“LEGO®Man” Creates Asymptomatic Persistent Esophageal Foreign Body Identifiable On Barium Esophagram
Nuleema Tummala1 and Adele K Evans2
1Department of Otolaryngology - Head & Neck Surgery, Wake Forest School of Medicine, United States
2Department of Pediatric Otolaryngology, Salem Pediatric Ear and Airway Center, USA
Submission: February 08, 2017; Published: February 23, 2017
*Corresponding author: Adele K Evans, Pediatric Otolaryngology,Salem Pediatric Ear and Airway Center, 1677 Westbrook Plaza Dr, Suite 180, United States, NC 27103, Tel:336-245-4972 ; Fax: 336-955-2480; Email:adeleevans@SPEAC-ORL.COM
How to cite this article: Nuleema T, Adele K E. “LEGO®Man” Creates Asymptomatic Persistent Esophageal Foreign Body Identifiable On Barium Esophagram. Glob J Oto 2017; 4(2): 555631. DOI: 10.19080/GJO.2017.04.555631
Introduction
Pediatricians and emergency room specialists are routinely faced with the challenge of management of young patients who are suspected to have accidentally swallowed foreign objects. These objects can become a pathologic esophageal or airway foreign body. The persisting esophageal foreign body, one that does not pass spontaneously through the gastrointestinal tract, is suspected based on patient history and clinical symptoms. These often include regurgitation, drooling and unrelenting discomfort worsened by attempts to swallow. However, there are times when persisting esophageal foreign body is asymptomatic. This report describes the utility of using a contrasted esophagram in identifying the presence of a large but asymptomatic persistent radiolucent esophageal foreign object, a ‘‘Lego Man’’.
Case Presentation
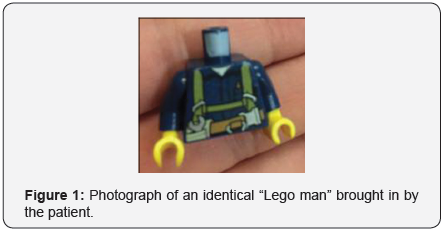
A 10-year old male whose past medical history was significant only for Attention Deficit Hyperactivity Disorder presented to the Emergency Department six hours after having swallowed a “Lego Man” that he felt may have passed completely. Apart from mild generalized throat discomfort, he was asymptomatic at the time of presentation and at the time of specialty examination: he had no respiratory complaints, no drooling, no dysphagia, nor chest pain. He brought with him an example of the “Lego Man” (Figure 1).
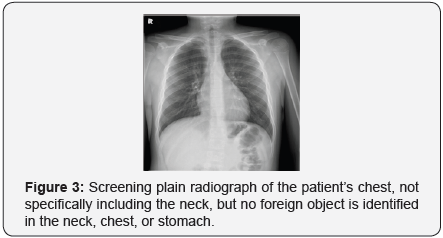
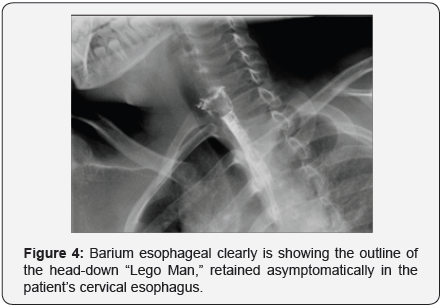
Because it was unclear if this material was radio-opaque or radio-lucent, a plain film of an identical ‘‘Lego Man’’ alone on a radiographic plate was obtained. This demonstrated a partially radiopaque foreign object (Figure 2). Because of the possibility of some degree of radio-opacity based on the plain film, the emergency department obtained a formal posterior-anterior chest radiograph, a formal lateral chest radiograph, and then a KUB radiograph to evaluate for a possible enteric “Lego Man.”

These imaging studies did not reveal the location of the foreign object (Figure 3).
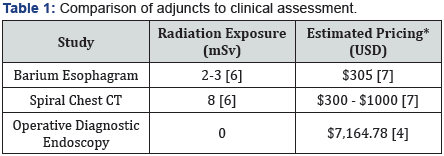
In this case of an asymptomatic patient with clearly negative imaging and work up with overall satisfied parents, the provider was met with the diagnostic dilemma of observant discharge versus recommendation for further pursuit of the foreign body with a computed-tomography (risks being cost and radiation exposure) or operative diagnostic esophagoscopy, (risks being cost, anesthesia risks and a potentially unnecessary invasive procedure). A third diagnostic option was entertained: obtaining barium esophagram. Considering the large size of the foreign object and the relatively lower cost and X-ray exposure associated with this imaging modality, the decision was made to pursue this option. This imaging study clearly outlined the “Lego Man,” persisting in the cervical esophagus (Figure 4).
The patient subsequently underwent therapeutic operative esophagoscopy in the operating room. This revealed the “Lego Man” lodged in the cervical esophagus, just below the upper esophageal sphincter. The “Lego Man” was removed atraumatically with very scant excoriation of the esophageal mucosa. The patient did well in the recovery room and was discharged home in stable condition.
