Cholestaetoma- Surgical Steps Revisited With A Novel Technique of Cavity Closure
Pankaj Srivastava1* and Rohit Mehrotra2
1Director, Pankaj ENT hospital, India
2Professor, GSVM Medical College, India
Submission: February 06, 2017; Published: February 15, 2017
*Corresponding author: Pankaj Srivastava, Director, Pankaj ENT hospital, 56-C Singar Nagar, Alambagh, Lucknow, India, Tel:9984477770; Email:drpankajsrivasthava@rediffmail.com
How to cite this article: Pankaj S, Rohit M. Cholestaetoma- Surgical Steps Revisited With A Novel Technique of Cavity Closure. Glob J Oto 2017; 4(1): 002 555626. DOI: 10.19080/GJO.2017.04.555626
Abstract
Objective: Open mastoid cavities still have problem of recurring discharge. We have here tried to point those factors and suggest a novel method of closing the cavity so that these cavity problems are minimized.
Study design: Retrograde study was done on 218 canal wall down mastoidectomies with standard method and new method of closing the cavity and results were analysed.
Main outcome measure: Primary outcome measure was cavity healing.
Results: There was significant improvement in early and complete drying of mastoid cavities with new technique.
Conclusion: The cavity closure technique which is close to natural anatomy gives early and stable dry Mastoid cavity.
Keywords:Cholestaetoma; Canal wall down; Mastoidectomy; Mastoid cavity
Introduction
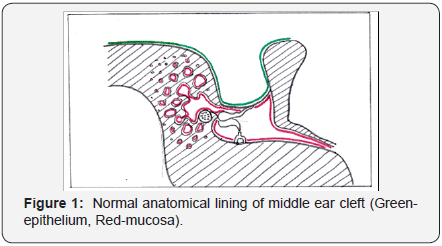
Anatomically there is a middle ear cleft comprising mastoid air cells, antrum, aditus, middle ear and Eustachian tube all lined by contiguous mucosa which secretes mucus and is drained finally to Nasopharynx. Other being Canal skin and Tympanic membrane epithelium which exfoliates epithelium and is open to exterior (Figure 1). After surgery if these natural cavities lose their anatomy, operated cavity will no longer be dry or healthy in long term. If skin goes inside middle ear cleft it is Cholestaetoma, if mucosa grows over epithelium it is granulations and if middle ear cleft is collapsed it will also granulate as it happens if fascia is directly laid over exposed air cells or skin grows over residual air cells in mastoid cavity (Figure 2).

Materials and Methods
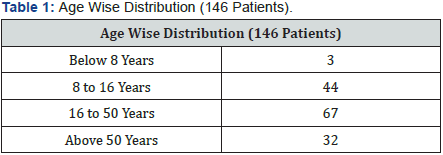
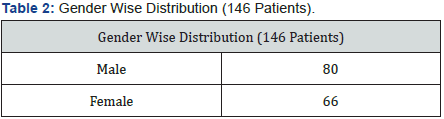
A retrograde study was done in 218 Tympanomastoidectomies in adults and children from both gender (Tables 1 & 2), from all regions of India who got operated in Pankaj ENT Hospital. Cases of Attic perforation, cholestaetoma, attic granulations (Table 3), who underwent canal down Mastoid surgery were included in this study. Video recordings of all surgery with operative notes were kept. Those cholestaetoma cases that did not need canal down procedure were excluded from the study.

All cases were reviewed with particular attention to the per operative findings, operative procedure & post-operative results. Operative details were reviewed with video recording when any problem was encountered in post operative visit, the problems like discharge, granulation, sloughing etc. were reviewed with operative steps and analyzed and were tried to correct in further surgeries, till we reached a method which provided satisfactory and consistent results.
