A Prospective Study of Complications of Tracheostomy and Management in Tertiary Care Hospital in Rural Area
Megha A Kawale*, Prashant N Keche, Surendra H Gawarle, Sneha V Bhat and Aniket Buche
Department of ENT, Shri V N. Government Medical College, India
Submission: March 03, 2016; Published: March 22, 2017
*Corresponding author: Megha A Kawale, Department of ENT, Shri V. N. Government Medical College, Yavatmal, Maharashtra, India,Tel: 8007778656; Email: kawale.megha@gmail.com
How to cite this article: Megha A K, Prashant N K, Surendra H G, Sneha V B, Aniket B. A Prospective Study of Complications of Tracheostomy and Management in Tertiary Care Hospital in Rural Area. Glob J Oto 2017; 5(4): 555667. DOI: 10.19080/GJO.2017.05.555667
Abstract
This study carried out in the department of ENT, Government medical college Yavatmal during the period of August 2012 to may 2014 was prospective evaluation of 124 patients of all ages and both sexe presenting in the department for whom tracheostomy was done for various indications.The aim of the study was to evaluate incidence of complications of tracheostomy and to suggest prevention measures for the same.The incidence of complications was 29.81% with 1.6% mortality,the commonest complication during study was surgical emphysema. The common indication for tracheostomy was artificial ventilation accounted for 68.8%.We concludes that all the complications are preventable.
Keywords: Tracheostomy; Demographic data; Indications; Complications
Introduction
Tracheostomy is one of the oldest medical proce-dures known [1]; it has been routinely used since the middle of the 19th century, when Armand Trousseau improvised the technique in order to treat diphtheria patients with dyspnea [2]. The indications of the procedure are increasing day by day. Initially all tracheostomy was carried out only to relieve the upper airway obstruction, gradually its indication became extensive and now it’s being increasingly used as temporary procedure for airway access especially for anesthetic purpose and artificial ventilation. Similarly the indication of long term or permanent tracheostomy as in cases of severe respiratory distress, sleep apnoea syndrome and terminal malignant neoplasm are also increasing [3].
The benefits of tracheostomy are not without associated risk and complications. The increasing use of tracheostomy in the past decades has resulted in parallel increase in complications; moreover little emphasis is given in medical and nursing instruction on post operative management to reduce the complications. The post trecheostomy care of the patient, involve large number of highly trained staff, elaborate machinery and expenditure of much time and money. The problems are multifold in paediatric patients including associated feeding difficulties, communication development, schooling etc. The timing of tracheostomy is very important. If the tracheostomy can be performed before severe anoxia and irreversible lung damage have set in, it greatly simplifies the post operative care and helps to reduce the forthcoming complication; in-fact the best time to do tracheostomy is when the attending physician first thinks about it in a particular case [4].
Elective tracheostomy is much more favorable than waiting for the situation to become emergency. The morbidity and mortality due to procedure is not exclusively due to procedure per se but more often due to age of the patient, general condition of the patient, whether tracheostomy is the primary procedure or part of other procedure the urgency of the procedure, the skill of the surgeon, timing of the procedure, the instrument kept in the tray, quality of the tracheostomy tube, post operative care of the patient. In pediatric patients this procedure is more challen-ging and it is associated to a higher degree of morbidity and mortality when compared to the adult population. The younger the child is submitted to the procedure, the greater is the risk of complication [5,6].
There are plenty of studies available on tracheostomy from urban centers but the same has beenlacking for rural area in our country where more than 70% of the population resides. hus this study was planned at ENT department of medical college and hospital which is situated in rural area. Hence, the goal of present study was to analyze the various indi-cations and study the prevalence of tracheostomy and compare it between emergency and planned tracheostomy. Moreover, the other objectives were to study the complications of tracheostomy and their modesof managements.
