Perilymph Fistulae: An Uncommon Cause of Dizziness
Tiffany Whitney* and Steven Parnes
Division of Otolaryngology Head and Neck Surgery, Department of Surgery, Albany Medical Center, USA
Submission: June 01, 2017; Published: June 06, 2017
*Corresponding author: Tiffany Whitney, Division of Otolaryngology Head and Neck Surgery, Department of Surgery, Albany Medical Center, Albany, New York, USA, Tel: (518)262-5575; Email: chentl@mail.amc.edu
How to cite this article: Tiffany W, Steven P. Perilymph Fistulae: An Uncommon Cause of Dizziness. Glob J Oto 2017; 8(3): 555738. DOI: 10.19080/GJO.2017.08.555738
Abstract
Dizziness is common complaints that people seek medical attention for. It is listed as one of the top ten symptoms evaluated by primary care providers. To determine the cause of dizziness requires a detailed and careful history and physical examination, with a particular focus on the otolaryngological aspects. A differential diagnosis can be generated from the initial evaluation that can be further corroborated with laboratory tests and imaging studies such as audiograms, video nystagmography, CT scans and MRIs. At this stage, one can often determine whether a patient presents with a vestibular or non-vestibular cause and then refer to the appropriate specialist. To an otolaryngologist, a vestibulopathy is usually apparent in the initial encounter and can be categorized as benign positional vertigo, vestibular neuronitis, viral labyrinthitis, or Meniere's disease. However, when the patient does not conform to these categories, one must consider other causes, such as atypical or vestibular migraine, superior canal dehiscence syndrome, debarquement syndrome, or perilymph fistula (PLF).
Introduction
An inner ear fistula is defined as an anomalous communication between the labyrinth and surrounding structures, leading to abnormal drainage of perilymph fluid into the middle ear. Etiology includes head trauma, barotrauma, iatrogenic injury after stapedectomy, spontaneous development, congenital anomalies (such as Mondini's dysplasia), or erosive bony labyrinth break down from chronic middle ear disease. The perilymph can leak into the middle ear through the oval window, round window, or a fissure in the bony labyrinth [1].
Patients will often present with symptoms of vertigo, hearing loss, and tinnitus, but sometimes the presentation is variable and can be indistinguishable from patients with other vestibulopathies. There is no audiologically distinct pattern for PLF, and vestibular complaints can be quite protean, ranging from true vertigo or Meniere-like attacks, to an off-balance sensation; both Tulio's phenomenon and the Hennebert's sign have also been noted in these patients [2].
Conservative management is often recommended because many PLF will heal spontaneously. For those who have persistent symptoms with a high suspicion of this diagnosis, the management remains controversial. The variable diagnostic criteria and lack of any laboratory or imaging studies to prove this entity creates a clinical challenge. In addition, the total volume of perilymph is estimated to be 3 micrometers [3], and past studies have determined that the amount of intraoperatively collectable perilymph fluid is too small for protein marker testing with reliable sensitivity. Therefore, in order to ascertain the diagnosis, an exploration of the middle ear via exploratory tympanotomy is recommended, during which one could note the presence of clear fluid pooling in the oval or round window, though this is not definitive evidence of fistula, as it could also be attributed to transudation or accumulation of local anesthetic. As a result, there is no clear consensus on the diagnosis or management of PLF [4].
No large series have distinguished improvement after exploratory tympanotomy based on traumatic or non-traumatic ideology. Goodhill proposed a theory of labyrinthine window rupture after traumatic PLF, in that an explosive force could rupture the intratympanic basilar and Reisner's membranes into the scala vestibule leading to potential injury to the labyrinthine round window membrane or annular ligament of the stapes. It has also been proposed that an intratympanic implosive force from a valsalva maneuver could cause a sudden increase in pressure that ruptures these structures [3]. The objective of this study was to determine if the etiology of the fistula affected clinical response to exploratory tympanotomy and repair.
