Sinus Headaches: A diagnostic dilemma
Pablo Stolovitzky*
Department of Otolaryngology, International Affairs Coordinator-elect, American Academy of Otolaryngology-Head and Neck Surgery, USA
Submission: March 01, 2016; Published: March 07, 2017
*Corresponding author: Pablo Stolovitzky, Department of Otolaryngology, International Affairs Coordinator-elect, American Academy of Otolaryngology-Head and Neck Surgery, Emory University School of Medicine, Atlanta, Georgia, USA, Tel:770-851-6311;Email:stol@ENTOFGA.COM
How to cite this article: Pablo S. Sinus Headaches: A diagnostic dilemma. Glob J Oto 2017; 4(5): 555646. DOI: 10.19080/GJO.2017.04.555646
Mini Review
Sinus headaches present diagnostic and therapeutic challenges. This mini review will discuss why symptoms commonly interpreted as “sinus headaches or sinusitis” are frequently misdiagnosis of migraines. The high rate of underdiagnosed migraine is of concern because migraine, when not adequately diagnosed and treated, can impair the quality of life and daily functions of patients. Migraines are misdiagnosed because of its association with pain in the sinus region and therefore, confused with sinusitis by patients and physicians. We see patients daily in consultation for pain in the sinus area. Patients are convinced they have a sinus infection, yet the physical exam, nasal endoscopy and CT scan are absolutely normal.
We need to ask ourselves: Is there a causal relationship between recurrent sinus headaches and sinusitis?
Why do patients with sinus headaches think they have sinusitis? A large quantitative market research study was conducted among 810 patients, 649 of which met the International Headache Society (IHS) criteria for migraine but were not necessarily diagnosed. The study assessed the prevalence of patient-labeled headaches among these migraineurs. Sixty percent of the patients reported sinus headaches as their diagnosis, but when strict IHS diagnostic criteria was applied, these patients’ diagnosis was migraine [1]. Eross re-evaluated sinus headaches by applying strict diagnostic criteria and found that 86% of these patients had migraine or probably migraine andonly 3% had acute rhinosinusitis [2].
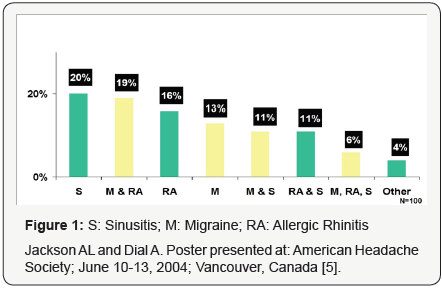
The Landmark Study looked at the prevalence and diagnosis of migraine in 377 patients. S.J. Tepper reported similar findings to those reported by Eross. Ninety four percent of the patients had migraine or probable migraine, 3% had episodic tensional headache and 3% had other diagnosis including acute rinosinusitis [3]. Data from the American Migraine Study II sheds light on the question of why more than half of migraineurs remain undiagnosed. These data show a substantial proportion of undiagnosed migraineurs report being diagnosed with other headache types. This result raises the possibility that migraine was overlooked in favor of tension headache (32%) and sinus headache (42%) among this sample of migraineurs [4]. Figure 1 shows that nearly half of the patients referred for otorhinolaryngological consultation for sinus headache had migraine Lal et al. [5] conducted a retrospective chart review of “sinus” headache/pressure/pain patients and concluded that a high symptom-burden/SNOT-22 scores and high psychosocial symptoms should raise suspicion of primary headache disorderswhen endoscopy and/or CT results do not correlate with symptoms [6].
Diagnostic Criteria of Headache (ICHD) [7]
Headache classification was determined using the ICHD-II criteria established by the International Headache Society (IHS) [7]
“Definitive Migraine”
- At least five lifetime headache attacks lasting 4-72 hours)
- With at least two of the qualifying pain characteristics
- unilateral location,
- pulsating quality
- moderate or severe pain intensity)
- aggravation by routine physical exertion
- At least one of the associated symptoms
- nausea and/or vomiting
- photo/phonophobia
- not readily attributable to another central nervous system disorder or head trauma
- Glaxo Smith Kline (2001) Migraine Consumer Segmentation Study.
- Eross E, Dodick D (2003) Non-infectious sinus headache (NISH): evidence for new primary headache disorder. Cephalalgia 23: 581-762.
- (2004) Landmark Study Headache. 44: 856-864.
- Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF (2001) Migraine diagnosis and treatment: results from the American Migraine Study II. Headache 41(7): 638-657.
- Jackson AL, Dial A (2004) Poster presented at: American Headache Society. Vancouver, Canada.
- Lal D, Rounds AB, Rank MA, Divekar R (2015) Clinical and 22-item Sino- Nasal Outcome Test symptom patterns in primary headache disorder patients presenting to otolaryngologists with “sinus” headaches, pain or pressure. Int Forum Allergy Rhinol 20: 1-9.
- Olesen J (2004) The International Classification of Headache Disorders (2nd edn). Cephalalgia 24 Suppl 1: 9-160.
- Cady, Schreiber (2004) OtolaryngolClin N Am 37: 267-288.
Probable Migraine” was designated if all but one of the definitive migraine criteria were fulfilled, excluding headaches attributable to another disorder.