Materials and Methods
The study designed was a prospective and interventional study carried out in the Department of ENT, at tertiary care hospital, during the period from August 2012 to May 2014. Permission of Institutional Ethics Committee was taken and written informed consent was obtained from the patient or his relatives / parents (in case of minor) before starting the procedure. During the study period, a total of 124 patients (both pediatric and adult) undergoing tracheostomies for various indications were studied. All patients were properly evaluated with regard to age and sex distribution, indications of tracheostomy, whether the procedure was planned or emergency.
Technique of Tracheostomy
All infants and children were operated under general anaesthesia with endotracheal intubation while all adults, most of them with respiratory obstruction were operated under local anesthesia in the operating theatre as well as bedside as per the situation. However pediatric patients with infectious diseases like tetanus were operated bedside under local anesthesia. All patients were atrophinized by giving 0.6 ml of atropine intravenously. All sedating drugs including analgesics were avoided before establishment of airway. The neck was extended using a sand bag below the shoulder and ring pillow below the head. The neck area was cleaned with betadine and antiseptic solution and draped with sterile surgical towels. If extension of the neck increased respiratory distress then compromised position was used without full neck extension. In cases of suspected spinal injuries the extension of the neck was avoided.
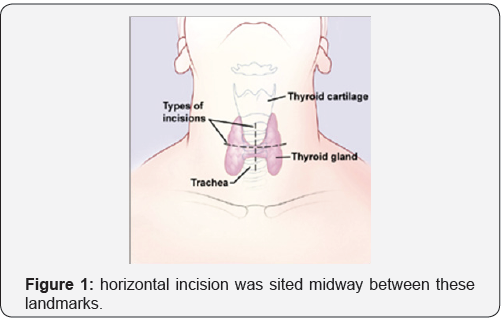
Classical surgical technique, as described in the books, was used. Local anaesthesia with 2% lignocaine and adrenaline was injected on anterior aspect of neck starting from just below the cricoids cartilage to suprasternal notch. In planned tracheostomy horizontal incision was sited midway between these landmarks (as shown in Figure 1). In a true emergency vertical skin incision in the midline after palpating the trachea, starting from just below the cricoids cartilage to just above the suprasternal notch was taken. The skin, subcutaneous tissue and fascia were retracted laterally. Then with blunt dissections, the strap muscles were separated in the midline and retracted laterally. The trachea was palpated and the position confirmed by aspiration of the air through syringe and needle, when small amount of local anaesthesia was also injected in the tracheal lumen. Then thyroid isthmus was separated from anterior aspect of trachea and retracted upward (sometimes it was divided in the midline after applying haemostatic forceps and ligated). Once the trachea was exposed, the pretracheal fascia was separated from the anterior wall of the trachea [7].
Now the procedure was slightly different in children and in adults
a) In children: The 3rd and 4th tracheal rings were identified and a small vertical incision was given between 3rd and 4th tracheal ring. A tracheal dilator was then inserted, tracheal slit dilated. The anaesthetist has to withdraw the endotracheal tube gradually till upper edge of incision of the tube is visible. A suitable size tracheostomy tube with tapes tied was then introduced carefully with the obturator. Obturator was then removed and air blast was confirmed with cotton wool or with back of hand. A suitable size sterile rubber catheter was then passed inside and suction done. The tube was then tied around the neck with tape, such that one finger can be passed between the tape and skin. The remaining wound was loosely closed with silk, a vaseline gauze dressing of the stoma around the tube was done and then the patient was shifted for further observation and proper post operative management.
b) In adult: A vertical midline incision was taken over second, third or third fourth tracheal rings. Silk stay sutures, were placed on either side of the incision line. The stay sutures were to allow tracheostomy to be held open if the tube needs to be resided prior to formation of good track and edges of the tracheostomy could be pulled up to the skin to facilitate the tube change. A proper size and type of tracheostomy tube was then inserted along with obturator. The position of tube was then confirmed by feel of air blast on the back of the hand, after removing obturator. A suitable size sterile rubber catheter was then passed inside and suction done. The tube was then tied around the neck with tape, such that one finger can be passed between the tape and skin. The remaining wound was loosely closed with silk, a vaseline gauze dressing of the stoma around the tube was done, and then the patient was shifted for further observation and proper post operative management.