Discussion
Pediatric specialists routinely face the challenge of evaluation and management of young patients who are suspected to have accidentally swallowed potentially dangerous foreign objects. The persisting esophageal foreign body is suspected based upon a parent-provided patient history (most often) and on active clinical symptoms, which usually include obvious regurgitation, drooling and unrelenting discomfort worsened by attempts to swallow. However, there are times when persisting esophageal foreign body is asymptomatic. In clinical practice, every otolaryngologist has removed meat impacted for days on end; our practice has reported disc batteries sitting for days [Evans & Panella]; and this investigator has observed stricture with proximal esophageal dilation after a dime was present for an estimated 6 months. In the setting of an unreliable history and / or an asymptomatic patient, the diagnostic challenge is further increased [1,2].
Many foreign objects will pass through the alimentary tract without causing any harm, however there is a real risk of morbidity and even mortality with any esophageal foreign object. Our greatest concern remains the disc battery, wherein “time is tissue” and sequelae are significant, i.e. tracheoesophageal fistula, aortic rupture. However, acute upper airway obstruction, failure to thrive and aspiration of refluxate into the airway with subsequent aspiration pneumonia remain important consequences of the undiagnosed esophageal foreign body. Therefore, each patient should be appropriately worked up and managed to avoid these, and other, possible sequela.
Beyond history and physical examination, imaging studies increasingly play a critical role in the first line of assessment as a part of the medical decision making process. Used appropriately, imaging can guide further management [1]. The vast majority of esophageal foreign bodies are radiopaque (coins) [3], and the utility of plain radiograph for this diagnosis is well documented. Radiolucent foreign objects, such as plastic, organic material and glass, present greater challenge with plain films that can provide a false sense of reassurance. The internationally popular Lego is considered a radiolucent plastic toy, based upon its relative invisibility on radiograph at physiologic settings [4]. Retrospectively, our radiologists were able to capture “Lego Man’s” image with the potentially false reassurance of radioopacity because the image was obtained separate from the patient and the X-ray was coned specifically for the toy.
Studies have suggested that spiral CT serves as an alternative imaging modality to identify the presence of radiolucent foreign objects in the esophagus or trachea [5]. Spiral CT does require a cooperative child and a thorough interpretation. As an alternate, providers may forego imaging and proceed directly to the operating room. This raises several concerns in the parent-doctor discussion. One concern is NPO-status and airway management in the acute foreign body. Another is the parental concern for performing a potentially unnecessary and possibly costly invasive diagnostic test.
In the modern era, parents are carefully following their child’s risk: benefit analysis regarding studies and interventions. Publications reporting increased concerns for unnecessary anesthesia experience permeate both the scientific literature and the lay press. As the deductibles for third-party payers have increased, parents have more carefully rationed the distribution of the healthcare dollars. And culturally, the last 20 years have demonstrated a shift away from paternalistic medicine towards joint medical care planning in partnership with parents. These interactive forces add challenges for the provider who is working to make a safe, efficient, and cost-effective decision regarding the optimal acute evaluation and management of the asymptomatic patient (Table 1).
It is well documented that pricing varies with locality and the contracted payor-biller relationship. This reflects assessments of billing patterns prior to institution of “facility fee” charges in addition to surgical anesthetic and operative time fees.
Conclusion
This case illustrates that even an asymptomatic patient deserves a high index of suspicion for persistent esophageal foreign body, and barium esophagram can be critical in identifying the presence of such an object for surgical decision making. Though availability of urgent fluoroscopy may be limited, there is overall lower radiation exposure than a CT scan [6-8], it is less costly than a negative operative endoscopy [3], and it may be safer than observant discharge.
References
- Sink JR, Kitsko DJ, Mehta DK, Georg MW, Simons JP (2016) Diagnosis of Pediatric Foreign Body Ingestion: Clinical Presentation, Physical Examination, and Radiologic Findings. Ann Otol Rhinol Laryngol 125(4): 342-350.
- Pugmire BS, Lim R, Avery LL (2015) Review of Ingested and Aspirated Foreign Bodies in Children and Their Clinical Significance for Radiologists. Radiographics 35(5): 1528-1538.
- Goins JL, Evans AK (2011) Retrieval of a penny from the pediatric esophagus: a cost analysis. Int J Pediatric Otohinolaryngology 75(12): 1553-1557.
- Saps M, Rosen J, Ecanow J (2014) X-ray detection of ingested nonmetallic foreign bodies. World J Clin Pediatr 3(2): 14-18.
- Applegate KE, Dardingr JT, Lieber ML, Herts BR, Davros WJ, et al. (2001) Spiral CT scanning technique in the detection of aspiration of LEGO foreign bodies. Pediatr Radiol 31(12): 836-840.
- The Health Physics Society. “Radiation Exposure from Medical Diagnostic Imaging Procedures”. PDF File.
- Health Care Blue Book Fair Pricing Index.
- Panella NJ, Kirse DJ, Pranikoff T, Evans AK (2013) “Disk battery ingestion: case series with assessment of clinical and financial impact of a preventable disease.” PediatrEmerg Care 29(2): 165-169.





























