Malignant Vascular Tumors of Temporal Bone: Review Article
Omar Ramadan*
Department of ENT, Paterson NJ, USA
Submission: November 22, 2016; Published: December 06, 2016
*Corresponding author: Omar Ramadan, Independent researcher, ENT registrar, Paterson NJ, New Jersey, USA
How to cite this article: Omar R. Malignant Vascular Tumors of Temporal Bone: Review Article. Glob J Otolaryngol. 2016; 2(3): 555589. DOI: 10.19080/GJO.2016.02.555589
Abstract
Objective: The objective of this study was to present a review article about temporal bone vascular tumors.
Data Sources: Published English-language literatures in PubMed and Google scholar.
Review methods: PubMed and Google scholar were systematically searched using search terms: angisarcoma, temporal and bone, hemangioendothelioma, temporal and bone. Kaposi, sarcoma, temporal and bone, hemangiopericytoma, temporal and bone.
Study Selection: We included studies about vascular tumors of temporal bone.
Results: Fortyfive studies were included in this study.The results showed the most patients were male, mass was the common symptom, external ear was the most common site and surgery was the essential treatment.
Conclusion: malignant vascular tumors of temporal bone are rare malignant sarcomas that should be considered in the differential diagnosis of temporal bone mass.
Introduction
Malignant vascular tumors are extremely rare in children and adults. Vascular neoplasms are the most common subcutaneous deep soft tissue sarcoma and in pediatric age. Malignancy is only seen in 2% of blood vessel tumors. They include angiosarcoma, hemangioendothelioma, Kaposi sarcoma and hemangiopericytoma A review by the University of Minnesota revealed only four case of malignant vascular tumor among 228 vascular tumor (3 angiosarcoma and one Kaposi cancer). A review by the Memorial Sloan-Kettering Cancer Center included six patients less than 21 years diagnosed between 1970 and 1995: four were angiosarcomas and two malignant hemangioendotheliomas. Farr et al. [1,2] reported 21 cases of head and neck malignant vascular tumor, ten of them were angiosarcomas and the other eleven cases were hemangiopericytomas .The absolute and net five year cure rate was 25 % and was achieved by radical surgery alone.
Material and Methods
Literature review was conducted using PubMed (MEDLINE) and Google Scholar for English articles. The following keywords were used: angisarcoma, temporal and bone; hemangioendothelioma, temporal and bone; Kaposi, sarcoma, temporal and bone; hemangiopericytoma, temporal and bone.
Inclusion criteria
All malignant vascular tumors of temporal bone published articles were included in the study.
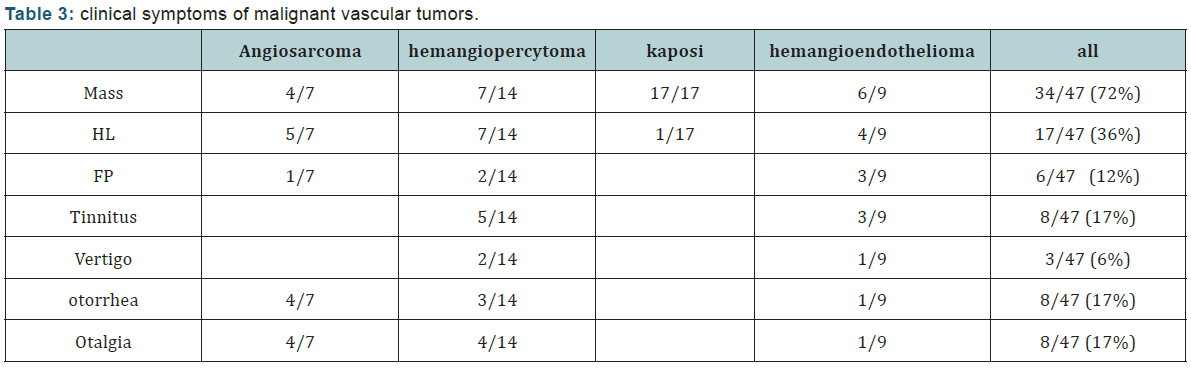
Results: Forty-five studies about malignant vascular tumors of temporal bone were available in PubMed (MEDLINE) and Google scholar in English literature (Tables 1 & 2).
