligaments, primarily from the external carotid artery, typically the ascending pharyngeal artery. It is innervated by the hearing nerve, originating from the glossopharyngeal nerve about 1.5 cm distal to the jugular foramen. We discharge the patient with all the instructions necessary and we establish a follow-up program-starting with the first at 2 weeks [7]. Unfortunately at two weeks before the surgery the scar seams to became a keloid and also she accuse, numbness on hemi tongue, dysphonia and dysphagia .We examine the patients and we discovered that the last 4 cranial nerves are compress with incomplete palsy of the hemi tongue, soft palate, also pharynx and left vocal cords. We order an MRI but nothing was abnormal, so we transfer our patient to neurology department also was in attention of a plastic surgeon.
But even now the scar is nice the nerves were irremediably damaged so our patient complains of rhinolalia, liquids returning through the nose and dysphagia, dysphonia and even aspiration. The left valecula and pyriform sinus were full of saliva [8]. So my only choice was to start with her exercises to learn to swallow first foods moist but sticky like banana, soft cheese, than to use a position of the head more favorable for deglutition, to use a straw for the liquids, to use supraglotic swallowing, and at the end to swallow repeatedly to remove the rest of foods from the hypo pharynx, so step by step and with some phoniatric exercises she is much better without incompetence of the soft palate, just dysphonia but only if she talk too much ,and dysphagia sometimes for meat.
Every year we repeat an AngioCT but till now there is no recurrence, so after 6 years, we still are disappointed what after such a diagnosis we realize a perfect surgery, without a single problems and in the end we learn that not always depends on you but every patient is unique so like a tailor its important also the material you work on.
Introduction
The carotid body, first described by Van Haller in 1743, is located in the carotid adventitia on the posterior, aspect of the carotid bifurcation and is embryologically, derived from the neuroectodermal tissue of the, amine precursor uptake and the decarboxylation system. Carotid body tumors are rare neoplasms, with an incidence of about 0.012%. Although they represent about 65% of head and neck paragangliomas an incidence of about 0.012%. Although they represent about 65% of head and neck paragangliomas [1]. These tumors develop within the adventitia of the medial aspect of the carotid bifurcation (Figure 3).

Glenner, GG and Grimley PM. Tumors of the Extra-Adrenal Paraganglion System. Bethesda, MD: Armed Forces Institute of Pathology, 1974, Head and Neck. Ten percent of these are familial, and out of this small percentage, 30%are bilateral in nature. Ultimately, bilateral familial are observed in only in 5% of the total number of cases of this type of tumor [9]. Although have been observed in children, they are predominantly found in middle-aged adults, and the average age of onset is 45 years. The etiology of carotid body tumors is unknown, but there is an increased incidence in populations living at high altitudes and in patients with chronic obstructive pulmonary disease (COPD), which has led to the hypothesis that chronic stimulation of the carotid body by hypoxia may predispose certain people to the development of these tumors.
The carotid body serve as un adaptor to fluctuating concentrations of oxygen, carbon dioxide, and pH, protecting the organs from hypoxia by releasing neurotransmitters that increase the ventilatory rate when stimulated, also act on arterial tension.
The following 3 different types of carotid body tumors (CBTs) have been described in the literature:
a. Familial
b. Sporadic
c. Hyperplastic
The sporadic form is the most common type, representing approximately 85% of carotid body tumors. The familial type (10-50%) is more common in younger patients. The hyperplastic form is very common in patients with chronic hypoxia, which includes those patients living at a high altitude (> 5000 feet above sea level), like those patients living in New Mexico, Peru, and Colorado. The hyperplastic form is also seen in patients who have chronic obstructive pulmonary disease or cyanotic heart disease [10].