A careful post operative management was done in every patient and a constant watch was kept on general condition of the patient, their nutrition and identification of any early post operative complication. Routine investigations were done during the postoperative period. Once the condition necessitating tracheostomy was overcome, attempts were made for decannulation. In case of difficult decannulation attempts were made to find cause and investigations including radiography of the chest and neck, naso-pharyngoscopy, bronchoscopy and psychiatric evaluation whenever indicated was done [3]. In patients who were tracheostomy dependent for long period, due to psychological factors, a much slower sequence of tube occlusion was followed with decannulation taking place over the course of several days or whole week [3]. In case of, death of tracheostomised patient, during hospital stay or follow up, the cause of death was noted and any association with tracheostomy was analyzed.
Observation and Result
Of the total 48,916 indoor patients, 124 patients gave the consent to participate in the study, therefore during study period total number of tracheostomy performed were 124, so prevalence rate of tracheostomy was 0.253%. The most common age group for tracheostomy found was 15-50 years of age i.e. 88 cases (70.96%), but only 5 (4.04-%) patients belonged to pediatric age group (0-14 years) and the remaining 31 patients (i.e. 25%) belonged to older age groups (51-80 years), (Figure 1). The average age of the patients was 37.8 years. Of the 124 patients, 93 (75%) were males and 31 (25%) female, so male: female ratio (M: F) was 3:1.
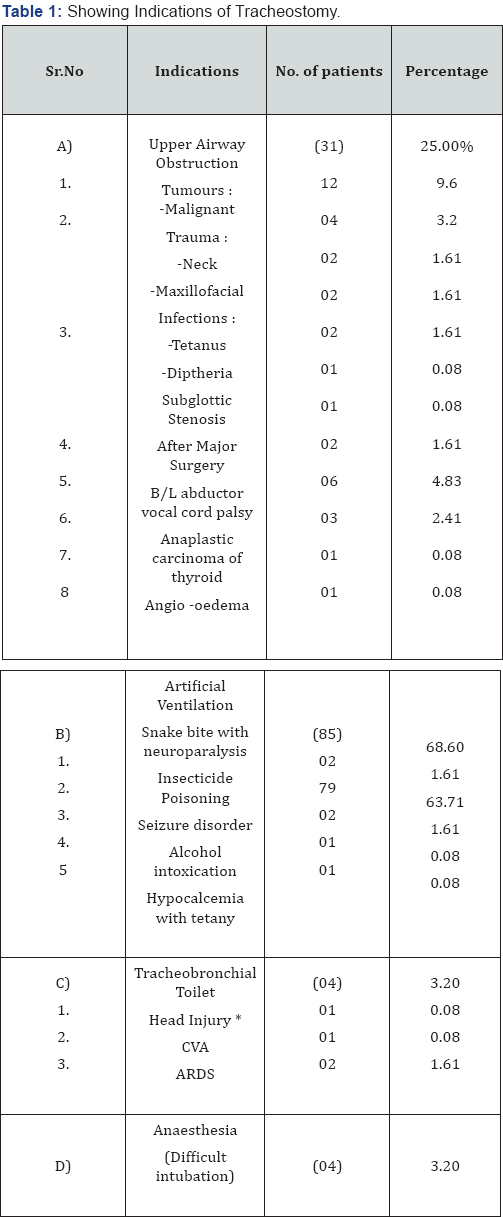
Most common indication for tracheostomy in the study was assisted ventilation (Total 85 (68.60%) tracheostomies were performed for this indication) as maximum cases (79 cases) were prolonged intubation due to respiratory muscle paralysis due to organo-phosphorus poisoning (Table 1). The prevalence of emergency and planned tracheostomy was 22.57% and 77.43% respectively. Most of the tracheostomies i.e. 113 (91.12%) both in adults and children were performed under local anaesthesia, of these 23 were in emergency and 90 were planned. Out of 11 (8.88%) cases requiring general anesthesia, 7 were planned and 4 were emergency. There was no significant difference in complication rates with type of anaesthesia used. There was no significant difference in complication rates with type of anaesthesia used. Tracheostomy was safety performed bedside, in ICU or wards provided proper aseptic conditions were maintained.