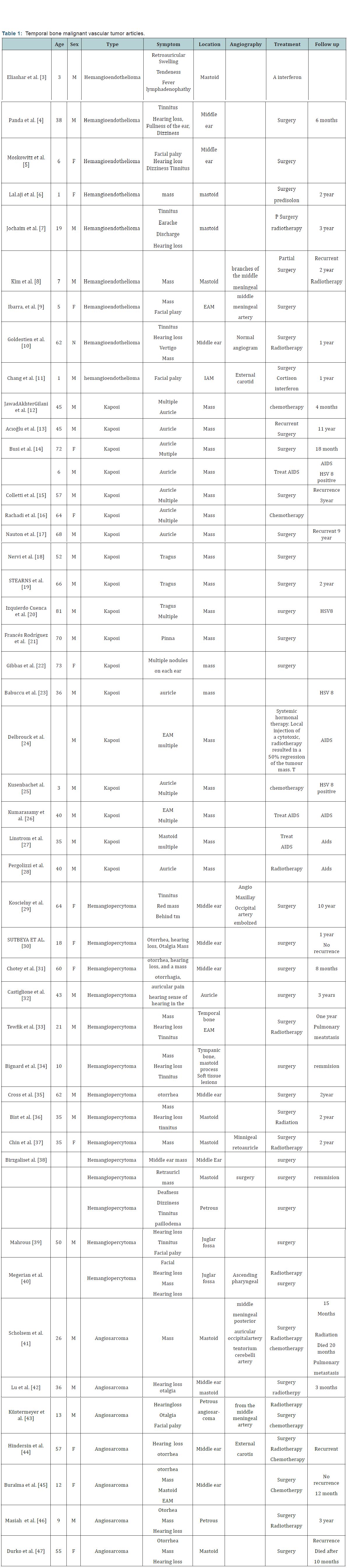
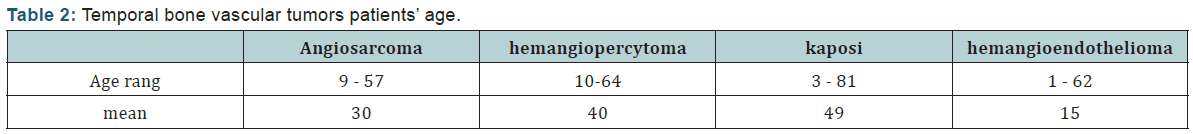
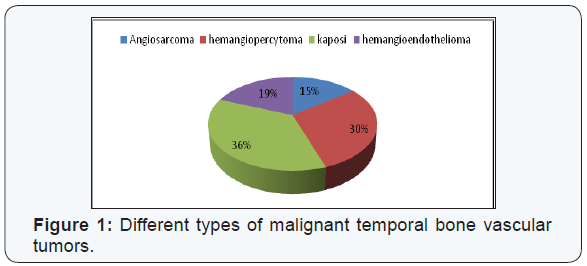
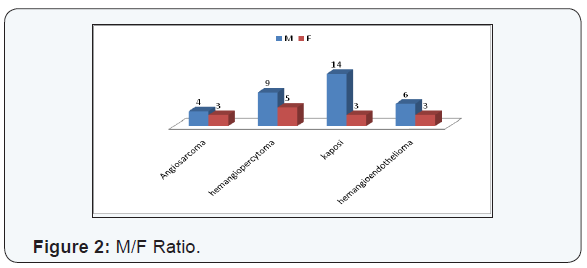
- Demography: There were 47 cases of malignant vascular tumors, 7 cases of angiosarcoma, 14 cases of hemangiopercytoma, 17 cases of kaposi sarcoma and 9 cases of hemangioendothelioma. There were 33 male and 14 female. There were 11 children and 36 adults. Angiosarcoma and hemangiendothelioma are seen more in child and young patients, while hemangiopercytoma and Kaposi sarcoma are seen more in adults (Figures 1-3) (Table 3).
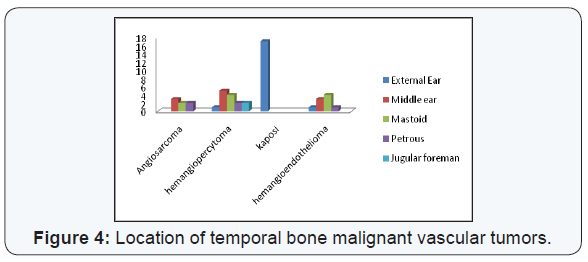
- Location: The most common location was middle ear for angiosarcoma and hemangiopercytoma, external ear for Kaposi sarcoma and mastoid for hemangioendothelioma (Figure 4).
