Glomus Jugularae with Endocranial Extenion- Case Report
Cristina Laza*1 and Sarv Mostafa2
1Assistant Professor, Maxillo-facial surgery Clinic, Romania
2ENTsurgeon, Romania
Submission: April 23, 2017; Published: May 15, 2017
*Corresponding author: Laza Cristina Otilia, ENT/OMF Clinic, SCJU , SF APOSTOL ANDREI, B-dul Tomis 145 , 900432, Constanta, Romania, Email: cristinaotilia@gmail.com
How to cite this article: Cristina L, Sarv M. Glomus Jugularae with Endocranial Extension-Case Report. Glob J Oto 2017; 7(5): 555724. DOI: 10.19080/GJO.2017.07.555724
Abstract
Paragangliomas of the head and neck are rare tumors originated from the paraganglia cells located on the middle ear , jugular foramen and carotid body most frequent. Glomustumors usually occur in middle aged patients most frequent females and the evolution is very slow so the presentation is usually late. The principal symptoms are: pulsatile tinnitus, deafness, dizziness, cranial nerve palsies-IX-XI, rare VII or XII. The diagnosis requires intensive imaging studies -CT, MRI with contrast studies to reveal the vascular structure, the real extension, to determine the treatment and the prognosis. We present a case of a middle aged man with a glomus jugulare tumor with extension in the posterior cranial fossa, with a long history of evolution, misdiagnosed with chronic polypoidotitis .MRI-studies with contrast studies revealed the important extension in the temporal bone and endocranial extension. At the beniging he accept only radiotherapy finally, requiwiembolizationand surgery perform in cooperation neurosurgeon-otologist. was treated with gamma-knife surgery.
Keywords: Chemodectoma; Paraganglioma; Glomusjugulare; Glomustympanicum; Glomusvagale
Case Report
Our patient A.M. a 61 years man, was admitted in august 2007 in our clinic for a long history of mucopurulent, left-sided otorrheea, hearing loss, hemicrania discrete on the same side. The symptoms appeared 10 years before but were neglected by the patient, the only treatments were sporadic: earinstillations of drops but he can't remember a type. It was considered a chronic suppurative otomastoiditis with polypoidal degeneration of the mucosa because of chronic inflammation. Consequently was investigated by harvesting ear discharge for bacteriological examination, X-rays of the mastoid - Shuller, Stenvers views, audiometry without nothing particular-typical transmission type of deafness. We start a local and general antibiotic therapy based on antibiogramm and under local anesthesia, on the microscope we try to remove a giant polypoidal mass fully occupying the ear canal, no pulsatile, without particular aspect, except a significant bleeding and an abnormal hardness for an inflammatory polyp. We stopped the bleeding by plugging the ear channel with Merocel, gauses with adrenaline 1/10000 and sent the tissue removed to the anatomo-pathological examination. Which confirmed the vascular natures of the tumor we decide to perform an Angio MRI but the patient refused, and requested discharge? [1].
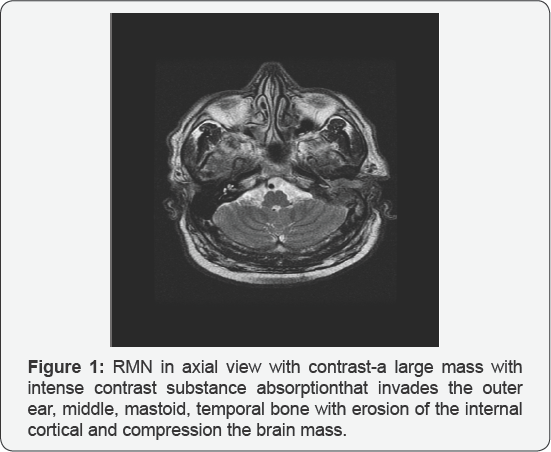
In January 2010 the patient returns with the same symptoms which added a left facial paroxysmal hemi spasm, hearing loss progress to cofosis, and a discrete dizziness appeared (Figure 1). Clinical examination -of the cervicofacial region and of the mastoid process-left facial -hemispasm. Cranial nerve examination is rest apparently normal. Otoscopy- with the otoscope, microscope or endoscope -left external auditory canal is occupied by a polypoidal, irregular, mass ,purple-red in colour , covered with yellow-green pus with bad odor , easy bleeding when is touched ,without pulsation . Tunning fork test -false negative Rinne test -left , Weber test deflected to the right Pure tone-auiiometry- leftcofosis. Acoustic immitance audiometry- cannot be perform on the left ear Imagistic -X-rays-Hirtz view of the skull base -enlargement of the foramen jugulare, he base of the diagnosis are CT scan who can revealed the destruction of the petrous temporal bone, mastoid process etc.