The familial paraganglioma form is a genetically heterogenous entity; currently, 4 genes are identified. The first 3 genes encode the subunits of the enzyme succinate dehydrogenase complex, which is part of the Kreb's cycle [11]. Paraganglioma (PG) syndrome 1, 3, and 4 occur because of mutations of the corresponding genes of the subunits D, C, and B. PG syndrome 2 gene mutations are yet to be identified. Hereditary paragangliomas result from mutations in the genes for succinate dehydrogenase (SDHD, SDHA, SDHC, SDHB). Defective succinate dehydrogenase has been postulated to cause an increase in the intracellular concentration of molecular hypoxia mediators and the vascular endothelial growth factor (VEGF) thus resulting in hyperplasia, angiogenesis, and neoplasia. Carotid body tumors can be occasionally associated with other syndromes, like MEN type II, von Hippel-Lindau syndrome, and Neurofibromatosis type 1.
Method of Diagnosis
Symptoms
Most of them are silent, but may accuse pain, dysphagia, dysphonia or autonomic dysfunction-myosis, enophtalmia and palpebral ptosis-Claude Bernard sdr, shoulder drop-CN XI, immobile, paralyzed tongue -CN XII with problems like eating and speaking
i. Pheochromocytoma-like symptoms, paroxysmal hypertension, palpitations, and diaphoresis
ii. Fever of unknown origine
Signs
Most commonly carotid body tumor present as an asymptomatic palpable neck mass in the anterior triangle of the neck. They are slow-growing tumors that can remain asymptomatic for many years, Jansen et al estimate using sequential imaging, a median growth rate of 0.83 mm/year. On examination, the mass is typically vertically fixed because of its attachment to the bifurcation of the common carotid (Fontaine sign). A bruit can be felt; also only a part is pulsatile [12]. Vagal body tumors are more cranially located and sometimes project into the lateral pharynx as a pulsatile mass. In large tumors - paralysis of the hypoglossal, glossopharyngeal, recurrent laryngeal, or spinal accessory nerve, or involvement of the sympathetic chain with Horner syndrome, or shoulder drop.
Lab Test
a. Usual test plus,
b. Urinary catecholamines,
c. Vanillyl-mandelic acid (VMA),
d. Metanephrines
Incisional biopsy of carotid body tumors (CBTs) is not indicated and should not be performed except in very unusual cases because may lead to profuse bleeding and/or cranial nerve injuries. Fine-needle aspiration biopsy is helpful only if the diagnosis is unclear via imaging studies.
`Histologic Findings
Carotid body tumors are composed of the following 2 cell types that are arranged in a pseudoalveolar pattern characteristic of paragangliomas known as «cell balls» (zellballen):
i. Type I cells, which are the chief cells that predominate in carotid body tumors (CBTs) and contain catecholamine- bound granules.
ii. Type II cells, which are the sustentacular cells located at the periphery, are devoid of granules.
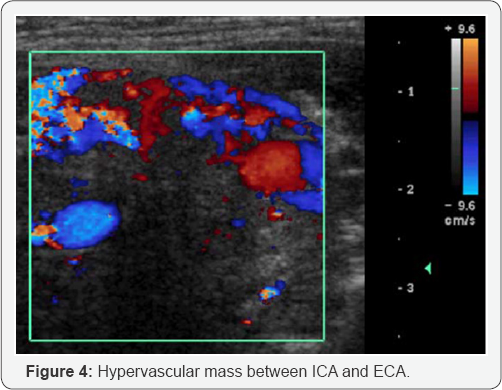
Paragangliomas are classified into noninvasive, locally invasive, and metastatic types. Unfortunately, malignancy cannot be detected by routine histological findings and is only defined when the tumor metastasizes to regional lymph nodes or more distant sites. Nuclear polymorphism, neurovascular invasion, high mitotic indices, and necrosis may be present in both benign and malignant carotid body tumors (CBTs) [13]. Paragangliomas may be initially detected during ultrasound or Doppler ultrasound ofthe neck; however CT and MRI are more sensitive for accurate tumor measurement. 123I-metaiodobenzylguanidine scintigraphy images paraganglioma tumor tissue based on the selective uptake of precursors for catecholamine synthesis, but is most useful in detecting occult paragangliomas or extra adrenal tumors in unusual anatomic sites and is therefore infrequently utilized.
USG: Ultrasonography
Delineates tumor margins, size and location also revealed cystic or solid nature of the mass.