There was no significant increase in complication rates compared to operating room tracheostomies. Portex cuffed tracheostomy tubes were used in most of the cases i.e. 105 (84.68%) as compared to metallic tubes (19 cases). Metallic and noncuffed tubes were used whenever possible; to prevent the cuff related complications. In present study, thirty seven patients had either one or multiple complications; this makes the complication rate of 29.81%. Surgical emphysema (18 i.e. 14.51%) was the most common complication followed by peristomal infection in 5 cases. Major complications like trachea- esophageal fistula, trachea-innominate artery fistula and tracheal stenosis were less, as only one case of each was found in the study. Complications were more commonly encountered in emergency tracheostomies, compared to planned ones. Most of the complications were managed conservatively, (Table 2).

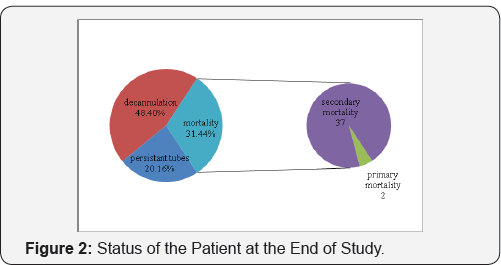
Total 39 patients died during hospital stay, making the mortality rate of 31.44%. 37 patients died of causes unrelated to tracheostomy (i.e. due to primary disease requiring tracheostomy). 2 deaths were related to tracheostomy, one due to apnoea during the procedure and one patient died due sudden massive haemorrhage due to tracheoinnominate artery fistula which occurred on 17th post-operative day during the hospital stay. Thus in present study tracheostomy specific mortality rate was found to be 1.61% (Figure 2). Out of total tracheostomies performed, 60 patients (i.e. 48.40%) were successfully dacannulated. Decannulation was not done in 25 cases as they required tracheostomy due to various causes and these cases were followed up regularly.
Discussion
statical analysis showed no significant difference in the incidence of complication between males and females,adult and paediatric patients and emergency and elective procedure. In the review of 1928 cases evaluated by Chew and Cantrell [7] in 1972 found that overall complication rate was 1.5% with mortality 1.6%.The most common complication was hemorrhage.The common cause of death was haemorrhage and displacement of tube Wood & Methison et al. [8] (1999) found that most of the late complication, can be prevented by proper surgical procedure and postoperative care.
Mehta & Chamyal [9] in their study of 100 cases, noted complications in 48% cases. Early and relatively minor complications were encountered commonly. Complications were twice more common in emergency than planned cases. No tracheostomy related deaths were noted. Zeitouni & Kost [10] studied 281 cases of tracheostomy and found a total complication rate of 24%. A statistically significant increased risk of complications was found both in emergency situation and in ICU patients. Haemorrhage was the most common intra-operative complication (2.8%). Infection was common postoperative complication (7.8%). No tracheostomy related deaths were reported.
Goldenberg et al. [11] studied 1130 cases oftracheostomy and found major complications in 49 cases (4.3%) and 8 tracheostomy related deaths (0.7%). The common complications were tracheal stenosis (21 cases), severe bleeding in 9 cases (including 2 cases of tracheo-innominate artery fistula), tracheo-cutaneous fistula (6 cases), infection (5 cases) and tracheo-oesophageal fistula (1 case). 8 deaths occurred, which included 4 cases of accidental decannulation, 2 cases of severe bleeding and 2 cases of tension pneumothorax. He further stated that complications can be minimized by avoidance of emergency tracheostomy by endotracheal intubation or cricothyroidotomy,correct surgical technique and meticulous postoperative care.