Methods
This was an institutional review board-approved retrospective chart review of patients who underwent perilymph fistula exploratory tympanotomy by the senior author from 20052015 with the aim of analyzing the approach to management of PLF, the indications for surgery, and the improvement of symptoms, specifically focusing on patients with traumatic vs. non-traumatic PLF. Data collection included age, primary and secondary symptoms, postoperative findings, imaging and ancillary tests, and etiology of the PLF. Data on evidence of intraoperative PLF, use of graft, perioperative complications, postoperative symptom changes, and postoperative audiograms (when available), months of follow up, symptom reoccurrence, and secondary surgeries were collected.
The senior author has performed over 300 exploratory tympanotomies for perilymph fistulae over a forty year period. Initially, the surgical approach comprised an exploratory tympanotomy and evaluation of the oval and round window regions for the presence of a fistula. Regardless of presence or absence of clear fluid, the windows were packed with temporalis fascia followed by gel foam. In an early review, it was noted that 60% of patients had improvement in vestibular and audiometric symptoms. After ten years, fibrin glue was added to the armamentarium, which resulted in a 10% increase in the improvement rate. In this study population, each patient underwent the standardized exploratory tympanotomywithtemporalis fascia graft repair followed by gel foam and fibrin glue placement in the oval and round window,regardless of whether a fluid leak was identified.
Results
A total of 58 patients were included in the study, with an average age of 52; 27 patients were males and 31 were female. The average length of time from initial office visit to surgery was 4.9 months and the average duration of follow up postoperatively was 19.5 months. Thirty-seven patients underwent imaging studies, of which 6 had positive findings that possibly contributed to their symptoms (i.e. temporal bone fracture, superior semicircular canal dehiscence, and foreign body).Thirty-three patients received a preoperative audiogram, while only 16 underwent audiometric testing postoperatively. Ten patients underwent vestibular testing with electro nystagmography or video nystagmography.
Presenting symptoms were attributed to a traumatic etiology in 69% of patients andnon-traumatic causes in 31%. Traumatic causes included head trauma (35 patients), barotrauma (4), and penetrating trauma (1).Non-traumatic etiology included previous history of stapedectomy, other ear surgery, infection, and unknown cause. The most common presenting symptomsin this cohort were dizzinessor loss of equilibrium (87.5% of trauma and 72.2% of non-trauma patients), vertigo (30% of trauma and 38.9% of non-trauma patients), and hearing loss (22.5% of trauma patients and 38.9% of non-trauma patients)[4] . Of the patients with complete operative reports, 70.7% had visible perilymph fluid at the time of surgery. Perilymph fistula occurred at the oval window with the highest frequency (61% of patients) followed by the round window (36.6%); one patient had simultaneous oval and round window fistulae (2.4%).
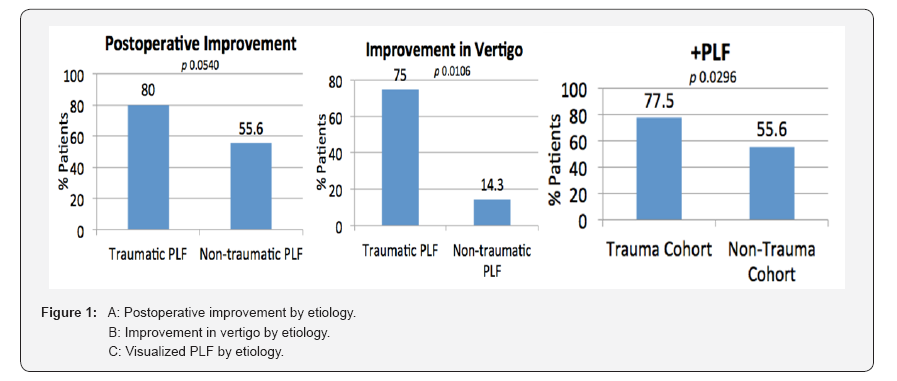
Traumatic etiology comprised a majority of patients with successful visualization of PLF on exploration (31 patients, 75.6%) versus 10 patients (24.4%) of non-traumatic etiology, while most patients with a negative PLF at surgery had clinical symptoms most likely attributed to non-traumatic cause-6 patients (60%) versus 4 patients (40%) from a traumatic etiology. Analysis by traumatic versus non-traumatic etiology revealed that the patients with traumatic etiology were more likely to have a positive PLF upon exploration (77.5% of trauma vs. 55.6% of non-traumatic patients), as exhibited in Table 1 and Figure 1C. This proved to be statistically significant (P=0.02956). Most trauma-induced PLF were localized to the oval window (58.1%), while most non-traumatic PLF were localized to the round window (70%); this was not statistically significant (P=0.0999).
