Relapsing Polychondritis - Presenting As a Recurrent Auricular Perichondritis-Case Report
Cristina Otilia Laza1* and Sarv Mostafa2 and Claudia Mihailov3
1Assistant Professor, Maxillo-facial surgery Clinic, Romania
2ENTsurgeon, Romania
3Rheumotology Clinic, Romania
Submission: May 01, 2017; Published: May 30, 2017
*Corresponding author: Laza Cristina Otilia, ENT/OMF Clinic, SCJU , SF APOSTOL ANDREI, B-dul Tomis 145 , 900432, Constanta, Romania, Email: cristinaotilia@gmail.com
How to cite this article: Cristina O L,Sarv M ,Claudia M. Relapsing Polychondritis - Presenting As a Recurrent Auricular Perichondritis-Case Report. Glob J Oto 2017; 8(3): 555736. DOI: 10.19080/GJO.2017.08.555736
Abstract
Authors presents a rare case of relapsing polycondritis in a middle age man, which went undiagnosed for six months. With bilateral perichondritis of the auricles was unsuccessfully rebel to usual treatment. Evaluations of nonspecific anti-inflammatory testes-fibrinogen, Erythrocyte Sedimentation Rate, PCR were extremely high, like in an autoimmune disorder. A very complex clinical exam, combining with specific lab tests establish the diagnosis, and the treatment with Steroids was amazing. Then was transferred to rheumatology department were he continue the investigations and treatment. Now is on specific treatment, with Medrol and Imuran, with minimum accuses, till now without severe complications
Keywords: Polycondritis; Recurrence; Autoimmune disorders
Introduction
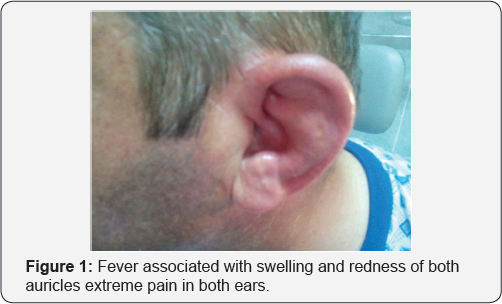
Our patient an 45 year old men, came to our ENT Department with fever associated with swelling and redness of both auricles extreme pain in both ears without, history of trauma, but also with a sudden hearing loss on the right ear, tinnitus, vertigo, or otorrhea. Bilateral also he presents red watering eyes, pain and swelling of the joints. The patient’s past history was significant,6month ago starts with redness and swelling of both ears, arthritis, periods of irritative cough and dysphonia -scratchy voice also fevers and chills sometimes (Figure 1).
A long series of doctors from general practice, emergency, ENT, dermatology departments consider first his condition as a bacterial external otitis with Staphilococcus auresus or Pseudomonasomplicated with perichondritis of the pinna and treat him with courses of oral or IV. Antibiotics like oxacillin, ciprofloxacin cephalosporines without remission. ENT examination showed not just the auricles edematous, redness, without fluctuence, Inflammation was extending in the EAC but without otorrhea.
Otoscopy-ear drum normal
Audiometry: Pure tone audiometry - moderate mixt -sensori neural predominant type of deafness on right ear. He accuse also recurrent attacks of vertigo at sudden head movements -vestibular test revealed -nystagmus + in horizontal rotatory plane, Romberg, Weil-Babinsky tests, positive-Head shake test positive. Review of symptoms and erythrocyte sedimentation and PCR rate significantly very high elevated, force us to think at a possible polychondritis and transfer the patient to the Rheumatology department after a previous cartilage biopsy showing a mixed inflammatory infiltrate of lymphocytes, neutrophils, and plasma cells in the perichondrium. Inflamed joints were asymmetric, polyarticular, non deforming, and nonerosive. Involving the ankles, elbow, wrists, proximal interphalangeal joints, metacarpophalangeal joints, with effusion and mild inflammatory signs. Ophthalmological examination revealed conjunctivitis in right eye and episcleritis in the left eye.
a) Neurological exam-normal
b) Cardiological with EKG, echography -normal
c) Dermatological exam normal.