Yellon [12] reported 7 cases of totally obstructing tracheostomy associated suprastomal granulation tissue. He noted that the complications due to granulations include progression of subglottic stenosis, posterior laryngeal stenosis and supraglottic stenosis.He also noted that dislodgement of granulations may cause distal tracheal obstruction. Carr et al. [13] studied 142 cases and found granulations as the most common complication in pediatric age group (44 cases i.e. 26%). Yaremchuk [14] found that regular tube changes, at least once in two weeks, are associated with fewer complications from the granulation tissue.
Morar et al. [15] studied the impact of tracheostomy on colonization and infection of lower airway in children and found that despite high levels of hygiene, exogenous colonization without infection was common. Infection rates were lower after tracheostomy compared to translaryngeal intubation, which may be due to enhanced immunity & improved tracheobronchial toilet. Louhimo et al. [16] found post -tracheostomy tracheal stenosis in 6 patients with rate of 2.3%. The patients were managed by dilatation and tracheal resection with anastomosis. Total mortality was about 10%.
Arola et al. [17] found 9 cases of tracheal stenosis (in 812 cases) with a incidence rate of 1.1%. All cases were diagnosed within 10 weeks of extubation. Cases were managed by various methods including, resection & anastomosis (5 cases), dilatation (4 cases) and removal of granulations in (1 case). He concluded that use of low pressure cuff and avoidance of over inflation of the cuff are most important measures to prevent cuff related tracheal stenosis. Park et al. [18] found that early maturation of stoma by placement of 4 - quadrant sutures from tracheal cartilage to dermis, resulted in a decreased morbidity from accidental decannulation and did not increase the incidence of tracheocutaneous fistulas or granulation tissue formation.
The complication rate was found to be 29.83% which was comparable to study of Munir et al. [19] i.e.30%. In the study, subcutaneous emphysema and peristomal infection were the most common complications. Tracheal stenosis, tracheo- innominate artery fistula and trachea - esophageal fistula were very rarely seen. Complications were more commonly encountered in emergency tracheostomies, compared to planned ones. Thus the present study can be compared with previous studies [17,20]. Also Soni et al. [21], reported subcutaneous emphysema as the second most common complication after infection but in our study only one case of tracheal stenosis occurred in total of 124 patients. Similarly Mehta and Chamyal et al. [20], reported one patient in 100 cases and Soni et al. [21], 2 cases in 100. This was in sharp contrast to study of Goldenberg et al. [11], who reporter subglottic stenosis as the most common complication (21 cases).
In present study haemorrhage during or after the procedure was managed by proper haemostasis. Surgical emphysema was usually minimal and resolved spontaneously. Only one case of severe subcutaneous emphysema required multiple skin incisions and removal of sutures for relief. Peristomal infections were managed by appropriate antibiotics along with frequent cleaning and dressing. Tube blockage required suction after instillation of sodium bicarbonate and changing of tube if needed. Displaced tubes were reinserted in operating room after proper exposure. One case of trachea - esophageal fistula was managed conservatively by Ryle's tube insertion and keeping the patient nil by mouth till the fistula healed. Subloglottic stenosis occurred in two cases and was managed by tracheoplasty and stenting with Montgomery t-tube. Stent was removed after 6 months. Decannulation was difficult in two cases of pediatric age group due to formation of peristomal granulations. It was managed by excision of granulations followed by chemical cautery.
Conclusion
All complications are preventable as most occurred while performing a hurried procedure in a struggling patient. Hence the best method of prevention is early intervention in semi emergency situation. Moser dictum is valid that -'the best time to do tracheostomy is when you first think about it". In an emergency time should not be wasted to stop bleeding but airway should be secured. In case of cuffed tube, the cuffs should be deflated frequently to avoid pressure necrosis.