In our setup the operations planned in any attic disease is Tympanomastoidectomy - it means complete Mastoidectomy with examination and procedure whatever is needed (that is decided as per operative findings) in middle ear including ossiculoplasty. All the cases were done postaurally; the incision was given at postaural crease only. Subcutaneous dissection was along the conchal cartilage so that all the subcutaneous tissues and periosteum is saved posteriorly which will ultimately fall in the cavity post operatively and the meatoplasty flap will be thin and easily inverted by sutures. A ‘T’ shaped incision is given at Periosteom saving any injury to Temporalis muscle. Posteriorly subcutaneous tissue is dissected from skin flap at this stage only to prevent bleeding at the time of closure and this separated subcutaneous flap will fall in mastoid cavity in the last. Complete Mastoidectomy is done lowering facial ridge to its lowest with special attention to anterior attic and saucerisation of margins to reduce cavity size. Near 360-degree elevation of canal skin is done leaving mucosal layer for overlay grafting.
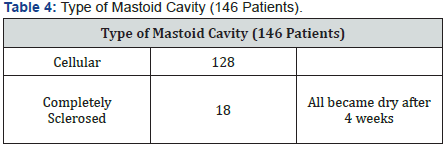

Now two types of mastoid cavities can be found after Mastoidectomy (Table 4) - First -completely sclerosed - means there remains no visible mastoid cells at the floor-here a large and thin (large to cover all exposed mastoid bone and thin to reduce its nutritional requirement) so that is becomes live early and for sure (Figure 3). Fascia is lined from anterior elevated skin 2 mm above annulus to cover the entirecavity. If there are out pouchings it can be filled with small amount of bone pate to give circular cavity. (This type of sclerosed mastoid is very less in number as it depends on the duration of inflammatory process, which leads to sclerosis. As today’s diagnostic facilities are improving and patients are conscious early diagnosis and treatment occurs and chances of getting sclerosed cavity will further reduce).
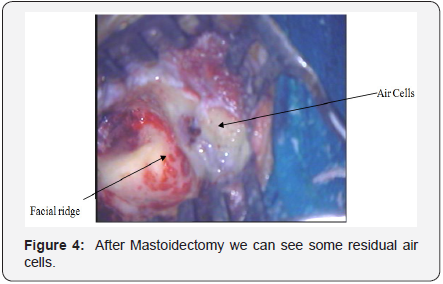
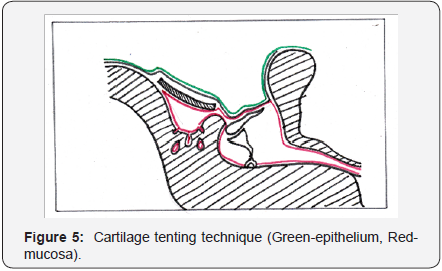
And Second - cellular cavity - in which after complete removal of Cholestaetoma and complete Mastoidectomy, there still remains some cells at the floor (Figure 4). A novel method of closing the cavity - Conchal cartilage which is harvested at the time of meatoplasty is thinned out and laid down posteriorly with convexity upwards or flat so that it creates a small cavity communicating to aditus and then to middle ear and large fascia is lined over it exactly as previous case (Figure 5). If the cartilage is kept touching the floor it will be like cavity filling, not tenting as we want. In both the cases posterior subcutaneous tissue is laid down, canal and TM skin is reflected back and cavity filled with gelfoam and pack for seven days. In some cases attic retraction and thinning of membrane was observed so one small piece of cartilage is also kept at attic to reduce retraction there in further surgeries.
Results
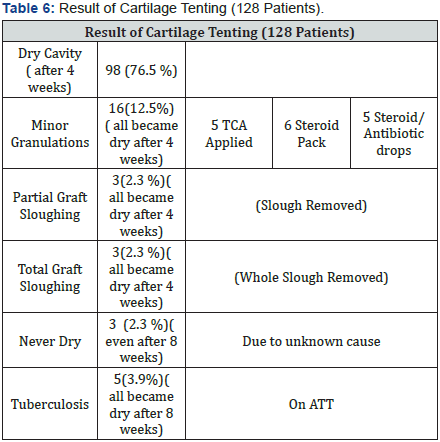
Out of 218 Tympanomastoidectomies, in 72 cases we did not consider air cells in the operated mastoid and all cavities were lined by large fascia directly. This group had 33.33% discharging cavity even after 8 weeks of surgery (Table 5). In another group of 146 we differentiated cellular and sclerotic cavity and reconstructed accordingly. In this group we found cellular cavity in 128 cases and 18were completely sclerosed. Sclerosed cavity mastoids became dries eventless within 4 weeks. Cartilage tenting technique was followed in cellular cavity as discussed before in all 128 cases.