d) Pneumophtiziology examinations with spirometry were normal (Figure 2)

IMAGISTIC
a) X ray examination of facial bones showed the nasal cartilages intact
b) Chest X-ray was normal no tracheal stenosis or calcifications
c) X-ray of the joints -inflammation of the joints
d) CT scan spiral-better exploring thorax ,lungs
e) MRI-exceptional for inflammation
f) Scintigraphy with Technetium
Laboratory Findings
a) Complete blood cell count (CBC) -anaemia normocytic,normocromic, mild leukocitosis
b) Metabolic panel :glucosis, Serum creatinine
c) Liver transaminase and serum alkaline phosphatasestudies
d) Nonspecific indicators of inflammation (eg, elevatederythrocyte sedimentation rate= 53 (1-7 mm/h);, elevated levels of C-reactive protein)
e) Rheumatoid factor, and antiphospholipid antibodies (if history of thrombosis is found)-
f) Urinalysis dipstick and microscopic evaluation of sediment
g) Cryoglobulins
h) Viral hepatitis panel
i) Antinuclear antibody (ANA)
j) Antineutrophil cytoplasmic antibody (ANCA)
k) ASLO < 200 Ul/rnl
l) VDRL (-);
m) acid alpha 1 glucoprotein = 395 (43-130 mg/dl).
n) Prothrombin Time = 80.8 (>70%); INR = 1.19; PTT =1.0 «1.25); Bleeding Time = 1 (1-3 min); coagulation time =7 (4-9).
o) anti native DNA antibody(-),
p) anti ENA antibody (UI-RNP, anti-Sm, anti SS-AlRo,anti- SS-BlLa) =(-); CH50 = 188 U(130-330);
q) LE cels; Mucoprotein = 5.3
r) PCR for TB, Sputum cultures(-)
s) Blood cultures in fever were negative
t) Bacteriological and mycological examination of otorheea-Staphilococcus ,Candida were negative
Other Test
a) Bacteriological and viral ex of CSF- meningitis
b) BYOPSY from cartilage
c) Sypirometry
d) EKG
e) EEG
f) AUDIOMETRY-Pure tone audiometry,immitance audiometry
g) Vestibular tests-Vegn,Posturography,Head Shake Test (Figure 3)

The diagnosis supposition of relapsing polychondritis was confirm and started on Medrol so he improved gradually clinically and the auricular erythema, edema, and tenderness disappeared, also joints swelling and conjunctivitis, his erythrocyte sedimentation and PCR rate slowly normalized and now is on permanent follow up. At 6 month we explore endoscopic the superior airways, to discover in time an eventual stenosis. Also we complete the exam with otoscopy and audiometry also vestibulomatr.
Discussion
a) Relapsing polychondritis is a rare disease of unknown etiology easily misdiagnosed characterized by episodic attacks of inflammation of hyaline and elastic cartilaginous structures including the ears, nose, larynx-trachea, and articular cartilages, as well as other organs So is not rare to discover a long number of consultations and treatment before you .
b) It is thought to be an autoimmune disease based on, the presence of serum antibodies to type 11 collagen during an acute attac, granular deposits of IgG, IgA, IgM, and C3, as immune complexes , cell-mediated immune responses to various cartilage components . An increase in HLADR4 antigen was detected in patients with relapsing polychondritis, association with other autoimmune disorders such as vasculitis, the presence of cartilage inflammation on biopsy, anticollagen antibodies, and a therapeutic response to corticosteroid therapy.
c) Relapsing polychondritis was first described in 1923 by Jaksch-Wartenhorst as "polychondropathia" or systemicor chronic chondromalacia. Carl Pearson in 1960 suggested the term relapsing polychondritis, highlighting the episodic nature of the syndrome. Only 500 cases have been published worldwide up until now. Diagnosis is made with difficulty when cartilage material cannot be obtained for analysis, or in advanced cases is replacing by fibrous tissues. When there is no possibility of a histological diagnosis, it must be made clinically.
Signs and symptoms reported in patients with relapsing polychondritis before and after diagnosis include the following:
- General - Intermittent fever, weight loss, and skin rash
- Auricular chondritis 85%-95%. Unilateral or bilateral auricular pain, swelling, and redness develop suddenly but spare the lobules, recurrence. The ear cartilage softens and collapses with the EAC, nodules calcification occurs in 40% of patients.
- External, media, suppurative otitis
- Audiovestibular damage-46%-50% of patients,
- Sudden loss of hearing, is attributed to vasculitic damage to the VIII CN, tinnitus, nystagmus and vertigo
- Nonerosive seronegative inflammatory polyarthritis in 52%-85% of patients.