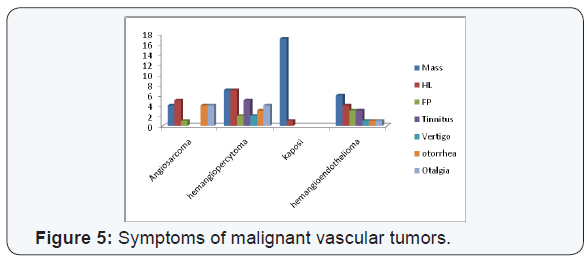
- Clinical symptom: Mass was the most common symptom in all types of malignant vascular tumors, followed by hearing loss and otorrhea (Table 2) (Figure 5).
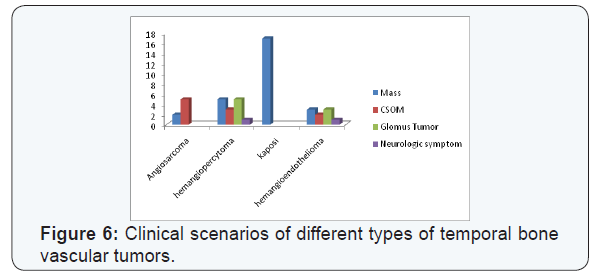
- Clinical course: Kaposi sarcoma of temporal bone usually appear as mass in external ear, hemangioperacytoma appear like a glmous tumor or mass, angiosarcoma appear as CSOM, while there is no specific form for angiosarcoma (Figure 6).
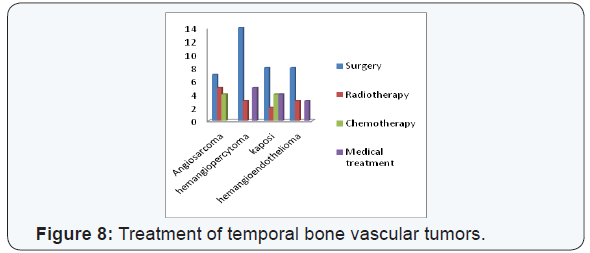
- Treatment: Surgery is the essential treatment for malignant vascular tumors, radiotherapy used for high degree tumors or close margins, chemotherapy used for angisarcoma and multiple lesions of Kaposi sarcoma. Interferon or cortisonmay be used for hemangioendotheloma. AIDS should be treated in positive patients with sarcoma Kaposi (Figures 7 & 8).
- Recurrence: There were 6 cases of recurrence 12% (one case of angiosarcoma, one case of hemangiopercytoma, one case of hemangioendothelioma and 3 cases of Kaposi sarcoma).


Kapos Sarcoma
There were 17 case of Kaposi sarcoma, 10 cases were multiple lesions (58%), 6 cases associated with AIDS (35%) and four cases associated with HSV 8 (23%).
Angiography
Middle meningeal artery was the most common artery giving blood supply to tumors followed by posterior auricle artery (Figure 7).
Discussion
Hemangioendotheliomas are neoplastic proliferations of blood vessel endothelial cells, forming thin-walled blood vessels and sheets of neoplastic cells. These lesions have variable malignant behavior, depending on their microscopic features. Hemangioendotheliomas usually show poor histologic differentiation, nuclear a typia and the existence of mitotic figures. These tumors may be divided into three groups: grade I, grade II, and grade III. The diagnostic grades I through III [3-7] are based on the presence of abundant vascular channels lined by only mildly atypical neoplastic endothelial cells and rare mitoses (in grade I). Grade III lesions show the most anaplastic features.
The radiographic findings of hemangioendothelium usually demonstrate an osteolytic sharply demarcated lesion. Surgical resection is the treatment of choice for hemangioendothelioma, radiation is advised for high grade lesions and non-operable cases. Chemotherapy has no significant role in the treatment.
Some authors reported successful treatment with a interferon in two infants with hemangioendotheliomas [3].