ECHO Doppler
Demonstrates hypervascularity of paragangliomas, surveys neck for other lesions. Differentiates CBTs from vascular anomalies and pseudoaneurysms, can obtain US guided fine needle aspiration (Figure 4).
CT: Computed Tomography
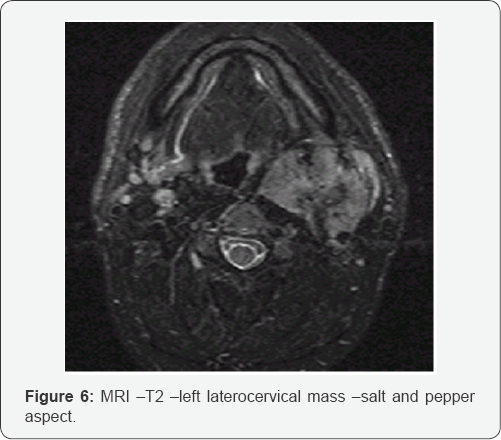
The typical radiologic findings include a hypervascular, hypoechogeniv ic tumor with splaying of the carotid bifurcation Thin section scanning from thoracic inlet to skull base in patients with CB or vagal paragangliomas or other palpable neck mass .Examines integrity of associated soft tissues ,capable to detect multiple lesions , 3D reconstruction visualizes associated vasculature (Figure 5).

Angio CT scan spiral enhanced (Figure 6)
MRA: Magnetic resonance angiography
MRA provides better insight into the vascularity of the tumor and its feeder vessels. However, accurate diagnosis is usually based on angiographic criteria, which show the typical lyre sign.
Aids in lesion diagnosis and localization

a. Differentiates mass from surrounding inflammatory changes, fluid or vascular structures
b. More sensitive for delineating encroachment and encasement of vessels
c. Images middle ear structures and bony erosions
d. Coronal sequences-Noninvasive
e. Delineates displacement of vasculature
f. Demonstrates tumor vascular supply (Figure 7).
CTA: Computed tomography angiography
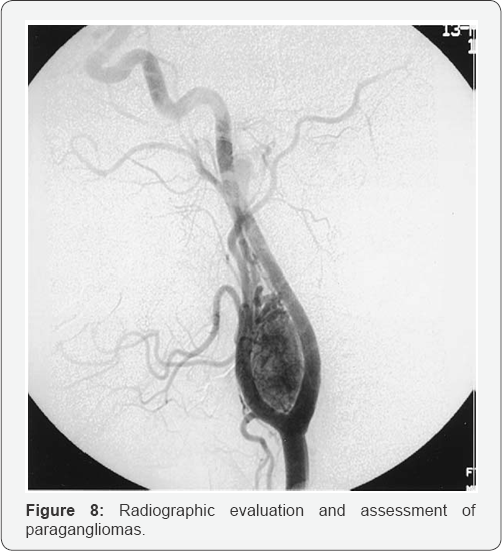
DSA: Digital subtraction angiography
Demonstrates the primary arterial supply and collateral vessels of tumor
a. Reveals relationships with neck blood vessels
b. Angiography is also helpful for better visualization of the feeder vessels and is of utmost importance for high-risk tumors (Shamblin II or III) that need either embolization or a preoperative balloon occlusion test (Figure 8).
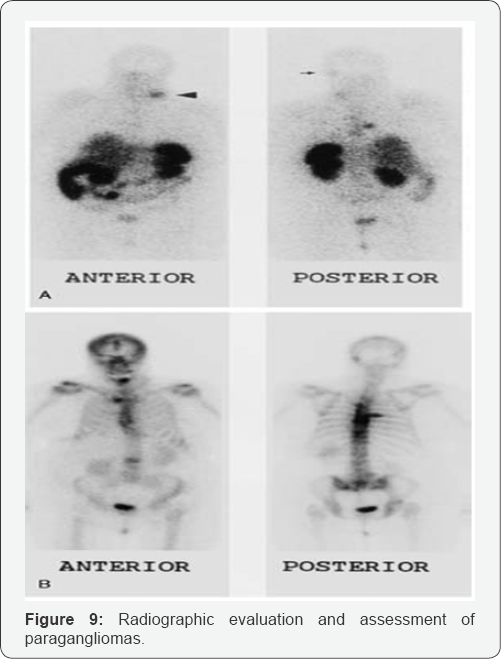
Scintigraphy
Pentetreotide= octreotide radiolabelled with 111 indium- DTPA binds somatostatin type 2 receptors in paragangliomas. Uses: follow recurrent disease, locates multiple lesions, detects familial paragangliomas (Figure 9).