Acknowledgement
The authors would like to thank the department of ENT, surgery, other staff of operation theatre and administration of Shri V. N. Government Medical College, Yavatmal, Maharashtra, for permission to study and providing facility to carry out the work.
References
- Van Heurn LW, Brink PR (1996) The history of percutaneous tracheostomy. J Laryngol Otol 110(8): 723-726.
- Peumery JJ (2003) Armand Trousseau (1801-1867) French physician par excellence. Hist Sci Med 37(2): 151-156.
- Patrick James Bradley (1997) Management of the obstructed airway and Tracheostomy. In Editor: Scott-Brown's otorhinolaryngology, Head and Neck Surgery. (6th edn), vol Butterworth-Heinemann.
- Paul Pracy (2008) Tracheostomy. In Editor. Scott-Brown's Otolaryngology, Head and Neck Surgery. (7th edn), Vol 2. Hodder Arnold.
- Gilmore BB, Mickelson SA (1986) Pediatric tracheotomy: controversies in management. Otolaryngol Clin N Am 19(1): 141-151.
- Crysdale WS, Feldman RI, Naito K (1998) Tracheostomies: a 10-year experience in 319 children. Ann Otol Rhinol Laryngol 97: 439-443.
- Chew John Y, Robert Cantrell W (1972) Tracheostomy - complications & its management. Archotolaryngology 96(6): 538-547.
- Wood DE, Mathisen DJ (1991) Late Complications of tracheostomy. Clin Chest Med 12(3): 597-609.
- Mehta AK, Chamyal PC (1993) Tracheostomy complications and their management. Med J Armed forces of India 55(3): 197-200.
- Zeitouni AG, Kost KM (1994) Tracheostomy: A retrospective review of 281 cases. J Otolaryngol 23(1): 61-66.
- Goldenberg D, Ari EG, Golz A, Danino J, Netzer A, et al. (2000) Tracheostomy complications : A retrospective study of 1130 cases. Otolaryngol Head Neck Surg 123(4): 495-500.
- Yellon RF (2000) Totally obstructing tracheostomy associated suprastomal granulation tissue. Int Jour Pead Otorhinolaryngol 53(1): 49-55.
- Carr MM, Poje CP, Kingston L, Kielma D, Heard C (2001) Complications in pediatric Tracheostomies. Laryngoscope 111(11 Pt 1): 1925-1928.
- Yaremchuk K (2003) Regular tracheostomy tube changes to prevent formation of granulation tissue. Laryngoscope 113(1): 1-10.
- Pradeep Morar, Vivian Singh, Andrew S Jones, Julie Hughes, Rick van Saene (1998) Impact of Tracheostomy on colonization and Infection of lower airways in Children Requiring Long-term Ventilation: A Prospective Observational Cohort Study. Chest 113(1) : 77-85.
- Louhimo I, Grahne B, Pasila M, Suqtarinen T (1997) Acquired Laryngotracheal Stenosis in Children. Journal of Pediatric Surgery 6(6)
- Arola MK, Inberg MV, Puhakka H (1981) Tracheal Stenosis after Tracheostomy and after Orotracheal Cuffed Intubation. Acta Chir Scand 147(3): 183-192.?
- Park JY, Suskind DL, Prater D, Muntz HR, Lusk RP (1999) Maturation of the Pediatric Tracheostomy Stoma : Effects on complications. Ann Otol Rhinol Laryngol 108(12): 1115-1119.
- Imran Munir, Syed Mosaddaque Iqbal, Syed Abid Ali (2012) Open surgical tracheostomy and complications. Pak J Surg 28(3): 217-221.
- Mehta AK and Chamyal PC (1993) Tracheostomy complications and their management. Med J Armed forces of India 55(3): 197-200.
- Soni NK, Chatterji MS, Thind SS (1984) Tracheostomy in chindren. Indian J Pediatrics 51(408): 45-47.





























