Local Anaesthesia of Nose and Nasal cavity- A Review
Balasubramanian Thiagarajan*
The Tamilnadu Dr. MGR Medical University, India
Submission: February 13, 2017; Published: March 06, 2017
*Corresponding author: Balasubramanian Thiagarajan, The Tamilnadu Dr. MGR Medical University, Tamilnadu, India, Email:drtbalu@gmail.com
How to cite this article: Balasubramanian T. Local Anaesthesia of Nose and Nasal cavity- A Review. Glob J Oto 2017; 4(4): 555643. DOI: 10.19080/GJO.2017.04.555643
Introduction
Local anaesthesia is defined as any technique that induces loss of sensation in a specific part of the body. Even though this definition is correct in general terms local anaesthesia also causes loss of other sensations as well. Local anaesthesia can be induced by drugs. Ideal local anaesthesia for surgical treatment purposes should be reversible. The first local anaesthetic to be used was Cocaine. Cocaine was isolated from Coca leaves. It was originally popular with residents of Andes mountain area. Australian surgeon Koller [1] was the first to perform a surgery in the eye after administration of cocaine. This caused a spurt in the use of cocaine as local anaesthetic agent in United States and Great Britain. Soon the complications of cocaine became evident including its addictive potential. Initially it was commonly used as a local anaesthetic agent by dentists to be followed by otolaryngologists as topical anaesthetic agent in the nasal cavity.
This drug was widely preferred in nasal surgeries because of its associated vasoconstrictive property. Initially cocaine for otolaryngological use was available in two concentrations (4% and 10%). Since nasal mucosa provided a vast absorptive surface the incidence of toxicity following use of cocaine was rather high [2]. Despite the high levels of toxicity Halstead started to use it as nerve block for his surgeries in United States in 1885. The irony was Halstead himself became an addict to cocaine due to his self experimentations [3]. Search for safer synthetic alternatives lead to the synthesis of the first synthetic derivative to cocaine. It was named as Procaine (1904). Lidocaine which is still commonly used local anaesthetic was developed by Lofgren and was put to extensive use during the Second World War.
Mechanism of action of Local Anaesthetics
Local anaesthetics induce anaesthesia by inhibiting excitation of nerve endings / blocking conduction in peripheral nerves. This is usually caused due to reversible binding and inactivation of sodium channels. Normal functioning of sodium channels in a nerve is important for depolarization process which causes nerve conduction.
Chemical Structure of local anaesthetics
All local anaesthetics have an intermediate chain linking an amine to one end and aromatic ring on the other. The amine end is hydrophilic and the aromatic end is lipophilic. Chemical variations to amine end / aromatic end causes changes to the chemical activity of the drug.
In chemical terms there are two classes of local anaesthetics available:
- Amino amides: This group has an amide link between the intermediate chain and the aromatic end
- Amino esters: This group has an ester link between the intermediate chain and the aromatic end
Commonly used amino amides
- Lidocaine
- Mepivacaine
- Pilocarpine
- Bupivacaine
- Ropivacaine
- Etidocaine
Commonly used amino esters
- Cocaine
- Procaine
- Tetracaine
- Benzocaine
Activity of Local anaesthetics
Activity of local anaesthetics depends on their:
- Lipid solubility: Potency is directly related to lipid solubility. It should be remembered that 90% of nerve cell membrane is composed of lipid [3].
- Protein binding: Is usually related to the duration of action. If the drug binds firmly to the protein of sodium channel the effect of local anaesthesia would be longer.
- Ionization at physiological pH: Chemically local anaesthetics exist in ionized and non ionized forms. The proportion of these two forms depends on the pH of the environment. The non-ionized form of local anaesthetic is that one that is capable of diffusing across nerve cell membrane causing local anaesthesia. Local anaesthetics with larger amounts of non-ionized components are capable of inducing faster anaesthesia. Ideally local anaesthetic drugs should be available in non-ionized form in physiologic pH. A decrease in pH shifts the local anaesthetic drug to its ionized form there by reducing its potency. This is the reason why the action of local anaesthetics is suboptimal in inflamed tissues. Addition of sodium bicarbonate to the local anaesthetic drug would increase its potency as this would increase the pH at the tissue level.
- Vasodilating properties: All local anaesthetics except cocaine are known to cause vasodilatation. Vasodilatation occurs due to relaxation of peripheral arteriolar smooth muscle fibres. Greater vasodilatation causes rapid absorption of the drug thereby shortening its action. Hence vasoconstrictors like adrenaline are added to local anaesthetic drug to increase their duration of action.
Ideally it is the duty of the surgeon to find the smallest dose of local anaesthetic drug possible whose local anaesthetic effect could last the entire duration of surgery. It should be stated here that addition of adrenaline increases the margin of safety and prolongs the duration of action of the drug. To increase the shelf life of local anaesthetic drugs the pH is deliberately kept in the range between 4-5. This when injected will not only reduce the potency of the drug but also can cause undesirable burning sensation if administered in awake patients. Addition of sodium bicarbonate 1cc of a 1 mEQ/ml solution for every 9 ml of local anaesthetic taken will not only increase the potency of the drug but also would minimize the burning sensation.