In patients who are suspected to have multiple small tumors, such as those with familial carotid body tumors (CBTs), performing a physical examination and supplementing it with imaging studies (including a CT, MRI, or metaiodobenzylguanidine [MIBG] scintigraphy) is essential. MIBG scans are quicker to perform than MRI and are also used in patients who are claustrophobic [14,15]. The only issue with this scan is that it can only be used in patients who have functional tumors. In cases in which the tumor is nonfunctional, a better test is a pentetreotide scan, which uses a radiolabeled somatostatin analogue.
Staging
Shamblin classification of carotid body tumors stages
i. Type I - small tumor that is easily dissected in a periadventitial plane.
ii. Type II tumors are larger and more adherent and partially surround the vessel required ECA resection
iii. Type III tumors completely surround the carotid bifurcation plus reconstruction of ICA.
Methods of Treatment
Surgical Therapy
Descriptions of surgery for carotid body tumors have existed for over 100 years. The early reports described significant complications, particularly mortalities secondary to intraoperative bleeding. In the United States, the earliest successful carotid body tumor resection was performed by Scudder in 1903. Even into the middle of the 20th century, resecting these tumors remained a problem because of the complications; In 1940, Gordon-Taylor showed a safe sub adventitial plane of tumor dissection. However, when dealing with large carotid body tumors, ligation of the carotid artery was necessary for resection at that time, and mortality approached 50% in those who survived .Hayes Martin, in his textbook of head and neck tumors, recommended against resection of any tumor that is now considered a Shamblin type III.
Modern imaging and current surgical and vascular techniques have significantly improved the safety and success of this operation. Carotid body tumors (CBTs) are treated with either surgery or radiotherapy. When choosing treatment, consider the following factors: presence of other paragangliomas, malignant mass, bilateral carotid body tumors, or recurrent, the age and the health of the patient, and very important is what prefer our patient [16-18].
Also a larger than 5 cm in Shamblin classification ,the vascular resection and reconstruction are dangerous ,high risk of stroke, and other complication is safer to use as a treatment radiation therapy. Preoperative evaluation is extremely important to avoid major surgical complications. The use of MRI and genetic testing in susceptible families have allowed earlier detection of multicentric tumors in many patients. Operative risk is directly related to the size and extent of the tumor. Preoperative embolization is still controversial, although it has been used to decrease the risk of intraoperative bleeding, particularly in larger tumors [19].
Radiotherapy as a primary modality of treatment for carotid body tumors has also been heavily debated because some investigators have found that these tumors are not radiosensitive and have reported regrowth after suppression. The tumors that are treated primarily with radiation are also difficult to resect afterwards because of radiation-induced fibrosis, and difficult healing of radiated tissues. Other investigators have reported no cure rates for patients who received radiation for their carotid body tumors. The primary goal of radiotherapy is to slow the progression acting on the large vessels finally with fibrosis. For these reasons, surgery is usually the treatment modality of choice for younger, healthier patients with carotid body tumors (CBTs), and radiotherapy is reserved for the elderly, patients who are poor surgical candidates, and selected individuals with multiple paragangliomas in whom resection may be highly morbid.
Preoperative Details
Carotid balloon test occlusion is performed in patients who are at a high risk of carotid resection due to the tumor's involvement [20]. In such cases, consultation with a vascular surgeon and a neurologist for intraoperative EEG monitoring may be necessary. Discus with your patient, about the risks and possible postoperative complications as cranial nerve injuries (IX, X, XI, XII), bleeding, infection, the possibility of a carotid bypass or vein grafts, stroke, and death. Embolization of carotid body tumors has been a controversial topic. It has been recommended by some surgeons when the size of the tumor exceeds 4 cm in size. Blood loss appears to be less with prior embolization of larger tumors, but other studies appreciate that where is no difference in amount of blood loss with or without embolization. In our hospital arteriography and embolization are not available.