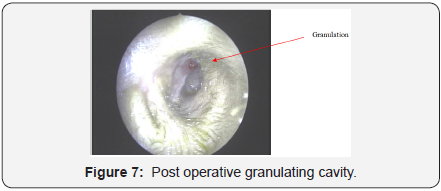
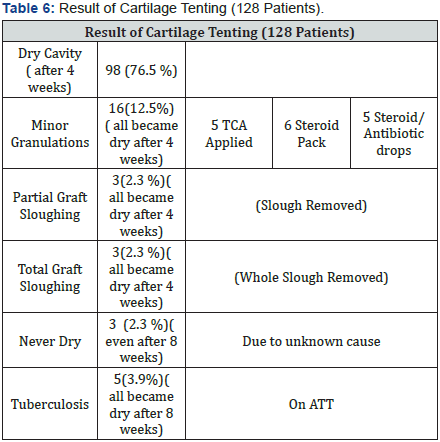
Out of 128 patients we found primary healed cavity in 98, which never had cavity problem.16 cavities were showing granulations (Figures 6 & 7) in follow up and were cured with TCA, steroid pack or steroids drop. 3 mastoid cavities had partial graft sloughing and 3 had total graft sloughing which were removed in post op visit and they healed by secondary intention in 8 weeks time. Biopsy of Mastoid and middle ear granulations was tubercular in 5 patients and they responded well to antitubercular treatment and were dry within 8 weeks. Three patients never became dry even after 8 weeks due to unknown reasons. No revision surgery was required due to cholestaetoma recurrence, meatoplasty problem or for any other reason (Table 6).
Discussion
Earlier we did with end aural approach for all types of cholesteatoma for five years to avoid large incision and scar but we encountered few problems. First being insufficient exposure. Although we get enough exposure but it is definitely less than postaural approach and any limitation in exposure will bring down the results in terms of Cholestaetoma removal or reconstruction, which is not acceptable. Large fascia harvesting is also not possible with this approach, which is indeed needed to cover all the bone, and for primary healing of cavity. It is rare but there is a chance of Keloid formation or a hypertrophied visible scar. So we concluded that endaural approach is not suitable for cholestaetoma surgery and it should be done with post aural incision exactly at post aural crease, which gives no visible scar.
Canal wall up or down procedure
CWU Mastoidectomy means removal of all mastoid air cells while maintaining the integrity of contours in the ear canal. In contrast, CWD Mastoidectomy involves removing the bony posterior canal wall to create a common cavity which combines the ear canal and mastoid [1-3]. Only for rare cases where Cholestaetoma sac is very thick and small and we are sure that by pulling sac the disease comes out in to canal up procedure can be chosen, all other cases will need canal down procedure, because Cholestaetoma removal is by far the most important aim of Cholestaetoma surgery. If we leave Cholestaetoma during surgery for not lowering the canal wall and this becomes the cause of recurrence this is nor forgivable. To conclude canal wall up procedure, and combined approach is not recommended if we are dealing with cholestaetoma. Canal down can be done both inside out and outside in.
The pros and cons of Canal wall up and Canal wall down techniques have long been debated. The root of the controversy remains around whether the bony posterior canal wall should be preserved. In the CWU procedure, the maintenance of original normal contours, such as those of the external auditory canal will help alleviate the disadvantages of creating a cavity in the CWD procedure, which include a lifelong aural servicing, water exposure limits, caloric stimulation vertigo when cold air or water enters the cavity, prolonged recovery, a cosmetically unpleasing appearance, and difficulties in filling hearing aids [4- 7].