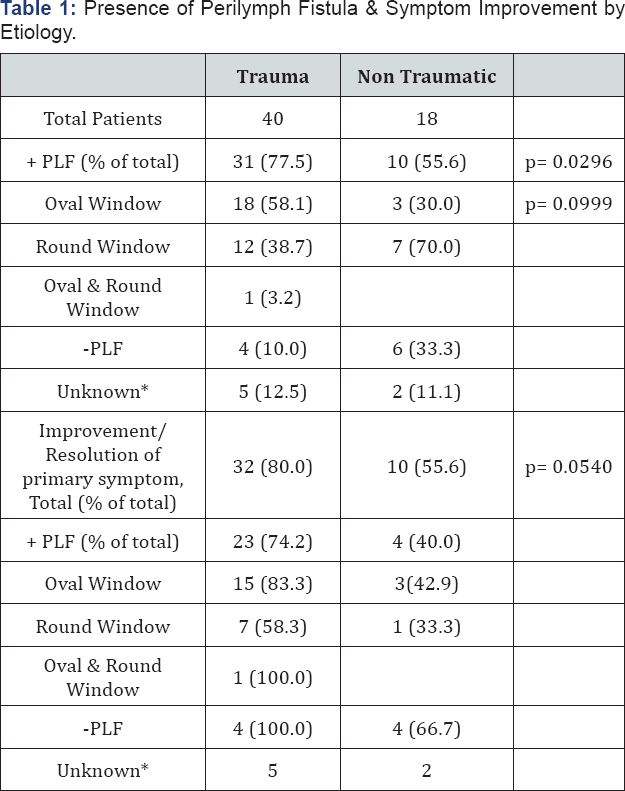
*no operative report.
All patients received temporalis fascia grafts at the round and oval windows followed by gel-foam packing and fibrin glue. No patients experienced perioperative complications. Seventy two percent of patients experienced improvement or resolution of their primary presenting symptom (65.9% of patients with positive PLF, 80.0% with negative PLF, P=0.3874); 54.5% of patients had improvement or resolution of secondary symptoms after surgery (52.2% of patients with positive PLF, 33.3% with negative PLF). When analyzed by traumatic versus non-traumatic etiology (Table 1), 80% of trauma patients had improvement or resolution of their primary symptoms (74.2% of patients with positive PLF improved, 100% of negative PLF patients improved) while only 55.6% of non-traumatic patient had improvement (40.0% with PLF, 66.7% of negative PLF patients);this approached statistical significance (P=0.0540, Figure 1A).
Greatest improvement in trauma patients was achieved for dizziness and nausea/vomiting, followed by tinnitus and dysequilibrium. In the non-trauma patients, the greatest improvement was exhibited with otalgia, dizziness, and dysequilibrium. Overall, there was greater postoperative improvement investibular symptoms in trauma patients and cochlear symptoms in non-trauma patients. Of note, the difference in improvement in vertigo was statistically significant when comparing trauma versus non-trauma patients (P=0.01606, Figure 1B).
Discussion
Many institutional series were published on the topic of clinical improvement after exploratory tympanotomy for perilymph fistula in the past. In the Iowa experience, 49% had improved hearing and 95% had improved vestibular symptoms [5] . This was followed by the Stanford experience- 64% of +PLF and 44% of -PLF patients had resolution of their major symptom [6]. The House experience showed 43% had subjective improvement [7]. In 1997, the DC experience showed improved vestibular symptoms in 87% of patients and improved hearing in 40% [8]. In 2014, a Montreal series concluded that there were no predisposing factors from history or clinical exam to predict PLF [9]. In our series of 58 patients, 72.4% experienced improvement or resolution of the primary symptom after surgery. Though this did not reach statistical significance, our results are consistent with the range of improvement in previous studies.