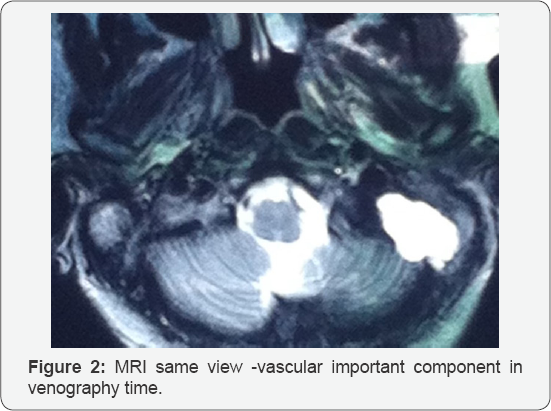
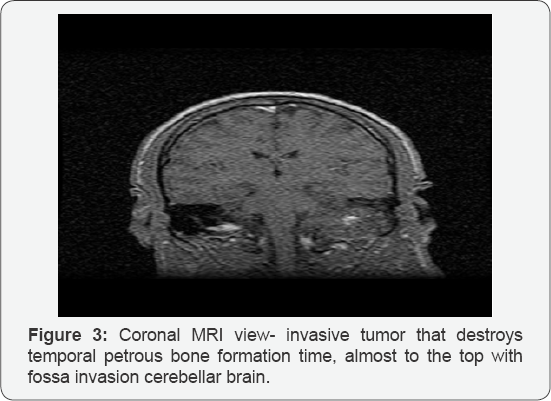
Using Angio CT scan we can obtain a complete image of the vascular tumor with 3D reconstruction if is required for surgery (Figure 2). Angio CT scan-reveals an intense iodophile a vascular tumor mass, occupying the outer ear, average domestic mastoid cells, and extensive erosion in the rock with its temporal and posterior cerebral fossa invasion, compression. MRI scan -complete the extension of the mass, brain status- edema, inflammation. Arteriography is necessary in large tumors for embilization or preoperatory, venography is also very useful. Neurosurgical examination confirmed the diagnosis of glomusjugulare with endocranial invasion recommending transfer to a Neurosurgical Clinic specialized in vascular brain tumors in Bagdasar Hospital Bucharest for treatment [2].Subsequently the patient refuse surgery and embolization because of the risks and accepted radiotherapy .He recognize that he want a second opinion in Italy -and the diagnosis and recommendation were similar so finally he accept surgery performed by a mixt team-ear surgeon and neurosurgeon both with great experience. They successfully remove the entire tumor without complication, no recurrence till now. The patient now 6 years after surgery at 3-4 month use to come for cleaning of the mastoid cavity on the microscope to remove was and epithelial debris. Also repeated CT scan are negative (Figure 3).
Background
Glomus tumors develop from embryonic neuroectoderm from neural crest paragangliomic cells associated with autonomic nervous tissue. At birth, areas of those structures are located on the carotid bifurcation-carotid body tumours, internal jugular vein bulb, middle ear, less the aortic arch, nasopharynx, larynx, orbit on the ciliary ganglion, or in the pterygopalatine fossa. Histologically these structures are composed of chemoreceptors type I and type II cells support a dense matrix of connective tissue between nerve fascicles and highly vascularized showing a maze arterial drains in a vast peripheral venous system. Chemoreceptors Type I and II secrete dopamine, noradrenaline, tumoral secretion and the most important blood supply is coming from ascending pharyngeal artery (EC). Large tumors can receive extended branches of the internal carotid or vertebral artery [3].
Tumors left from these tissues are called equal chemodectomas, paragangliomas noncromaphine. The first description of such tumors was made by Haller at the carotid bifurcation. In 1950, Mulligan calls these tumors chemodectomas to specify their origin. In 1971, Glenner and Grimly call these tumors paragangliomas based on anatomical and physiological characteristics. The incidence is very rare- 1 case per 1.3 million people; 0.6% of head and neck tumors, 0.03% of all tumors; however, it is the most common tumor of the middle ear and second of the temporal bone after acoustic schwannoma;
- In females are 3-6 more frequent than in males in 5070 decades in particular; especially on the left side
- 25-50% is in family cases, the gene responsible for these cases is located on 11q23 band.