KS is a vascular tumor that originates from vascular and lymphatic endothelium, it is characterized by a multifocal angiogenic process, frequently presenting as multiple vascular cutaneous and mucosal nodules. Nodal and visceral manifestations are usually observed in case of severe immuno suppression. Risk factors for KS development may include e diabetes, advanced age and the use of corticosteroid medication KS is also associated with viral infection such AIDS and HHV8. Typical lesions are reddish-purplish papules, maculae, or nodules. KS mostly occurs in elderly men as multiple bilateral cutaneous lesions of the lower extremities. The involvements of the head and neck area have been observed in only 14% of cases of KS with Only a few cases of ear involvement. A standard therapeutic guideline is not available; the treatment is depending on the subtype and stage of the neoplasm as well as on the immune status of the patient [15].
Haemangiopericytoma is extremely rare vascular tumor that usually seen in the trunk and lower extremities. It acounts1% of all vascular neoplasms, about 15-25% of haemangiopericytomas occur in the head and neck region. The pericytes are the round or spindle shaped contractile cells, proliferations of these cells are responsible for the haemangiopericytoma evolution. McMaster et al. have divided haemangiopericytomas histologically as: benign (low-grade); borderline (intermediate grade); and malignant (high-grade). They expected malignant behavior in cases having a slight degree of cellular anaplasia or one mitotic figure per 10 highpower fields or having a moderate degree of cellular anaplasia and one mitotic figure per 20 high-power fields. The majority of the reported head and neck cases are seen in the nasopharynx, nasal cavity, paranasal sinuses, mandible, maxilla and the orbit. Haemangiopericytoma of the temporal bone is extremely rare with only a few cases were reported in English literatures. Pre-operative embolization may help to obtain a better surgical result. Surgical excision is the treatment of choice. Radiotherapy may be helpful after incomplete resection of the tumor. The role of chemotherapy in the treatment of the haemangiopericytoma is still unclear. The recurrence rate of the tumour is relatively high [31].
Angiosarcoma is a rare malignant sarcoma with endothelial differentiation. They represent only 0.5-1% of malignant primary bone neoplasia. Bone angiosarcom as usually occur in the limbs and less likely in the pelvis, ribs, and vertebra. The skull is an unusual site of angiosarcom with only few cases reported in the literature. Parietal and frontal bones are more commonly involved than the sphenoid, occipitaland temporal bones. Radiation therapy, arsenic exposure and previous trauma have not reported to be predisposing factors for skull angiosarcoma. Cranial angiosarcomas are often unicentric lesions. Most cases of skull angiosarcoma occurred in the third decade with a marked male predominance. Skull angiosarcoma often occur as growing mass or swelling, while the manifestations of temporal bone angiosarcoma are hearing loss, tinnitus, and otalgia with a mass in the temporal area. On CT scan, skull angiosarcoma usually appear as a well-demarcated lytic, hypervascularized and hemorrhagic mass. Angiosarcomas have variable malignant behavior related to their degree of vascular differentiation and microscopic appearance. Immunohistochemistry is necessary in poorly differentiated tumors for the identification of an endothelial lineage. Skull angiosarcomas have a rapid onset of symptoms and high percentage of local recurrence or metastasis. The prognosis of skull angiosarcoma is a poor due secondarily involvement of the meninges and the brain and the impossibility to perform a complete surgical resection. Extensive staging must be conducted in all cases at the time of diagnosis and the follow-up should include regular bone CT scan, cerebral imaging and chest radiography. Preoperative embolization may help to achieve a total excision of the tumor with minimal blood loss. The complete surgical removal of the tumor is the most effective treatment, but adequate margins are often difficult to achieve. Radiotherapy may be given as an adjunct to surgical therapy or as palliative treatment in non-operable cases of skull angiosarcoma. Adjuvant chemotherapy with paclitaxel may help the condition of patients with soft-tissue sarcoma of the face or scalp [41].
Conclusion
Malignant vascular tumors of temporal bone are very rare, mostly seen in adult male except hemangioendothelioma which is seen more in pediatrics, Kaposi sarcoma is the most commonly type of theses tumors, it is usually seen as multiple lesions associated with HIV or HSV * virus.. Mass and hearing loss are the most common symptoms. Middle meningeal artery was the most common artery giving blood supply. Surgery is the essential treatment with adjuvant radiotherapy and chemotherapy for selected cases. There is a local recurrence in 12% of cases (Table 4).

References
- Ferrari A, Casanova M, Bisogno G, Cecchetto G, Meazza C, et al. (2002) Malignant vascular tumors in children and adolescents: a report from the Italian and German Soft Tissue Sarcoma Cooperative Group. Med Pediatr Oncol 39(2): 109-114.