Goodhill proposed that acute "explosive" and "implosive" forces led to labyrinthine window rupture and traumatic PLF We believe that the acute nature of these changes leads to a more severe and dramatic onset of PLF symptoms, particularly vestibular symptoms. Once repair is performed, re-equilibration leads to symptom improvement. Non-traumatic PLF tend to have a more latent course, and over time may impact the cochlear system more than the vestibular system due to the slow nature of change. This may explain the trend towards increased vestibular symptom improvement (particularly vertigo) in the trauma cohort and increased cochlear symptom improvement in the non- traumatic cohort, as well as the finding of increased frequency of +PLF in the trauma cohort. Perhaps due to the insidious nature of chronic ear disease, the non-traumatic cohort may develop micro fistulae that are not grossly apparent intraoperatively, or other changes that cannot be effectively resolved surgically. This is further corroborated by our data on repeat exploratory tympanotomy for poorly-controlled symptoms. Most patients undergoing multiple surgeries originally suffered from acute head trauma, and there was a greater improvement in vestibular symptoms after reoperation than cochlear symptoms.
Weaknesses of this study are due to its retrospective nature. The trauma and non-trauma PLF cohorts were unequal in size due to the nature of the referrals and patient population. Inconsistent documentation and non-standardized diagnostic work-up and follow-up lead to several variables that were difficult to control. This study can be expanded upon in the future with a prospective arm, with implementation of validated questionnaires pre- and postoperatively to objectify the results, as well as a separate analysis of audiogram data.
Conclusion
One must be diligent when a patient presents with a diagnosis of dizziness, specifically when it appears to be from a vestibular cause. Perilymph fistula should certainly be considered when more obvious vestibulopathies have been ruled out. A majority of these patients seem to benefit from exploratory tympanotomy whether or not a PLF is confirmed at the time of surgery. As this study shows, there is greater improvement in traumatic PLF patients versus non-traumatic PLF patients overall, as well as a trend toward greater improvement in vestibular symptoms (particularly vertigo) in traumatic PLF patients and in cochlear symptoms in non-traumatic PLF patients. Hopefully these findings can help guide future management of PLF and counseling on postoperative outcomes based on the etiology of the disease.
References
- Crane BT, Minor LB (2015) Cummings Otolaryngology: Head and Neck Surgery, (6th edn). Chapter 165 Peripheral Vestibular Disorders. Flint PW, Elsevier Saunders, Philadelphia, USA, pp. 2562-2563.
- Glasscock ME (1987) Persistent traumatic perilymph fistulas. Laryngoscope 97: 860-864.
- Maitland CG (2001) Perilymphatic fistula. Curr Neurol Neurosci Rep 1: 486-491.
- Hornibrook J (2012) Perilymph fistula: fifty years of controversy. ISRN Otolaryngology 1-9.
- Seltzer S, McCabe BF (1986) Perilymph fistula: the Iowa experience. Laryngoscope 94: 37-49.
- Shelton C, Simmons FB (1988) Perilymph fistula: the Stanford experience. Ann Otol Rhinol Laryngol 97(2 Pt 1): 105-108.
- Rizer FM, House JW (1991) Perilymph fistulas: the House Ear Clinic experience. Otolaryngol Head Neck Surg 104: 239-243.
- Fitzgerald DC (1997) Perilymphatic fistula: a Washington, DC, experience. Ann Otol Rhinol Laryngol 106(10 Pt 1): 830-837.
- Alzahrani M (2014) Perilymphatic fistulas: can we predict the diagnosis? Eur Arch Otorhinolaryngol 1-7.





