May be associated with thyroid carcinoma, parathyroid adenoma and adrenal tumors. Chemoreceptor detect variations of O2 and CO2, ph, being able to influence blood pressure and cardiac respiratory rate. Glomustumours can be caused by chronic hypoxia because they were observed in hypoxic carotid corpuscle hypertrophy and there is an increased incidence of tumors in those who lives at high altitudes and in smokers. There are four primary sites:
- cells located on the adventitia of jugular bulb -glomusjugularae-most common,
- middle ear -chemoreceptors located on nerve Jacobson (auricular branch of IX-th nerve) -glomustympanicum,
- chemoreceptor cells located on a vagus nerve branch accompanying ear-glomusvagalae
- carotid corpuscle cells-carotid body tumors
- uncommonly occur in the trachea, larynx, nose, jaw, Fallopian channel [4].
Distant metastases occur very rarely: in lungs, liver, bones, in cases of malignant transformation.
I. Glasscock-Jackson and FISCH classification of glomus tumours based on the extension:
- tumor confined to the middle ear - glomustympanicum,
- tumor located in tympanomastoidiane area without involvement of the infralabyrinthine area
- tumor invading the infralabyrinthine compartment with extension to the petrous apex
- C1-tumor limited to the carotid canal,
- C2-tumor that invades the vertical portion of the carotid canal,
- C3-tumor that invades the horizontal portion of the carotid canal,
- C4-tumor that invades foramen lacerum, cavernous sinus.
- tumor with intracranial extension
- D1-less than 2 cm intracranial invasion,
- D2- more than 2 cm intracranial -intradural invasion.
Diagnosis is often late because their slow development 1020 years. Main symptoms are
A. Ear symptoms:
- pulsatile tinnitus,
- hearing loss
- auricular fullness,
- purulentotorrhea,
- haemorrhage,
- vertigo.
B. symptoms related to cranial nerves VII, VIII, IX, X, XI, XII:
- sore throat,
- dysphagia,
- dysphonia,
- hemitongue
- facial palsy
- Claude- Bernard- Horner sdr
C. Signs of catecholamine, norepinephine, dopamine, VIP, enolase, somatostatine discharge -pheocromocytoma like 2-4%:
- hypertension,
- tachycardia, arrhythmias,
- pallor, nausea
D. Invasion of brain-related symptoms:
- headache, hydrocephalus vomiting,
- ataxia, brainstem symptoms
E. Diagnosis requires
- Neurological, neurosurgical examination
- ENT exam
- otoscopy - otomicroscopy
- endoscopy -The eardrum is intact but in the hypotimpanum a blue or purple pulsating mass or the eardrum is destroyed and in the ear canal is a mass very irregular easy bleeding tumor.
- Cervical palpation -swelling around the angle of the mandible
- Ex. Of oro, hypo-,rhinopharynx, mouth larynx-pulsatile mass behind the posterior tonsilarpilar-parapharyngeal retrostilian space with cranial nerves IX, X, XI paralysis
- Imaging
- basic skull radiograph Hirtz - widening of the foramen jugulare
- Angio CT / MRI for the diagnosis of vascular tumor,
- arteriography is necessary for preoperative embolization, for large endocranial invasion arteriography on the ICA and Vertebral Artery are required
- Audiometry
- Immitance- tympanogram throbbing, saw tooth,
- liminal-tone audiogram -transmission or mixed -sensorineural hearing loss up to cofosis,
- Biopsy is proscribed histologic diagnosis of certainty is on track surgically resected.
I. Differential diagnosis
- OtitisMedia
- Chronic mastoiditis,
- Cholesteatoma ,
- Cholesterol granuloma ,
- Chronic serous otitis,
- Idiopathic blue eardrum [6]
- Eosinophilic Granuloma (Histiocytosis X)
- Benign Tumors
- Meningioma,
- Schwannoma,
- Neurofibroma ,
- Osteoma,
- Chordoma
- Malignant tumors
- Chondrosarcoma
- EpidermoidCarcinoma (primary and metastatic)
- Otosclerosis
- Carotydaneurysm, cavernous
- Haemangioma
- Arterial malformations
- Aberrant intrapetrous internal carotid artery,
- Idiopathic hemotympanum,
- Prominent jugular bulb,
- Persistent stapedial artery
- Lymphoma
II. Treatment varies from simple periodic follow-up to surgery:
- Periodic follow- expectation is the best method in patients with small tumors, elderly or asymptomatic uncomplicated, and is best perform monthly, CTAngio scan at 6 month
- Medical Therapy in cases alpha-blockers and betablockers are useful for tumors secreting catechol amines, usually administered for 2-3 weeks before embolization and/or surgery to avoid potentially lethal blood pressure lability and arrhythmias.