- Arthritis is asymmetric, oligo- or polyarticular, nondeforming, and nonerosive with effusions without or with mild inflammation.
- The ankles, elbow, wrists, proximal inter- phalangeal joints, meta-carpo-phalangeal joints, and metatarsophalangeal joints are often involved, although any joint may be affected. The costo-chondral, sternoclavicular, and sternomanubrial joints may be involved. The forefeet are usually spared.
- Nasal chondritis 48%-72%. The nasal chondritis is acute and painful a feeling of fullness over the nasal bridge, with nasal obstruction, mild epistaxis, finally with saddle- nose deformity.
- Ocular inflammation
a) Episcleritis (39%), Scleritis (14%).,Peripheral ulcerative keratitis in 4%
b) Papilledema visual field defects, ptosis, lid retraction, proptosis, and cataracts.
XI. Respiratory tract chondritis affects 40%-56% of patients may include:
a) Chondritis inflammation and swelling of the larynx- thyroid cartilage, trachea-with hoarseness, dyspnea- bradipneea, stridor, cough-weakens the cartilages, replacing by collapsible fibrotic tissues Dyspnea, may require tracheostomy
b) Acute inflammation of the distal airways can lead to obstruction and recurrent pneumonia.
XII. Cardiovascular disease in 24% of patients.
a) Aortic and mitral valve regurgitation, aortic aneurysm, aortitis, aortic thrombosis, pericarditis, first- to third-degree heart block, and myocardial infarction,
b) Relapsing polychondritis aortitis exhibits inflammation in the media, leading to loss of glycosaminoglycans and elastic tissue of the aorta -especially in ascending aorta ,also aortic ring and abdominal aorta
XIII. Skin disease in 17%-39%
a) Aphthous ulcers are the most common, Limb nodules, purpura, papules, sterile pustules, superficial phlebitis, live do reticularis, limb ulceration, and distal necrosis have been reported.
b) Rarer findings include
i. Sweet syndrome, (Acute febrile neutrophilic dermatosis)
ii. Kaposi sarcoma.
iii. Cutaneous vasculitis: purpura or as hemorrhagic bullae, typically on the lower extremities
iv. Erythema elevatum diutinum
v. Cutaneous polyarteritis nodosa
c) Palpable purpura
i. Subcutaneous inflammatory nodules resembling erythema nodosum
ii. Panniculitis: 5- to 10-cm tender erythematous nodules
d) Isolated
i. Hyperpigmentation
ii. Pustular psoriasis
iii. Macular purpura of the palms, soles, lower limbs, and buttocks
iv. Erythematous papular plaques of the face, upper and lower extremities, and thorax
v. Alopecia universalis
vi. Actinic granulomas
vii. Urticaria
viii. Angioedema
ix. Livedo reticularis
x. Erythema multiforme
e) Mouth and genital ulcers with inflamed cartilage (MAGIC syndrome):
i. begins with the oral and genital ulcers of Behcet disease.
ii. genital ulcers or erythema nodosum follows
XIV. Central nervous system
Seizures, memory loss, delusions, limb weakness, paresthesias or gait disturbances, or other cerebellar symptoms. Cranial nerve damage is common in relapsing polychondritis-associated CNS vasculitis and most often affects the II CN, followed less commonly by the VI,VII,VIII CN. Limbic encephalitis Aseptic meningitis
XV. Renal 29 (22%) had evidence of glomerulonephritis. The response to treatment varies from stabilization of renal function to renal failure.
XVI. Other conditions: Relapsing polychondritis has been seen in patients with underlying myelodysplastic syndrome and, less often, lymphoma. These cases may be paraneoplastic in nature. Acute mastitis may be found in relapsing polychondritis. Thromboembolism has been reported.
XVII. Laboratory Test: explore de lesions, extensions, complication, exclude other diseases-there is no specific test for RP -no Anticartilage Ab
Other Consultation
a) Dermatologists or specialists in infectious diseases are often involved early in the course of the disease to evaluate the patient for infectious causes of cellulitis or perichondritis.
b) Rheumatologists usually become the primary care provider
c) Ophthalmologists diagnose, monitor, and treat the potentially devastating ocular complications.
d) Cardiologists, neurologists, nephrologists, and otolaryngologists may be asked to manage other aspects of relapsing polychondritis.
e) Plastic surgeon for saddle-nose deformity.