Effective communication between the surgeon and the anesthesiologist is very important most of the surgeons prefer on general anesthesia with controlled hypotension, to reduce hemorrhage most importance throughout the surgery [21,22]. Whether the patient is totally relaxed is the surgeon's preference. Different types of neck incisions have been described. T- A horizontal incision in the mid neck affords excellent exposure both superiorly and inferiorly and typically provides excellent cosmesis. Some surgeons prefer an endarterectomy approach using a transverse cervical incision along the anterior border of the sternocleidomastoid. For larger tumors, many incisions have been described, including -preauricular extension of the incision for tumors extending to the infratemporal fossa (Figure 10).

The most important step in tumor removal is superior and inferior control of the blood vessels. This includes identification of the internal jugular vein, common, and internal carotid arteries and placing vessel loops on each, all the branches of the ECA, including the artery. Hypoglossal and vagus nerve, these nerves should be exposed and followed cranially ,also accessory and glossopharyngeal nerve it is possible are dissected and push away from the tumor but almost in all cases the digastric muscle must be sacrificed for better exposure.
The small feeder vessels, together with some branches from the external carotid artery, are ligated. Dissection between the external and internal carotid artery exposes the larger feeding vessels, including the ascending pharyngeal artery, which is the main feeding vessel most of the time. Dissection of the carotid body tumor is performed in the sub adventitial plane using either loupes or microscope, as described by Gordon-Taylor [23]. This is supplemented with the use of bipolar cautery, which limits blood loss and controls bleeding.
Any injury to the carotid vessel requiring clamping of the common or internal arteries needs temporary heparinization with a low risk of complications; this is often followed by vascular reconstruction. Van der Mey reported that 65% of patients who had their internal carotid artery ligated had a stroke and that 25% of patients who passed their balloon occlusion test had a delayed stroke [24]. During removal of the carotid body tumor, care should be taken once again to avoid injuring the nerves, especially the superior laryngeal nerve, which has been reported to be the most injured nerve during dissection.
Postoperative Details
In the immediate postoperative period, the patient should be carefully observed for any complication of the procedure, including postoperative hemorrhage or late stroke. In patients who underwent vascular reconstruction, ICU admission is recommended, along with heparinization [25].
Follow-up
Patients should be closely observed for any local recurrence, although these are usually rare. If the patient has no morbidity from the initial surgery, contra lateral tumors should also be resected. In patients with significant permanent morbidities to cranial nerves, radiation to the contra lateral side might be considered. As always, a careful weighing of pros and cons must be done and presented to the patient. Operating on small tumors has a very low rate of complications and the long-term effects of radiation on younger patients is potentially a contraindication.
Complications
CN X- The most commonly injured nerve is the superior laryngeal nerve. This nerve supplies the cricothyroid muscle and provides sensation to the supraglottic larynx. The patient postoperatively might suffer from some degree of aspiration and voice changes (inability to create high-pitched sounds). CN X Injury to the vagus - nerve results in vocal cord paralysis with resultant hoarseness and increased aspiration risk. When combined with a superior nerve paralysis, as is the case with a high vagal injury, aspiration is a significant problem because the larynx not only does not function well but is also anesthetic. This may be compensated by the contra lateral vocal cord over time. If the problem persisted, then vocal cord medialization procedures should be performed.
a. CN XII -Speech and swallowing problems result from a hypoglossal nerve injury. If the nerve is accidentally cut, primary reanastomosis should be attempted first. If primary anastomosis fails, then other options include a greater auricular nerve graft.
b. CN XI accessory Postoperative shoulder pain and weakness is typically a result of an accessory nerve injury This results in significant disability for the patient.
c. CN simpatetic-sdr Claude Bernard Horner -myosis, enophtalmia palpebral ptosis.