- Farr HW, Carandang CM, Huvos AG (1970) Malignant vascular tumors of the head and neck. Am J Surg 120(4): 501-504.
- Eliashar R, Saah D, Osin P, Sichel JY (1997) Hemangioendothelioma of the temporal bone in a child. Int J Pediatr Otorhinolaryngol 40(1): 67- 71.
- Panda NK, Rao SS, Karuppiah S, Vaiphei K, Singh P (2007) Epithelioid of middle ear masquerading as glomus tumor. American Journal of Otolaryngology 28(1): 69-71.
- Moskowitz HS, Jaffe R, Hirsch BE (2011) Epithelioid hemangioendothelioma of the middle ear in a child. Am J Otolaryngol 32(3): 259-262.
- Lalaji TA, Haller JO, Burgess RJ (2001) A case of head and neck kaposi form hemangioendothelioma simulating a malignancy on imaging. Pediatr Radiol 31(12): 876-878.
- Joachims HZ, Cohen Y (1974) Hemangioendothelioma of the mastoid bone. Laryngoscope 84(3): 454-458.
- Kim HL, Im SA, Lim GY, Chun HJ, Lee H, et al. (2004) High grade hemangioendothelioma of the temporal bone in a child: a case report. Korean J Radiol 5(3): 214-217.
- Ibarra RA, Kesava P, Hallet KK, Bogaev C (2001) Hemangioendothelioma of the temporal bone with radiologic findings resembling hemangioma. AJNR Am J Neuroradiol 22(4): 755-758.
- Goldstein WS, Bowen BC, Balkany T (1994) Malignant hemangioendothelioma of the temporal bone masquerading as glomustympanicum. Ann OtolRhinolLaryngol 103(2): 156-159.
- Chang JM, Kwon BJ, Han MH, Kang HS, Chang KH (2006) Kaposi form hemangioendothelioma arising from the internal auditory canal. AJNR Am J Neuroradiol 27(4): 931-933.
- Gilani JA, Ullah Khan A, Shahid S, Ullah Khan I, Ullah Khan S (2009) Clinical presentation of non-HIV Kaposi Sarcoma. J Coll Physicians Surg Pak 19(9): 586-588.
- http://www.turkarchotolaryngol.net/sayilar/2/buyuk/45-48.pdf
- Busi M, Altieri E, Ciorba A, Aimoni C (2014) Auricular involvement of a multifocal non-AIDS Kaposi’s sarcoma: a case report. Acta Otorhinolaryngol Ital 34(2): 146-149.
- Colletti G, Allevi F, Moneghini L, Rabbiosi D (2013) Bilateral auricular classic Kaposi’s sarcoma. BMJ Case Rep
- Rachadi H, Zemmez Y, Znati K, Ismaili N, Hassam B (2016) External ear nodule revealing a disseminated Kaposi disease. Dermatol Online J 22(8).
- NAUNTON RF, STOLLER FM (1960) Kaposi’s sarcoma of the auricle. Laryngoscope 70: 1535-1540.
- Nervi SJ, Benson B, Gounder S, Jyung R (2006) Pathology quiz case 2. Kaposi sarcoma (KS) of the pinna and external auditory canal. Arch Otolaryngol Head Neck Surg 132(5): 555-555.
- Stearns MP, Hibbard AA, Patterson HC (1983) Kaposi’s Sarcoma of the ear: a case study. J Laryngol Otol 97(7): 641-645.
- Marta Izquierdo Cuenca, Magdalena Pérez Ortín, José M. Gómez Martín- Zarco (2013) Kaposi sarcoma in the external ear. Acta Otorrinolaringol Esp 64(6): 448.
- Gibbs RC (1968) Kaposi’s sarcoma involving the ears. Arch Dermatol 98: 104-105.
- Babuccu O, Kargi E, Hoşnuter M, Doğan BG (2003) Atypical presentation of Kaposi’s sarcoma in the external ear. Kulak Burun Bogaz Ihtis Derg 11: 17-20.
- Delbrouck C, Kampouridis S, Chantrain G (1998) An unusual localisation of Kaposi’s sarcoma: the external auditory canal. Acta Otorhinolaryngol Belg 52(1): 29-36.
- Kusenbach G, Rübben A, Schneider EM, Barker M, Büssing A, et al. (1997) Herpes virus (KSHV) associated Kaposi sarcoma in a 3-year-old child with non-HIV-induced immunodeficiency. Eur J Pediatr 156(6): 440-443.