Diagnosis Criteria
Diagnostic criteria for relapsing polychondritis first were proposed by McAdam et al. [1] and have been modified several times. Perform biopsy only if clinical criteria are in question.
McAdam et al. [1] criteria (3 of 6 clinical features)
a) Bilateral auricular chondritis
b) Nonerosive seronegative inflammatory polyarthritis
c) Nasal chondritis
d) Ocular inflammation
e) Respiratory tract chondritis
f) Audiovestibular damage
Damiani and Levine criteria (1 of 3 conditions)
a) Three McAdam et al. [1] criteria
b) One McAdam et al. [1] criterion plus positive histology results
c) Two McAdam et al. [1] criteria plus therapeutic response to corticosteroid or dapsone therapy
d) Michet et al. [1] criteria (1 of 2 conditions necessary for diagnosis)
e) Proven inflammation in 2 of 3 of the auricular, nasal, or laryngotracheal cartilages
f) Proven inflammation in 1 of 3 of the auricular, nasal, or laryngotracheal cartilages plus 2 other signs including ocular inflammation, vestibular dysfunction, seronegative inflammatory arthritis, and hearing loss [2-4].
Differential Diagnosis/Diseases Associated
Endocrine Disorders
a) Hashimoto thyroiditis/Hypothyroidism
b) Addison disease
c) Basedow Graves diseases
Autoimmune Rheumatic Diseases
a) Rheumatoid Arthritis
b) Sjogren's Syndrome
c) Systemic Sclerodermia
d) Psoriatic Arthritis
e) Systemic Lupus Erithematous
f) Mixed connective tissue diseases
Vasculitis
a) Granulomatosis Wegener
b) Polyarteritis Nodosa
c) Magic Syndrome
d) Churg Strauss
e) Behcet disease
f) Raynaud's Syndrome
Hematologic Diseases
a) Myelodisplastic syndromes
b) Hodgkin's lymphoma/Nonhodgkin’s lymphoma
c) Disgammaglobulinemia/Myxed cryoglobulinemia
d) Pernicious Anemia
e) Acute lymphoblastic leukemia
Dermatologic Conditions
a) Pioderma gangrenosum
b) Atopic dermatitis
c) Lichen plan,
d) Vitiligo
e) Paniculitis
Other Diseases
a) Ulcerative Colitis
b) Glomerulonephritis
c) Neoplasm Thymoma
d) Syphilis
e) Cellulitis
f) Myastenia gravis
Treatment
Medical Care
The goal of treatment is to abate current symptoms and to preserve the integrity of cartilaginous structures.
The mainstay of treatment is systemic corticosteroid therapy. Prednisone (20-60 mg/d) is administered in the acute phase and is tapered to 5-25 mg/d for maintenance. Severe flares may require 80-100 mg/d. Most patients require a low daily dose of prednisone for maintenance; however, intermittent administration of high doses during only flares of the condition is successful in rare cases. McAdam et al. [1] found that continuous prednisone decreased the severity, frequency, and duration of an acutisation. Other medications reported to control symptoms and, perhaps, progression of the disease, include dapsone (25200 mg/d), azathioprine, methotrexate (MTX; 7.5-22.5 mg/ wk), cyclophosphamide, and cyclosporin A. MTX has been administered beginning at 7.5 mg/wk, increasing up to 22.5 mg/wk in conjunction with steroid administration and has been found to significantly decrease corticosteroid requirements while controlling symptoms.
Cases reports have described successful treatment with the following:
a) Anti-tumor necrosis factor-alpha inhibitors : infliximab,etanercept, and adalimumab
b) Anakinra, an interleukin 1 receptor antagonist
c) Leflunomide, which inhibits pyrimidine synthesis
d) Rituximab, an anti-CD20 chimeric antibody
e) Tocilizumab, a humanized monoclonal antibody againstthe interleukin-6 receptor (IL-6R)
Oral administration of nonsteroidal anti-inflammatory drugs (NSAIDs) has not been effective.
Medical care must include assessment for and treatment of other confounding or concurrent autoimmune disorders.
