Respiratory Epithelial Adenomatoid Hamartoma (REAH): A Rare Cause of Nasal Obstruction- Case Report
Abhishek Kumar Ramadhin*
Sinai Hospital, USA
Submission: April 23, 2017; Published: May 11, 2017
*Corresponding author: Abhishek Kumar Ramadhin, Rhinology fellow, Sinai Hospital, Baltimore, USA, Tel: 4049555906; Email: drabhishekkumar4u@gmail.com; Aramadhi@lifebridgehealth.org
How to cite this article: Abhishek K R. Respiratory Epithelial Adenomatoid Hamartoma (REAH): A Rare Cause of Nasal Obstruction- Case Report. Glob J Oto 2017; 7(5): 555723. DOI: 10.19080/GJO.2017.07.555723
Abstract
Background: REAH is a rare type of hamartoma occurring in the sinonasal tract. So far only about 60 cases are documented in the literature.It is a non-neoplastic lesions constituted by a mixture of tissues primarily characterized by glandular proliferation and lined by ciliated airway epithelium.
Case outline: A 41-year male presented with a 3-year history of nasal block, and more than 1 year history of posterior nasal discharge and anosmia. Physical examination and CT PNS revealed polypoidal mass completely obliterating the left nasal cavity. It was removed surgically. Right side was near normal. Diagnosis of REAH was established by pathologist based on glandular proliferation originating from the surface of the respiratory epithelium. In2 year of follow up showed no evidence of recurrence.
Conclusion: Regardless of its rarity, REAH should be included in the differential diagnosis of a symptomatic sinonasal mass because misinterpretation of this benign lesion may lead to unnecessarily aggressive surgical intervention. Conservative surgical resection is the treatment of choice, and no recurrent, persistent, or metastatic disease has been reported to date.
Keywords: Respiratory epithelial adenomatoid hamartoma; REAH
Introduction
A hamartoma is a benign, focal malformation that resembles a neoplasm in the tissue of its origin. This is not a malignant tumor, and it grows at the same rate as the surrounding tissues [1]. It is composed of tissue elements normally found at that site, but which are growing in a disorganized mass. Respiratory epithelial adenomatoid hamartoma (REAH) is hamartomatous lesion of the nasal and paranasal sinuses. It was first described in 1995 by Wenig and Heffner [2].
Case Report
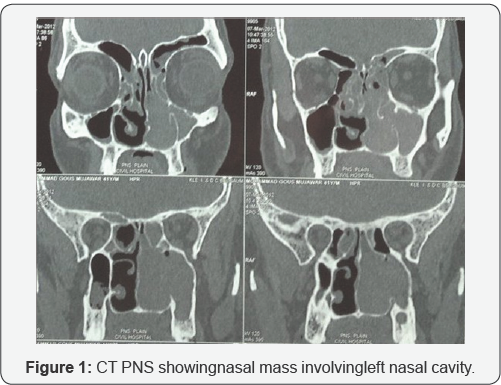
A 41-year-old male presented with a more than 3-year history of nasal blockage with more than 1 year history of posterior nasal discharge and anosmia. Symptoms were not relieved by antibiotic treatment. Routine investigations were within normal limits. Physical examination, anterior rhinoscopy and posterior rhinoscopy showed polypoidal mass occupying from the left middle meatus to choana. Computed tomography (CT) of Paranasal sinuses (Figure 1) revealed left nasal mass obliterating the nasal cavity till choana, resulting in significant upper airway compromise, there was also widening of maxillary sinus.. Right side was having mild anterior ethmoid sinusitis.
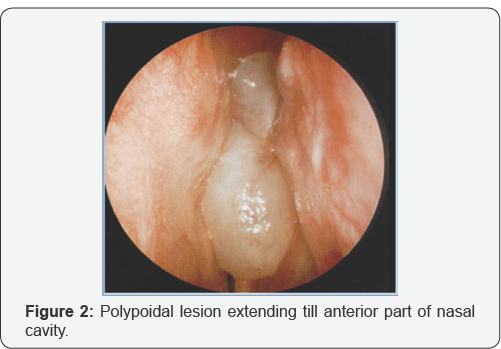
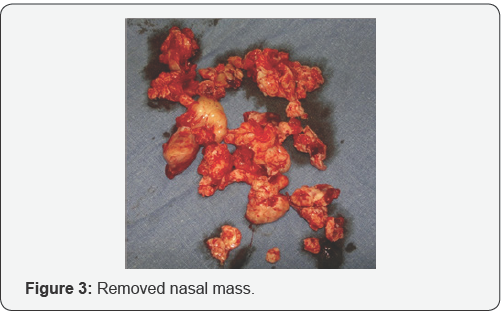
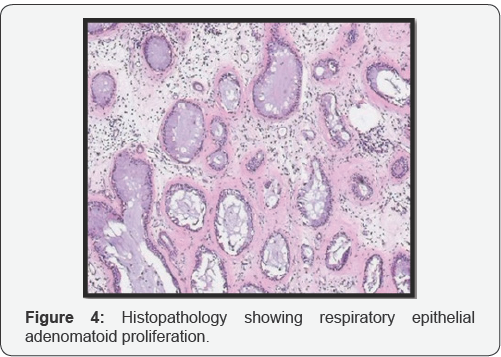
On endoscopy (Figure 2), it was a polypoidal lesion extending till anterior part of nasal cavity. Previous biopsy of the left nasal mass, reported by another pathologist, was suggestive for an inverted squamous cell papilloma. And as mass was extensive and occupying whole left nasal cavity, which was removed endoscopically. Intraoperatively the maxillary sinus was occupied by a purulent fluid and the mucosa was hyperemic and hypertrophic. As mass was going all around, it was taken out in piece meal. Mass was polypoidal with a smooth surface and rubbery consistency and a red-brown appearance (Figure 3). Histologically (Figure 4) it was found that it consists of respiratory epithelium that is continuous with the surface epithelium and the polypoidal growth is the result of respiratory epithelial adenomatoid proliferation. A characteristic finding was stromal hyalinization with a thick eosinophilic basement membrane covering the glands. The epithelial cells show no dysplasia or atypia, and the epithelium unrelated to the adenomatoid proliferations was normal. No identifiable mitotic activity or necrosis could be observed.