- Kumarasamy N, Venkatesh KK, Devaleenol B, Poongulali S, Ahilasamy N (2008) Regression of Kaposi’s sarcoma lesions following highly active antiretroviral therapy in an HIV-infected patient. Int J STD AIDS 19(11): 786-788.
- Christopher J Linstrom, Robert L Pincus, Eric B Leavitt, Mariana C Urbina (1993) Otologicneurotologic manifestations of HIV-related disease. Otolaryngol Head Neck Surg 108(6): 680-687.
- Pergolizzi S, Delia P, Grazioso Russi E, Raffaele L, Settineri N, et al. (1995) Radiotherapy of an unusual case of Kaposi’s sarcoma of the “classic” type located in the external ear. Radiol Med 89(6): 910-913.
- Koscielny S, Bräuer B, Förster G (2003) Hemangiopericytoma: a rare head and neck tumor. Eur Arch Otorhinolaryngol 260(8): 450-453.
- Sutbeyaz Y, Selimoglu E, Karasen M, Ciftcioglu A, Ozturk A (1995) Haemangiopericytoma of the middle ear: case report and literature review. J Laryngol Otol 109(10): 977-979.
- Chotey NA, Naidu TK, Naidoo V, Naidoo J (2013) Myopericytoma of the external auditory canal and tragus. J Laryngol Otol 127: 805-808.
- Castiglione M, Nardo L, Ottaviani F (2016) Hemangiopericytoma arising from the cartilage of the external auditory canal. Head Neck 38(5): E108-110.
- Tewfik TL, Finlayson M, Attia EL (1981) Hemangiopericytoma of the temporal bone. J Otolaryngol 10(1): 72-77.
- Bignardi L, Fabbiano A, Franceschetti E (1985) Hemangiopericytoma of the external auditory canal in childhood: description of a case. Acta Otorhinolaryngol Ital 5(6): 643-649.
- Cross DL, Mixon C (1996) Temporal bone hemangiopericytoma. Otolaryngol Head Neck Surg 114(4): 631.
- Bist SS, Varshney S, Kumar R, Gupta N (2010) Hemangiopericytoma presenting as an external auditory canal mass. Ear Nose Throat J 89: 208-212.
- Chin LS, Rabb CH, Hinton DR, Apuzzo ML (1993) Hemangiopericytoma of the temporal bone presenting as a retroauricular mass. Neurosurgery 33(4): 728-732.
- Birzgalis AR, Ramsden RT, Lye RH, Richardson PL (1990) Haemangiopericytoma of the temporal bone. J Laryngol Otol 104(12): 998-1003.
- Mahrous (2006) Haemangiopericytoma mimicking Glomus Jugulare tumour. The Internet Journal of Head and Neck Surgery 1(1).
- Megerian CA, McKenna MJ, Nadol JB (1995) Non-paraganglioma jugular foramen lesions masquerading as glomus jugulare tumors. Am J Otol 16(1): 94-98.
- Scholsem M, Raket D, Flandroy P, Sciot R, Deprez M (2005) Primary temporal bone angiosarcoma: a case report. J Neuro oncol 75(2): 121- 125.
- Lu Y, Zhang M (2012) Pemphigus herpetiformis in a patient with welldifferentiated cutaneous angiosarcoma: case report and review of the published work. J Dermatol 39(1): 89-91.
- Julian Küstermeyer, Helmut Ostertag, Jörg Hattingen, Hans-Jürgen Welkoborsky (2015) Tumor of the Temporal Bone Mimicking Acute Mastoiditis. Ann Otolaryngol Rhinol 2(5): 1039.
- Angiosarkom Des Os Temporale S Hindersin, et al. (2008) Laryngorhinootologie 87(5): 345-348.
- Buraïma F, Kouassi YM, Coulibaly A, Touré A, Tanon-anoh MJ, et al. (2011) A case of middle-ear angiosarcoma. Eur Ann Otorhinolaryngol Head Neck Dis 128(2): 87-89.
- Masieh M (1980) Haemangiosarcoma of the petrous temporal bone. J Laryngol Otol 94(2): 205-210.
- Durko T, Papierz W, Pajor A (2003) Angiosarcoma of the temporal bone. Otolaryngol Pol 57(3): 427-433.





