Surgical Care of patients with relapsing polychondritis may include the following:
a) Tracheostomy in emergency
b) Permanent tracheotomy placement
c) Mastoidectomy
d) Tympanoplasty
e) Tracheal stent placement
f) Aortic aneurysm repair
g) Cardiac valve replacement
h) Saddle-nose deformity repair
Subglottic stenosis can be treated with submucosal corticosteroid injection followed by serial dilation. If not, MLSS- laser, ND-YAG, resection -reconstruction plus Montgomery tube. The benefits of any proposed surgery must be weighed adequately against the patient's risk for infection, especially in the event of acute relapse, since patients are at an increased risk of infection whether or not they are using corticosteroids [5]. Additionally, patients with relapsing polychondritis and tracheal disease may be at particular risk regarding complications resulting from tracheal intubation and extubation. Hearing-aids are useful in case of deafness, eventual with tinnitus maskers.
Complications
a Ear
i. Auricle cartilage softens and collapses forward.
ii. External auditory canal can collapse after 1 or more episodes. Nodularity of the auricle may develop. Calcification occurs in 40% of patients
iii. Deafness vertigo, tinnitus,
b. Eyes: Blindness
c. Airways
i. Larynx =voice hoarseness, epiglottitis, stenosis with dispneea,
ii. Nasal Pyramid deformity, saddle-nose,
iii. Laryngotracheobronchial Tree stricture, severe pulmonary infection, frail chest wall, respiratory failure,
d. Cardiovascular: aortic regurgitation, mitral regurgitation,aorticdissection, requires valvularreplacement and aneurysmal repair. Renal- glomerulonephritis- associated renal failure.
Prognosis
The 5-year survival rate associated with relapsing polychondritis was reported to be 66%-74% (45% if relapsing polychondritis occurs with systemic vasculitis), The most common causes of relapsing polychondritis-related death include are complications secondary to corticosteroid treatment or respiratory compromise (10%-50% of deaths), systemic vasculitis, and malignancies related [6]
Conclusion
a) Relapsing polychondritis is an uncommon, multisystem disease that can be life-threatening, debilitating, and difficult to diagnose.
b) It is characterized by recurrent, potentially severe, and frightening episodes of inflammation of cartilaginous tissues. All types of cartilage may be involved, including the elastic cartilage of the ears and nose, the hyaline cartilage of peripheral joints, the fibrocartilage at axial sites, and the cartilage in the tracheobronchial tree. Relapsing polychondritis can also inflame other proteoglycan-rich structures, such as the eye, heart, blood vessels, and inner ear.
c) Systemic symptoms (for example, fever, lethargy, and weight loss) are common, and vasculitis affecting skin or internal organs may occur. Patients can present with a wide array of painful symptoms that often pose major diagnostic dilemmas [7-9].
d) Because no specific tests for it are available, relapsing polychondritis must be diagnosed on clinical grounds. Pathogenetically, a linkage to HLADR4 and, occasionally, other autoimmune disease suggests that antiself reactions may be operative.
e) In most patients, relapsing polychondritis assumes a fluctuating but progressive course in which polycyclic bouts of inflammation eventually lead to the permanent destruction of the involved structure.
References
- McAdam LP, O'Hanlan MA, Bluestone R (1976) Relapsing polychondritis: Prospective study of 23 patients and a review of the literature. Medicine 55: 193-215.
- Damiani JM, Levine HL (1979) Relapsing polychondritis: Report of ten cases. Laryngoscope 89: 929.
- McCluskey RT, Thomas L (1958) The removal of cartilage matrix, in vivo, by papain: The identification of crystalline papain protease as the cause of the phenomenon. J Exp Med 108: 371.
- Hughes RAC, Berry CL, Seiffert M (1972) Relapsing polychondritis: Three cases with a clinico-pathological study and literature review. J Med 41: 363.
- Kindblom LG, Dalen P, Edmar G (1977) Relapsing polychondritis: A clinical, pathologic-anatomic and histochemical study of 2 cases. Acta Pathol Microbiol Scand 85: 656.
- Valunzuela R, Cooperrider PA, Gogate P (1980) Relapsing polychondritis: Immunomicroscopic findings in cartilage of ear biopsy specimens. Human Pathol 11: 19.
- Franssen MJ, Boerbooms AM, van de Putte LB (1987) Polychondritis and rheumatoid arthritis: Case report and review of the literature. Clin Rheumatol 6: 453.
- Harisdangkul V, Johnson WW (1994) Association between relapsing polychondritis and systemic lupus erythematosus. South Med J 87: 753.
- Michet CJ (1990) Vasculitis and relapsing polychondritis. Rheum Dis Clin North Am 16: 441.





