Kuo et al. [8] suggested tailor-made tympanomastoidectomy with cartilage reconstruction [8] Mosher first introduced mastoid obliteration using a pedicle musculoperiosteal flap in 1911 to solve problems associated with the postoperative mastoid cavity [9]. Since that time, numerous otologists have reported success with mastoid obliteration techniques, using alloplastic materials as well as various biogenic implants, such as fat, cartilage, bone pate, bone chips, ceramic powder, Ceravital, and hydroxyapatite [10-12].
The prevailing methods of closing the cavity are:
- To leave the mastoid cavity open covering the middle ear with fascia. This allows the mastoid cavity to heal by secondary intention means by granulating and then epithelising. It takes long time to epithelise and till then it will be a discharging and possibly infected cavity or may never epithelise completely.
- The better way is to cover the entire cavity with fascia, post aural flap tissue and maximally saved metal skin.
- Fill the cavity with rotation flap of post aural tissue or Temporalis muscle.
- Fill the cavity with free graft fascia, cartilage pieces, bone pate etc.
Later three methods have their problems if the cells are still left after Mastoidectomy (cavity is cellular).
Cavity reconstruction
What are the options available for reconstruction so that skin and mucosal layers are separated in natural way and their analysis -To get normal anatomical cavities we did -1, canal wall reconstruction by drilling superior and inferior to mastoid cavity and fixing a large cartilage by prolele sutures in few cases, but the problems we encountered were:

- Difficult procedure - as we need really a big piece of cartilage to create posterior canal wall of natural height, but conchal cartilage was at times short of size needed and this led sometimes to Antrocutaneous fistula. Second - with thin dural and sinus plates sometimes it is difficult to drill through and fix cartilage (Figure 8).
- Second method of creating separate cavity is to leave a strip of bone laterally and clear everything downwards lowering the facial ridge to its maximum. This is as good as canal down in terms of exposure but not always possible. A large piece of cartilage which is harvested by meatoplasty is fixed on the bony strip and lined by fascia. Again the size of cartilage needed may always not be sufficient (Figures 9 & 10). These two groups were less in number so their results were not included in this study.


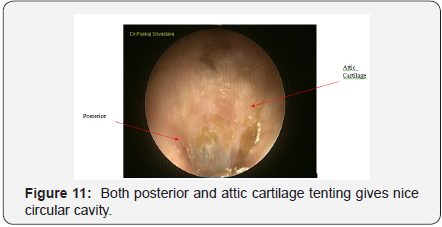
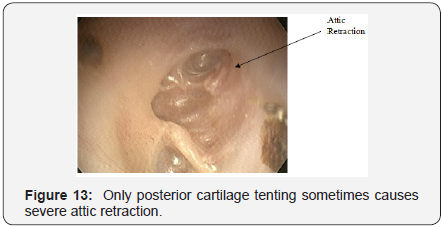
A new and easy method of achieving the goal of separated cavity is followed by us for last 7 yrs. The principle of this is that after Mastoidectomy the left over cells lie on floor of cavity and upper walls are either sclerosed or are thin plate of bone which actually do not have air cells. So if a piece of thin cartilage, large enough to tent these cells is laid in cavity with convexity upwards so that it creates a separate room which communicates with middle ear, and is ultimately lined by fascia? The cartilage piece needed is smaller which is already harvested for meatoplasty, no drilling required, not time consuming, still provides full purpose of maintaining normal physiologically functioning two cavities, primary healing and long term dry cavity. An added advantage being if facial ridge is not lowered ideally it will make no difference in outcome (which many times is the cause of persistent discharging cavity). A small cartilage piece is also kept at Scutum area to give perfect circular cavity (Figure 11) because sometimes there is severe attic retraction (Figures 12 & 13).

Meatoplasty- we do not need a very large meatoplasty as we have already reduced the size of cavity but a large meatoplasty isdone by removing conchal cartilage with extending and removing cartilage of floor of external auditory canal which actually increases the size of meatoplasty without ugly looking large size meatoplasty and it lowers the floor of canal entry which helps in easy drainage and early dry cavity. In Cholestaetoma surgery we close the mastoid cavity by putting fascia; cartilage etc as a free graft which ultimately needs nutrition to be live. So the more free graft we put more need of nutrition is there and so less chances of graft and tissue becoming live. Such grafts and tissues slough and become source of infection and discharging cavity. So we should put thinnest possible fascia and cartilage and minimum possible bone pate, cartilage or other tissue. Foreign body like sialastic sheet etc should be avoided to prevent failures.