First bite syndrome is another complication that occurs when the sympathetic supply to the ipsilateral parotid gland is severed. The resultant parotid gland has an unabated parasympathetic supply. To date, no successful treatment of this syndrome exists. Loss of the bilateral Hering nerves, patients experience labile blood pressure postoperatively, which is difficult to control medically. Concurrent excision of bilateral carotid body tumors should, therefore, be avoided, although staging the surgeries might help
i. Hemorrhage caused by rupture of a large vessel.
ii. Stroke in case of clamping the ICA or primitive CA.
In patients requiring arterial reconstruction following CBT resection, is useful an autogenous venous. Interposition if an end- to-end arterial anastomosis is not feasible. But other patients required arterial reconstruction with polytetrafluoroethylene graft/hybrid stent, we elected to keep the patient on dual antiplatelet therapy indefinitely given the limited data on such reconstructions. Postoperative care included close pharmacologic control of systolic blood pressure and postoperative, clinical neurologic evaluation. Patients with a known diagnosis of hereditary paraganglioma should undergo annual biochemical and clinical screening, testing for plasma and/or urinary catecholamines should begin at age of 10. Periodic imaging with CT/MRI or 123I-metaiodobenzylguanidine is indicated for surveillance in patients with a known SDH mutation and in patients with the development of symptoms or if the fractionated metanephrines and/or catecholamines become elevated.
After resection of a CBT, patients should continue to have lifelong biochemical and clinical surveillance. Although no clear consensus has been developed regarding when, how, and how often biochemical studies and imaging should be performed, testing should be individualized to the patient (Figure 11). So in conclusion after complete preoperative evaluation should be performed in patients with a known or suspected cervical paraganglioma, including a directed family history and genetic testing when appropriate and after appreciation of the Shamblin type it's clear that the best treatment is complete surgical resection. Embolisation can be useful in type 2 and 3 Shamblin. Also use the inflate balloon in the ICA for any neurologic changes, and the balloon is deflated if necessary. If no changes are detected, the blood pressure is dropped to simulate mild hypotension (systolic blood pressure 90-100) and verify that the patient still has no symptoms. If the patient passes the test, then the patient will tolerate internal carotid artery ligation without reconstruction but with high risk of stroke especially in older patients, that why an real team including a vascular surgeon must be included. Radiotherapy is not curative just reduce the tumor and prevent rapid development but surgery after radiation is very difficult because of fibrosis induced by radiation, but also post operation there is a long, very slow process of healing, sometimes with dehiscence of wounds, necrosis of tissues even of a large vessel.

Conclusion
- Carotid body tumors are uncommon entities, and their surgical management is technically challenging.
- As gradually increasing numbers of medical centers have surgeons capable of managing these tumors, there has been a decrease in the large number of cases referred to specialized centers.
- Carotid body tumors are found in both sides of the neck and both genders at the same rate of frequency, and they belong to a group of tumors called paragangliomas that can be found at many locations in the body.
- Multicentricity of paragangliomas can occur in up to 25% of patients with carotid body tumor .
- Locally invasive growth of these tumors subsequently leads to cranial nerve deficits along with compression symptoms like Horner's syndrome, syncope, hoarseness and dysphagia.[Cranial nerve deficits, particularly in the cranial nerves VII, IX, X, XI, or XII, can be seen in tumors that reach 5 cm in size.
- For the diagnosis of carotid body tumor, color Doppler USG is the first non-invasive procedure which allows to see that is vascular discrimination between the solid and cystic nature of the carotid body, parts of the tumors with and its relationship with the carotid artery bifurcation
- The gold standard for diagnosis is carotid angiography, which serves both diagnostic and treatment purposes.