On immunohistochemistry, it was found to be CK7 positive and CK20 and CDX-2 negative. Ki67 was also negative.
Discussion
The sinonasal tract is a complicated anatomic site, with an exhaustive list of possible diagnoses of reactive, inflammatory, benign, and malignant lesions. The commonest are inflammatory polyps, papilloma and squamous cell carcinomas [3]. A lesion that has been more clearly defined in recent years is the nasal hamartoma especially REAH. And it should be considered in the differential diagnosis of nasal mass. Hamartomas are defined as excess or abnormal growth of normal cells or tissue native to the organ in which they occur, likely as a result of aberrant differentiation. Hemartomas may involve one or more cellular elements and are presumed to involve either error during fetal growth or postnatal disturbance of immature tissue [2].
The epithelial subtypes of nasal hamartoma are respiratory epithelial adenomatoid hamartoma (REAH), Seromucinous hamartoma, and hybrid lesions [4]. REAH, though rare, is the most common hamartoma of the sinonasal tract. It was first described by Wenig and Heffner [2] as a benign overgrowth of sub mucosal ciliated respiratory lined glands forming a polypoidal mass lesion. It may arise in any part of the nasal tract but the majority arise from the posterior nasal septum, more commonly in males between the ages of 27 and 81, who present with unilateral obstructive symptoms or epistaxis [2,4].
REAH commonly involve the nasal cavity around the septum, but other part also involves i.e. the lateral wall, middle meatus, or inferior turbinate. Involving the maxillary sinus and ethmoid is comparatively rare. Our case is second in literature to involve this area. The first one reported was by Di Carlo et al in 2006 [5]. While differentiating it from other nasallesion, histologically the glands typically are back-to-back with minimal intervening stroma, a connection to the surface epithelium and periglandular hyalinization. As shown in our histopath also.
Although the epithelium in REAH is described as multilayered, it is perhaps more appropriate to define it as pseudo stratified columnar epithelium ± goblet cells. This differentiates it from its principle differential diagnosis, Inverted papilloma, which shows a similar back-to-back nested architecture and connection to the surface, but has true multi layering by “transitional type” cells. In addition, the thick basement membrane-like material seen in REAH is absent in inverted papilloma [6]. Another important differential is Seromucinous hamartoma which is distinguished from REAH by its proliferation of glands in a lobular, clustered, or haphazard arrangement. However, both are covered by a ciliated respiratory-type epithelium [6].
The next important differential is Sinonasal Adenocarcinoma (SNAC), especially the subtype, low grade tubular adenocarcinomas, that can rarely arise in the sinonasal tract but have very much similar histopathology like REAH. It can be readily distinguished by their typical staining for CK20 and/or CDX2 [7,8]. On immunohistochemistry, REAH, IP, and CS share similar immunoprofiles (CK7+, CK20-, and CDX-2- ), contrasting with SNAC (CK7+, CK20+/-, CDX-2-/+) [8]. To date, there have been no examples of REAH with aggressive behavior or convincing examples of recurrence after complete excision [2,6].
Conclusion
Regardless of its rarity, REAH should be included in the differential diagnosis of a symptomatic sinonasal mass because misinterpretation of this benign lesion may lead to unnecessarily aggressive surgical intervention. Conservative surgical resection is the treatment of choice, and no recurrent, persistent, or metastatic disease has been reported to date.
References
- Terris MH, Billman GF, Pransky SM (1993) Nasal hamartoma: case report and review of the literature. Int J Pediatr Otorhinolaryngol 28(1): 83-88.
- Wenig BM, Heffner DK (1995) Respiratory epithelial adenomatoid hamartomas of the sinonasal tract and nasopharynx: a clinicopathologic study of 31 cases. Ann Otol Rhinol Laryngol 104(8): 639-645.
- Perez-Ordonez B (2009) Hamartomas, papillomas and adenocarcinomas of the sinonasal tract and nasopharynx. J ClinPathol 62(12): 1085-1095.
- Khan RA, Chernock RD, Lewis JS (2011) Seromucinous hamartoma of the nasal cavity: a report of two cases and review of the literature. Head Neck Pathol 5(3):241-247.
- Di Carlo R, Rinaldi R, Ottaviano G, Pastore A (2006) Respiratory epithelial adenomatoid hamartoma of the maxillary sinus: case report. Acta Otorhinolaryngol Ital 26(4): 225-227.
- Wenig BM (2005) Respiratory epithelial adenomatoid hamartoma. In: Barnes LE, Eveson JW, Reichart P, Sidransky D, (eds). World Health Organization Pathology and Genetic Head and Neck Tumours. ARC Press, France, England, p. 33.
- Franchi A, Santucci M, Wenig BM (1995) Adenocarcinoma. In: Barnes L, Eveson JW, Reichart P, Sidransky D, editors. World Health clinicopathologic study of 31 cases. Ann OtolRhinol Laryngol 104(8): 639-645.
- Ozolek JA, Barnes EL, Hunt JL (2007) Basal/myoepithelial cells in chronic sinusitis, respiratory epithelial adenomatoid hamartoma, inverted papilloma, and intestinal type and nonintestinal types in nasal adenocarcinoma: an immunohistochemical study. Arch Pathol Lab Med 131: 530-533.





