Migraine PathophysiologyHypothesis
A. Presentation of Migraine as ‘‘Sinus Headache’’
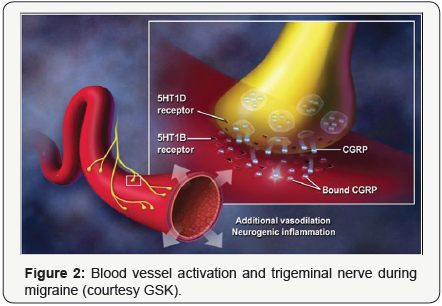
For many years migraine was thought to be a vascular disorder, a process involving constriction of cranial blood vessels followed by reflex dilation. Researchers have since demonstrated that migraine involves more than blood vessels. It also involves trigeminal nerve endings that surround the blood vessels, inflammatory neuropeptides released from the trigeminal nerve endings and the brain stem. Calcitonin Gene- Related Peptide (CGRP), one important inflammatory mediator, is a neuropeptide released from trigeminal nerve endings during migraine. It is a potent vasodilator and has been linked to the pain in migraine. Triptans are believed to interrupt the migraine process by stimulating 5HT1b receptors on cranial blood vessels to reduce the pain-inducing vasodilation and by stimulating the 5HT1d receptors on trigeminal nerve endings that surround the blood vessels to block the release of neuropeptides (e.g., CGRP) that cause further vasodilation and neurogenic inflammation (Figure 2).
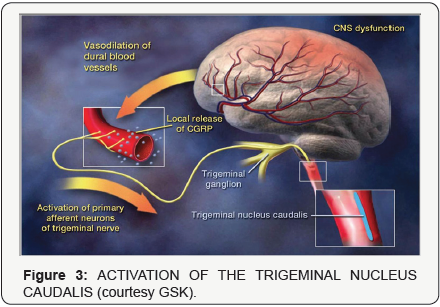
Although the cause of migraine is not fully understood, it is thought to begin when an episode of diffuse neural dysfunction leads to a cascade of events including vasodilation of cerebral blood vessels and activation of the trigeminovascular system. The dilated cerebral blood vessels cause irritation to the trigeminal nerve endings. This irritation results in the releaseof vasoactive neuropeptides such as CGRP and substance P from the trigeminal nerve endings which exacerbate vasodilation by producing neurogenic inflammation. Pain impulses from the dilation and inflammation are transmitted from the trigeminal nerve to the trigeminal nucleus caudalis in the brain stem (Figure 3).
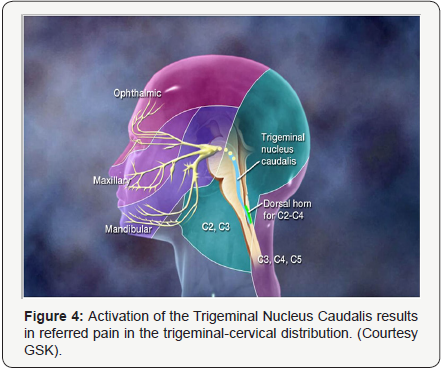
The trigeminocervical network, which includes the 3 branches of the trigeminal nerve (the ophthalmic branch (V1), the maxillary branch (V2), and the mandibular branch (V3)) as well as the sensory nerves for the posterior head and neck (C2, C3, C4, C5) feed into the Trigeminal Nucleus Caudalis (TNC). Activation of the TNC may result in referred pain to various locations along the trigeminocervical network. Pain may be perceived on one or both sides of the head, the eyes or sinuses, and the posterior head and neck (Figure 4). The superior salivatory nucleus, which is part of the cranial parasympathetic nervous system, lies in close proximity to the TNC. Activation of the TNC can cause reflex cranial parasympathetic activation through the superior salivatory nucleus. Cranial parasympathetic activation can result in sinus-like symptoms such as rhinorrhea, congestion and lacrimation (Figure 5).

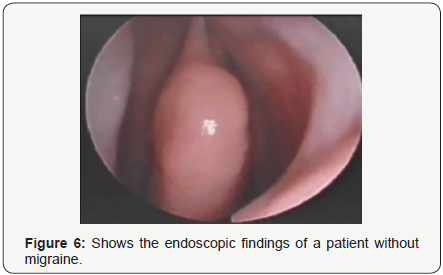
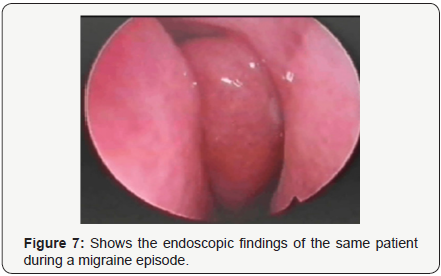
Cady and Schreiber published their endoscopic findings in a patient before and during a migraine episode [8]. This is from nasal endoscopy done on a single patient before they have a migraine and during an attack with sinus symptoms. No vasoconstrictor or analgesic was used prior to the endoscopy (Figures 6 & 7).
Conclusion
Migraine remains underdiagnosed both because of failure to recognize it and because of misdiagnosis of migraine as another headache type. Many of the undiagnosed migraineurs have been diagnosed with sinus headache because of the presence of symptoms such as bilateral, non- throbbing pain, sinus pain and pressure, nasal congestion, runny nose and lacrimation. In addition to the traditional symptoms of migraine, new studies show that these symptoms are common in migraine and may explain why migraine is sometimes misdiagnosed as sinus headache.
In order to be treated effectively, headaches need to be diagnosed accurately. In migraine, achieving a pain-free outcome is the top treatment goal of patients. The majority of patients with sinus pain are misdiagnosed as sinusitis because the stimulation of the trigeminal branches and reflex parasympathetic stimulation produces congestion, rhinorrhea and lacrimation. Otorhinolaryngologists should learn to diagnose and treat migraines since we see a large number of these patients. We should avoid performing sinus surgery in these patients if there is no sinus pathology because most these patients do not get any relieve of their migraines after surgery.





