- Differential diagnosis of CBTs,
- Branchial cysts,
- Laryngocele external or mixt,
- Phlebectasia of the Jugular Internal Vein or thrombosis /thromboflebitis,
- Tumors of the parotid salivary gland,
- Aneurysm /Pseudo aneurysm of carotid artery, ectasia,
- Lateral aberrant glandulae thyroideae,
- Lymphoma malignant Hodgkin or nonHodgkin,
- Neurofibroma, neuroblastoma, paraganglioma on the cranial nerves (IX,X,XIX,XII and sympathetic chain,
- Lymphadenitis, -bacterial or tuberculous,
- Metastasis of epidermoid carcinomas. Carotid body tumors may also accompany cancers of the larynx, breast, cervix, and colon
- Computed tomography scanning is recommended to delineate the extent of the mass and to rule out multicentric foci.
- Surgical resection remains the mainstay of treatment given the aggressive growth and malignant potential of CBTs. Shamblin type 1 and 2 tumors can often be dissected in a periadventitial plane without traumatizing the carotid vessels and without any need for arterial repair. If the proper plane between the tumor and the carotid arteries cannot be developed, resection of the involved portion may be required. The ICA should then be reinserted to the common carotid artery (CCA) or replaced with a saphenous vein interposition graft.
- Ligation of the ICA is associated with a high risk for stroke and a high mortality rate and should be avoided if possible.
- On the other hand, reconstruction of the ECA following tumor resection is not necessary, and it may be ligated.
- Operations for carotid body tumor are not risk-free. As the tumor grows, the surgery becomes more difficult, and the postoperative complication rate increases. The high rate of cranial nerve deficit on the first postoperative day may approach 49%.Even the majority of cranial nerve deficits are reversible, and the incidence of permanent cranial nerve palsy is reported to be low in the literature. Nevertheless, surgeons should be prepared to employ vascular reconstructive techniques, if necessary. In cases in which the clamping period is less than 10 minutes, the risk of developing neurological damage is quite low.?
- Radical resection prevented local recurrence and favorably affected the long-term results.
- Preoperative embolization has a high risk of stroke associated with accidental ICA embolisms when using the embolization material. Besides, in the literature, the true benefit of preoperative embolization is not recognize because does not significantly improve the conditions for a safest resection o.
- The malignant degeneration of Carotid body tumors is has been estimated at between 5 and 10% but in young patients, is higher. Malignancy is determined by the detection of metastases in local lymphatic nodes or remote organs such as the lungs, bones, liver, pancreas, thyroid, breast, and thorax rather than by the histological criteria or development of malignancy in neoplasms. The incidence of local or distant metastases is less than 10%. 16 In the end Carotid body tumors even if are slowly growing tumors, early diagnosis as well as early surgical treatment are important because of their risk of malignancy, locally aggressive growth potential, invasiveness of the essential ICA, last 4 cranial nerves.
- A good cooperation between ENT surgeon, imagistic, vascular surgeon, neurology, maxilla-facial surgery is essential for the best results.
- Surgical excision is the best treatment modality for glomus caroticum tumors. Arterial continuity should be maintained and special attention should be made to avoid damaging adjacent vascular and neural structures during dissection.
- If an early surgery will be able to prevent the neurological and vascular complications associated with carotid body tumors metastasis may appear years after the first resection, so is very important long-term follow is necessary.
The most common presentation in patients with CBTs is a slowly enlarging painless mass in the neck.
Magnetic resonance angiography, CT angiography, and DSA all can demonstrate the extent of the tumor and its relationship to adjacent structures In addition to the preoperative Doppler USG and CT performed on all of our patients, we used MR angiography for five patients, CT angiography for one, and DSA
References
- Van Haller (1743) Cited by Kohn A, Die paranganglien. Arch Mikr Anat 62: 263-268.
- Sajid MS, Hamilton G, Baker DM (2007) Joint Vascular Research Group. A multicenter review of carotid body tumour management. Eur J Vasc Endovasc Surg 34:127-130.
- Luna-Ortiz K, Rascon-Ortiz M, Villavicencio-Valencia V, Granados- Garcia M, Herrera-Gomez A (2005) Carotid body tumors:review of a 20-year experience. Oral Oncol 41(1): 56-61.
- Chedid A, Jao W (1974) Hereditary tumors of the carotid bodies and chronic obstructive pulmonary disease. Cancer 33(6): 1635-1641.
