Recurrent Nasal and Disseminated Rhinosporidiosis
Inderdeep Singh*, Anubhav Singh, Vikas Gupta, Sunil Goyal and Manoj Kumar
Department of ENT, Command Hospital, India
Submission: April 03, 2017; Published: April 11, 2017
*Corresponding author: Inderdeep Singh, Department of ENT, Command Hospital, Pune- 411040, India, Tel: +91 7767834137; Email: idgunjan@yahoo.co.in
How to cite this article: Inderdeep S, Anubhav S, Vikas G, Sunil G, Manoj K. Recurrent Nasal and Disseminated Rhinosporidiosis. Glob J Oto 2017; 6(4): 555691. DOI: 10.19080/GJO.2017.06.555691
Abstract
Rhinosporidiosis is a chronic granulomatous infective disease commonly involving the nose and occasionally involving the skin and subcutaneous tissues. We hereby report a case of nasal and disseminated rhinosporidiosis who was operated thrice and had a recurrence of disease in the nasal cavity and the nasopharynx. Biopsy from the lesions in nasal cavity proved the recurrence of disease and he was managed with endoscopic endonasal resection of the lesions along with CO2 laser assisted ablation & electrocautery assisted cauterisation of the base of the disease from the nasal cavity & nasopharynx.
Keywords: Rhinosporidiosis; Nasal; Disseminated; CO2 laser; Electrocautery
Introduction
Rhinosporidiosis is a chronic granulomatous infective disease. The disease was first described by Seeber in Argentina over a hundred years ago, after whom the causative organism was named as Rhinosporidium seeberi. The causative organism has been classified and re classified several times by the microbiologists. It belongs to a novel group of fish parasites belonging to the class Mesomycetozoa [1]. The disease is endemic in southern India and Sri Lanka. The proposed mechanisms of infection are the contact of traumatised epithelium to the natural habitat of its causative organism [1]. This explains the disease being commonly seen in people swimming in freshwater bodies, the sand being responsible for the abrasions on the mucosa and increasing the likelihood of infection [2]. The disease is characterized by the development of fleshy, pedunculated, mulberry like lesions on mucosa. It commonly involves the nasal cavity and nasopharynx but can also involve the paranasal sinuses, palate, larynx, trachea, conjunctiva, skin, subcutaneous tissues and urethra [2]. We present a case of cutaneous and disseminated rhinosporidiosis with extensive involvement of the nasal cavity and nasopharynx, which had undergone surgery thrice and had a recurrence of the disease in the nasal cavity.
Case Report
A 39 year old patient, a resident of Kerala, from southern India, presented to our OPD with complaints of epistaxis for past one year. He was a known case of nasal and disseminated cutaneous rhinosporidiosis who had been operated thrice before at different hospitals. He had a history of swimming in rivers and streams since childhood. He developed nasal obstruction and blood stained rhinorrhoea in 2003 when he presented to a tertiary care centre in Bengaluru, India. He was diagnosed as a case of nasal rhinosporidiosis and was managed surgically with medial maxillectomy by lateral rhinotomy approach in Feb 2003. He was on follow up in that hospital when he was found to have a recurrence and was managed with a revision nasal surgery in Sep 2003& was administered oral Dapsone at 100 mg/day for next 6 months. Thereafter the patient remained disease free till 2011 when he developed a wart like growth on dorsum of right foot for which he presented to a tertiary care centre in Pune. Where he was diagnosed as a case of disseminated cutaneous rhinosporidiosis. He underwent wound debridement followed by split skin grafting and was administered long term Dapsone at 100 mg/day for next6 months (Figure 1).
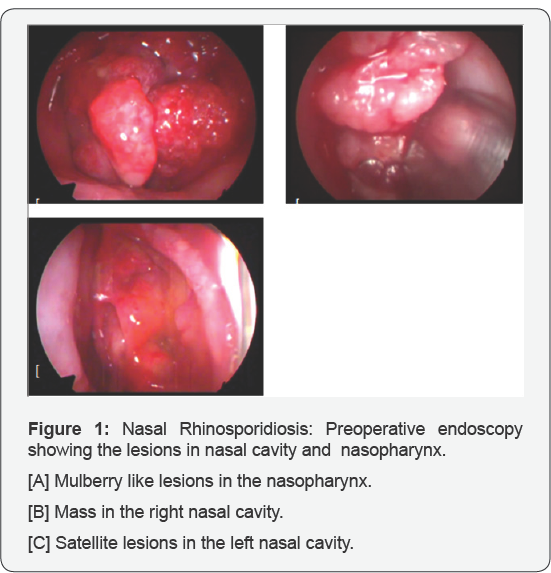
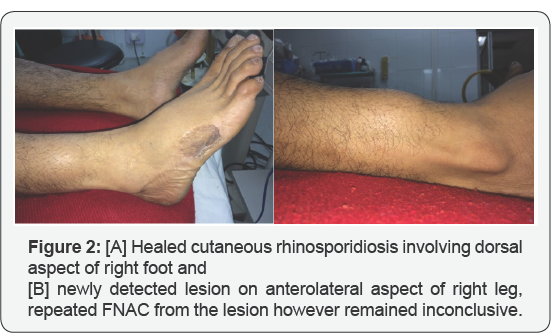
Currently, the patient presented to our OPD with complaints of epistaxis for past one year. On nasal endoscopy, irregular, mulberry like, friable masses which bled on touch were found in the roof of nasopharynx extending to the torus tuberous bilaterally. There was a large similar mass seen in right lateral nasal wall extending from the posterolateral wall of the right maxillary sinus to frontal recess. There were also satellite lesions on nasal floor and septum in the right nasal cavity and small lesions in the middle meatus and over agger nasi on the lateral wall in the left nasal cavity. He also had an operated lesion on the dorsal aspect of his right foot and a swelling on the lateral aspect of his right lower leg. Biopsy was taken from the lesions in the nasal cavity which showed numerous globular, thick walled sporangia containing numerous endospores in the subepithelium. FNAC was done from the lesion on right leg but was inconclusive. He was diagnosed as a case of nasal and disseminated cutaneous rhinosporidiosis (operated thrice, with recurrence in nasal cavity and nasopharynx (Figure 2).