Concept of Horizontal and vertical free grafts in mastoid: A large thin fascia kept will not slough as it gets supply from underlying bone (large area) so called horizontal graft, but thick fascia or multiple layer free grafts may slough as it will get supply from a smaller area, so called vertical graft. The various methods and steps followed in this study are selected on their merits and put together so that each patient is benefitted by best set of steps with a new cartilage tenting technique. It is at times impossible to remove / exenterate all the air cells or at least very time consuming and practically not necessary.
A complete, ideal Mastoidectomy, lowered ridge with saucerisation and good meatoplasty is done, because in few cases if posteriorly kept cartilage and fascia may slough out fully or in part, we remove all the slough whenever seen in post op visit and then cavity heals by secondary intention without any need for revision surgery. Concept of secondary infection: In post operative discharging cavity infection is not the primary cause, it is secondary to sloughing of tissues or granulations, mucosa coming over epithelium or epithelium growing inside mucosa or sometimes tuberculosis like chronic infections. We have to remove slough, treat granulation or revise Mastoidectomy. Only Antibiotics, aural toilet, culture sensitivity etc will not work most of the time.
Conclusion
The purpose of this paper is to travel through the shifting methods in performing ear surgery for Cholestaetoma, their problems, failure and learning from them to reach an acceptable procedure, which gives good and consistent result.
References
- Dornhoffer JL, Friedman AB, Gluth MB (2013) Management of acquired cholesteatoma in the paediatric population. Curr Opin Otolaryngol Head Neck Surg 21(5): 440-445.
- Nikolopoulos TP,Gerbesiotis P (2009) Surgical management of cholesteatoma: the two main options and the third way-atticotomy/ limited Mastoidectomy. Int J Pediatr Otorhinolaryngol 73(9): 1222- 1227.
- Syms CA, Syms MJ, SheehyJL (2010) Mastoidectomy-intact canal wall procedure. Otologic Surgery chapter 16, Saunders, Philadelphia, Pa, USA.
- Tomlin J, Chang D, McCutcheon B, Harris J (2013) Surgical technique and recurrence in cholesteatoma: a meta-analysis. Audiol Neurotol 18(3): 135-142.
- Dodson EE, Hashisaki GT, Hobgood TC, Lambert PR (1998) Intact canal wall Mastoidectomy with tympanoplasty for cholesteatoma in children. Laryngoscope 108(7): 977-983.
- Naclerio R, Neely JG, Alford BR (1981) A retrospective analysis of the intact canal wall tympanoplasty with Mastoidectomy. Am J Otol 2(4): 315-317.
- Carlson ML, Latuska RF, Pelosi S, Wanna GB, Bennett ML, et al. (2014) Evolving considerations in the surgical management of cholesteatoma in the only hearing ear. Otol Neurotol 35(1): 84-90.
- Kuo CL, Shiao AS, Liao WH, LienCF (2012) Functional surgery for paediatriccholesteatoma: a 25-year longitudinal study. Cholesteatoma and Ear Surgery-An Update pp. 225-227.
- Harris Peyton Mosher (1911) A method of filling the excavated mastoid with a flap from the back of the auricle. The Laryngoscope 21(12): 1158-1163.
- Kuo CL, Lien CF, Shiao AS (2014) Mastoid obliteration for paediatric suppurative cholesteatoma: long-term safety and sustained effectiveness after 30 years’ experience with cartilage obliteration. Audiol Neurotol 19(6): 358-369.
- Singh V, Atlas M (2007) Obliteration of the persistently discharging mastoid cavity using the middle temporal artery flap. Otolaryngol Head Neck Surg 137(3): 433-438.
- T. Palva (1973) Operative technique in mastoid obliteration. Acta Oto- Laryngologica 75(4): 289-290.





