- Kaman L, Singh R, Aggarwal R, Kumar R, Behera A, et al. (1940) Diagnostic and therapeutic approaches to carotid body tumours: report of three cases and review of the literature. Aust N Z J Surg 69: 852-855.
- Gordon-Taylor G (1940) On carotid tumours. Br J Surg 28:163-172.
- Shamblin WR, ReMine WH (1971) Carotid body tumor (chemodectoma). Clinicopathologic analysis of ninety cases. Am J Surg 122: 732-739.
- Dickinson PH, Griffin SM, Guy AJ, McNeill IF (1986) Carotid body tumour: 30 years experience. Br J Surg 73(1): 14-16.
- LaMuraglia GM, Fabian RL, Brewster DC, Pile-Spellman J, Darling RC, et al. (1992) The current surgical management of carotid body paragangliomas. J Vasc Surg 15(6): 1038-1044.
- Kotelis D, Rizos T, Geisbüsch P, Attigah N, Ringleb P, et al. (2009) Late outcome after surgical management of carotid body tumors from a 20- year single-center experience, Langenbecks Arch Surg 394(2): 339344.
- Seabrook GR, Haimovici H (1996) Nonatherosclerotic cerebrovascular disease. Haimovici's vascular surgery, Blackwell Science, USA.
- Van der Mey AG, Frijns JH, Cornelisse CJ, Brons EN, van Dulken H, et al. (1992) Does intervention improve the natural course of glomus tumors? A series of 108 patients seen in a 32-year period. Ann Otol Rhinol Laryngol 101: 635-642.
- Wang SJ, Wang MB, Barauskas TM, Calcaterra TC (2000) Surgical management of carotid body tumors. Otolaryngol Head Neck Surg 123(3): 202-206.
- Plukker JT, Brongers EP, Vermey A, Krikke A, van den Dungen JJ (2001) Outcome of surgical treatment for carotid body paraganglioma. Br J Surg 88: 1382-1386.
- Dardik A, Eisele DW, Williams GM, Perler BA (2002) A contemporary assessment of carotid body tumor surgery. Vasc Endovascular Surg 36(4): 277-283.
- Krupski WC (2006) Carotid body tumors. In: Rutherford RB, editor. Vascular surgery. (6th edn), W.B. Saunders, Philadelphia, USA, pp. 2066-2073.
- Patetsios P, Gable DR, Garrett WV, Lamont JP, Kuhn JA, et al. (2002) Management of carotid body paragangliomas and review of a 30-year experience. Ann Vasc Surg 16: 331-338.
- Muhm M, Polterauer P, Gstöttner W, Temmel A, Richling B, et al. (1997) Diagnostic and therapeutic approaches to carotid body tumors. Review of 24 patients. Arch Surg 132(3): 279-284.
- Litle VR, Reilly LM, Ramos TK (1996) Preoperative embolization of carotid body tumors: when is it appropriate? Ann Vasc Surg 10: 464468.
- McPherson GA, Halliday AW, Miss AO Mansfield (1989) Carotid body tumours and other cervical paragangliomas: diagnosis and management in 25 patients. Br J Surg 76(1): 33-36.
- Del Guercio L, Narese D (2013) Carotid and vagal body paragangliomas. Transl Med UniSa 6(6): 11-15.
- Kataria T, Bisht SS (2010) Synchronous malignant vagal paraganglioma with contralateral carotid body paraganglioma treated by radiation therapy. Rare Tumors 2(2): e21.
- Kollert M, Minovi AA, Draf W, Bockmuhl U (2006) Cervical paragangliomas—tumor control and long-term functional results after surgery. Skull Base 16(4): 185-191.
- Beigi AA, Ashtari F, Salari M, Norouzi R (2013) Convulsive syncope as presenting symptom of carotid body tumors: case series. J Res Med Sci 18(2): 164-166.
- Lustrin ES, Palestro C, Vaheesan K (2001) Radiographic evaluation and assessment of paragangliomas. Otolaryngologic Clinics of N America 34(5): 881-906.





