The patient was managed with endoscopic endonasal nasopharynx along with wide endoscopic sinus clearance. On the right side the medial maxillectomy was extended anterolaterally and posteriorly with endoscopic microdebrider drilling and Draf 2a procedure of right frontal sinus was done. Bipolar cautery was used to cauterize the base of the lesions after disease removal in nasopharynx and lateral walls of the nasal cavities. Also, CO2 laser was used to remove the islands of disease from the septum and the nasal floor (Figure 3).
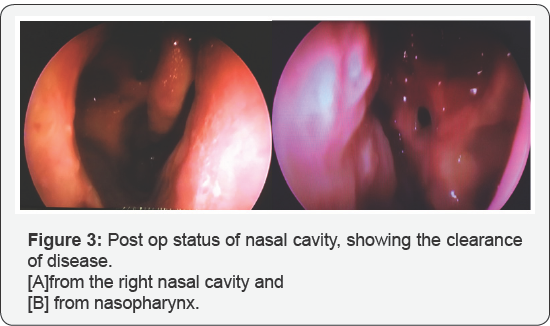
Post operatively, the patient was started on Tab Dapsone at 100 mg/day for six months. Histopathology from the specimen of diseased mucosa of the nasal cavity confirmed nasal rhinosporidiosis. Post operatively, he has been on regular follow up and is currently free of nasal rhinosporidiosis.
Results
Our patient had a recurrence of nasal lesions thrice (previously operated twice) and had a cutaneous lesion over the dorsum of right leg (operated). He was administered Dapsone for 6 months after the last surgery but still he had a recurrence of disease in the nasal cavity and nasopharynx. The patient was managed with wide excision of the disease, CO2 laser ablation and cauterisation of the base of the lesion with electrocautery to minimise the recurrence. The patient was given Dapsone post operatively to arrest the maturation of residual sporangia and accelerate the degenerative changes in them, thus further reducing the chances of recurrence.
The patient remains on our regular follow up and is currently disease free.
Discussion
Rhinosporidiosis is known to have a high chance of recurrence after medical and surgical therapy, with the recurrence rates being quoted ranging from 5-63% in literature [3]. The disease has a tendency to recur due to the difficulty in fully removing the disease surgically due to the dissemination of the microspores into the submucosa. The variation in rates of recurrence among different studies is attributable to the difference in the surgical technique [4]. The usage of electrocautery and laser for ablation of the base of the lesions is associated with a lower rate of recurrence [4]. Diamino diphenyl sulfone (Dapsone) is the only drug that has been shown to Medical management has been largely unsuccessful. The only drug that has shown some benefit in preventing the recurrence of rhinosporidiosis post surgery is Dapsone, when administered for 12 months [5].
References
- Herr RA, Ajello L, Taylor JW, Arseculeratne SN, Mendoza L (1999] Phylogenetic analysis of Rhinosporidium seeberi's 18S small- subunit ribosomal DNA groups this pathogen among members of the protoctistan Mesomycetozoa clade. Journal of Clinical Microbiology 37(9]: 2750-2754.
- Thappa DM, Venkatesan S, Sirka CS, Jaisankar TJ, Ratnakar C (1998] Disseminated cutaneous rhinosporidiosis. The Journal of dermatology 25(8]: 527-532.
- Karthikeyan P, Vijayasundaram S, Pulimoottil DT (2016] A Retrospective Epidemiological Study of Rhinosporidiosis in a Rural Tertiary Care Centre in Pondicherry. Journal of Clinical and Diagnostic Research: JCDR 10(5]: MC04.
- Aroor R, Gowda MM, Bhat VS, Bhandary SK (2015] Novel approach to rhinosporidiosis. Otolaryngology clinics: An international journal 1.
- Nair KK (1979] Clinical trial of diaminodiphenylsulfone (DDS] in nasal and nasopharyngeal rhinosporidiosis. The Laryngoscope 89(2]: 291295.





