- Pulmonary metastases are treated with with etoposide (VP-16) and cisplatin
- Surgical treatment:
- Type A: transmeatal or perimeatal approach the glomustympany
- Type B-extended posterior tympanostomy
- Type C require radical resection via a standard combined transmastoid-infratemporal or transtemporalinfratemporal approach with or without internal carotid artery (ICA) trapping, preceded by external carotid artery (ECA) embolization or superselective embolization. Intratumoral injection of cyanoacrylate glue has been proposed to control bleeding.
- Type D tumors -combined otologic and neurosurgical approach. An infratemporal approach with a skull base resection and a posterior fossa exploration. Partial resection of the tumor needs to be followed by radiation and follow-up [7].
- Radiation therapy it is useful ,as a classic fractionated radiation therapy with CO 60(40-50 Gy) and stereotactic radiosurgery (eg, gamma knife surgery) are successful in long-term control of tumor growth , because of fibrosis of the vessels and in decrease of catecholamine excretion in functional tumors;
- Radiation treatment is advised as the sole treatment modality for elderly or infirm patients who are symptomatic, those with extensive or recurrent tumors, or may be indicated to treat residual tumor following subtotal resection.
III. Complications of surgery
- Death,
- Bleeding massive-rupture of IC ,JV ,Lateral venou sinus
- Fistula CSF +/- meningitis, paralysis of cranial nerves, relapse.
IV. Complications of radiation
- Recurence, second tumor,
- ICA thrombosis,
- Pituitary -hypothalamic insufficiency,
- CSF leak, skull, brain or duranecrosis, encephalitis radically.
Funding
- Glomus tumors ar vascular tumors containing chemoreceptor cells type I and type II- rarely found in the temporal bone, yet it is the most common benign tumor of the middle ear.
- Tumor progression is very slow- 10-20 years, resulting in reduced symptoms, often neglected, leading to a later presentation, for example one of my cases -un old lady has a giant glomus invadind EAC, middle inner ear, mastoid cell, the entire temporal petrous bone. Superior was extended in the entire temporal lobe but also occipital .Inferior extend through the foramen jugulare on the neck-parapharyngeal retrostilian space ,with palsy of CN VII,VIII,IX,X XI,XII.
- Diagnosis is made by imaging studies with contrast, ANGIO CT scan being the biopsy is outlawed
- Glomus tumor most often is mistaken with a polyp caused by inflammation in chronic supurrative otitis. As an anecdote in residency my first trans tympanic injection was in a glomus looking like a Serous chronic otitis bilateral, but on this side looking like an Idiopathic blue eardrum. The doctor who teach me, an experienced cofosurgeon was indicating exactly the point where to inject, looking through the spy of the microscope. After the incident we explore the patient and we discover the enlargement of the foramen jugulare on Hirtz X-ray position ,and the exactly extension on the CT scan. Our lady was treated with radiotherapy.
- Treatment can be highly variable from simple tracking, aggressive surgery, embolization or radiotherapy supraselective.
- The prognosis is reserved due to the location, extension and vascular nature of the tumor, however slow development permit, even in the absence of treatment, at least 10 years of survival. For example my case with extension important on the brain after radiotherapy was still alive after 12 years.
References
- Biller HF, Lawson W, Som P, Rosenfeld R (1989) Glomusvagale tumors. Ann Otol Rhinol Laryngol 98(1 Pt 1): 21-26.
- Glenner GG, Grimley PM (1974) Tumors of the extra-adrenal para ganglion system (including chemoreceptors). In: Atlas of Tumor Pathology, Second Series. Armed Forces Institute of Pathology.
- Jackson CG (1993) Neurotologic skull base surgery for glomus tumors. Diagnosis for treatment planning and treatment options. Laryngoscope 103(11 Pt 2 Suppl 60): 17-22.
- Patel SJ, Sekhar LN, Cass SP, Hirsch BE (1994) Combined approaches for resection of extensive glomusjugulare tumors. A review of 12 cases. J Neurosurg 80(6):1026-1038.
- Li G, Chang S, Adler JR, Lim M (2007) Irradiation of glomus jugulare tumors: a historical perspective. Neurosurg Focus 23(6): E13.
- Henzel M, Hamm K, Gross MW, Surber G, Kleinert G, et al. (2007) Fractionated stereotactic radiotherapy of glomusjugulare tumors. Local control, toxicity, symptomatology, and quality of life. Strahlenther Onkol 183(10): 557-562.
- Varma A, Nathoo N, Neyman G, Suh JH, Ross J, et al. (2006) Gamma knife radiosurgery for glomusjugulare tumors: volumetric analysis in 17 patients. Neurosurgery 59(5): 1030-1036.





