Anaesthesia of nose and nasal cavity are indicated for various diagnostic and surgical procedures involving the nose. Some of these indications include:
- Insertion of Ryles tube
- Diagnostic nasal endoscopy
- Repair of fracture nasal bone [4]
- Nasal packing for epistaxis
- Foreign body removal
- Abscess drainage / Septal hematoma drainage
- Nasotracheal intubation [5]
Types of anaesthesia
- Topical anaesthesia using 4% topical xylocaine / 10% typical xylocaine spray3
- Infiltration anaesthesia using 2% xylocaine
- Regional blocks
- Combination of these
Innervations of nose
For effective administration of local anaesthesia a complete understanding of sensory innervation of nose and nasal cavity is a must. Innervations of nose can be divided into:
- Innervations of mucosa within the nasal cavity
- Innervations of external nose and its skin covering
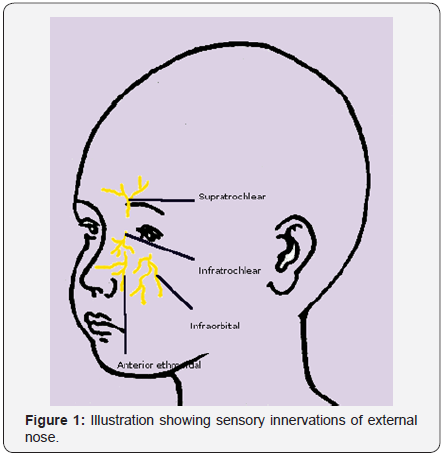
Sensory innervations of external nose
External nose and its skin lining is innervated by ophthalmic and maxillary divisions of trigeminal nerve.
Superior aspect of the nose is supplied by - Supratrochlear and Infratrochlear nerves (branches of trigeminal nerve) and external nasal branch of anterior ethmoidal nerve.
Inferior and lateral parts of the nose - is supplied by infraorbital nerve(Figure 1).
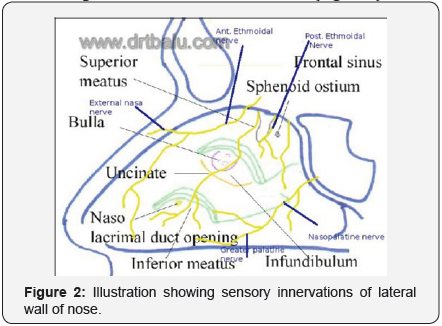
Sensory innervations of interior of nasal cavity:
- Superior inner aspect of the lateral nasal wall is supplied by anterior and posterior ethmoid nerves
- Sphenopalatine ganglion present at the posterior end of middle turbinate innervates the posterior nasal cavity
- Nasal septum is supplied by anterior and posterior ethmoidal nerves. Sphenopalatine ganglion also contributes to the sensory supply to the nasal septum via its nasopalatine branch.
- Cribriform plate superiorly holds the olfactory special sensation fibers.
Mucosal surface anaesthesia can be achieved by
- Using 10% xylocaine nasal spray: Topical surface anaesthesia just lasts for about 45 mins. This type of anaesthesia is preferred while performing diagnostic nasal endoscopy / minor procedures involving the nasal cavity like nasal packing.
- Nasal packing using cottonoids / pledgets soaked in 4% xylocaine mixed with 1 in 10000 adrenaline is useful for performing minor surgical procedures inside the nasal cavity. Cottonoids are comparatively better than cotton pledgets. Each nasal cavity should be packed with 3 packs. One is placed in the floor of the nasal cavity, the next one is placed over it to encroach into the middle meatus and the last one is placed above the second one to anaesthetize the frontal recess area. Presence of adrenaline in the mixtureshrinks the nasal mucosa and prolongs the duration of topical anaesthesia.
- Infiltration anaesthesia is preferred while performing surgeries inside the nasal cavity. 2% xylocaine mixed with 1 in 10000 adrenaline is used for infiltration. Infiltration can be used to anaesthetize the anterior ethmoidal nerve, infraorbital nerve via the canine fossa. This is very useful during reduction of fracture nasal bone(Figure 2).
Caution: While using 4% topical xylocaine for anaesthesia the maximum volume of the drug used should not exceed 7 ml. Pharyngeal wall mucosa gets anaesthetized when pledgets dipped in 4% xylocaine is used to pack the nose. This may cause the patient to aspirate blood and secretions. Periodical suction should be applied to the patient’s throat while performing nasal surgeries under local anaesthesia.
References
- https://www.ncbi.nlm.nih.gov/pubmed/11895133
- http://www.pbm.va.gov/clinicalguidance/criteriaforuse/benzocaine.
- http://emedicine.medscape.com/article/873879-overview
- Waldron J, Mitchell DB, Ford G (1989) Reduction of fractured nasal bones; local versus general anaesthesia. Clin Otolaryngol Allied Sci 14(4): 3577-3579.
- Techanivate A, Leelanukrom R, Prapongsena P, Terachinda D (2007) Effectiveness of mouthpiece nebulization and nasal swab stick packing for topical anesthesia in awake fiberoptic nasotracheal intubation. J Med Assoc Thai 90(10): 2063-2071 .





























