Factors that Delay Definitive Management of Chronic Rhinosinusitis in India: A survey based study
Jagdish Chaturvedi1*, Sunil N Dutt2, Pooja Kadambi3 and Roma Vishwanath4
1Rhinology Fellow, Otolaryngology, Apollo Hospital, India
2Clinical Director, Senior Consultant, Professor of ENT, Apollo hospitals, India
3Biomedical researcher, India
45Researcher, India
Submission: November 03, 2016; Published: November 10, 2016
*Corresponding author: Jagdish Chaturvedi, Department of Otorhinolaryngology, Apollo Hospital, Bannerghatta road, Bangalore- 560 076, India, Tel:91-9650928582; Email:dr.jagdishc@ymail.com
How to cite this article: Jagdish C, Sunil N D, Pooja K, Roma V. Factors that Delay Definitive Management of Chronic Rhinosinusitis in India: A survey based study. Glob J Otolaryngol. 2016; 2(3): 555586. DOI: 10.19080/GJO.2016.02.555586
Abstract
Background: In India, 134 million people suffer from Chronic Rhinosinusitis (CRS), an expensive and debilitating disorder. Despite Endoscopic Sinus Surgery (ESS) being an important intervention during the management of CRS, the criteria for taking a decision on when to offer surgery is poorly defined. The ambiguousness in Maximal Medical Therapy (MMT) criteria along with the lack of indication for failure of MMT represents an important gap in current healthcare delivery for CRS. This lack of clear indications for ESS is likely to contribute to surgical variation and creates the potential for inappropriate care.
Methods: In order to gather information from a diverse group of Ear Nose Throat (ENT) specialists from different parts of the country, a strategy to collect information at a national level ENT conference was adopted. At Gurgaon, Haryana, ENT specialists were selected at random and those who had more than 5 years of clinical experience and see an average of 15 or more CRS cases per month were selected for a detailed interview.
Results: 81 ENT specialists were interviewed who on an average see 158 cases of CRS per month. Approximately 45% of patients who are counseled for definitive surgical management in the form of ESS, do not undergo surgery immediately and delay it for varying durations of time. According to the ENT doctors that were interviewed, the reasons for patients to defer or refuse surgery are often multi factorial, majorly being cost of surgery and fear of going into surgery under General Anaesthesia (GA).
Conclusion: There is a need for a minimally invasive solution for CRS that can be provided soon after MMT fails, in the outpatient setting at affordable prices. Having alternatives like these that are more economically viable and less invasive would significantly alleviate the concerns of many patients.
Keywords: Balloon Sinuplasty, Chronic Rhinosinusitis, Affordability, Functional Endoscopic Sinus Surgery, minimally invasive surgery, Delayed management
Abbreviations: CRS: Chronic Rhinosinusitis; ESS: Endoscopic Sinus Surgery; FESS: Functional Endoscopic Sinus Surgery; MMT: Maximal Medical Therapy; GA: General Anaesthesia; QoL: Quality of Life
Introduction
Chronic rhinosinusitis (CRS) is a commonly occurring, debilitating, and expensive chronic inflammatory disease [1-3]. An estimated 134 million Indians suffer from CRS, as per the National Institute of Allergy and Infectious Diseases [4]. Despite appropriate medical therapy, a subset of patients with CRS continue to be symptomatic and eventually undergo endoscopic sinus surgery (ESS). Post recommendation of surgery, it often occurs only after many months or even years. Early surgical intervention after diagnosis of CRS, with or without asthma or polyps, is associated with reduced health care utilization compared to delayed intervention after many years of medical management [5].
In the appropriately selected patient with CRS, ESS is associated with improvements in patient symptoms, quality of life (QoL), and proves more economical in the long run than continued medical therapy alone [6-9]. Despite ESS being an important intervention during the management of CRS, the decision on when to consider surgery over medical management is poorly defined. Specifically, there is no consensus on what ‘appropriate’ or maximal medical therapy (MMT) should be provided to patients prior to considering ESS [10]. A minority of ESS studies explicitly reports MMT criteria before considering a patient with CRS as a candidate for ESS. The presence of large variation in MMT criteria along with the lack of what constitutes a “failure” of MMT represents an important gap in the current clinical management of CRS [11].
This lack of clear indications for ESS likely contributes to surgical protocol variations and can lead to inappropriate or inefficient care [12-14]. Further, the authors believe, as practicing ENT specialists that there may be some additional factors such as cost of surgery, hospital stay, fear of surgery and complications etc. that also play a role in this delay of definitive management. There is no data, specific to the Indian population available on the delay from time of failed MMT until definitive management in the form of ESS is received. There is also no data on the possible reasons for the same. To understand this scenario better, the authors carried out structured interviews with 81 E.N.T specialists from different parts of the country. The specialists were asked about the burden of CRS, statistics on patients who receive delayed surgical intervention; the average delay in receiving surgical management and the various factors that contribute to such a delay based on their clinical practice and experience. The authors believe that this information will help in recognizing the level of morbidity that these patients face while they transition from medical management to surgical care and will encourage ENT specialists to offer appropriate definitive management sooner once defined MMT fails.
Material and Methods
This study is a cross-sectional descriptive study led by the first author of this article who is an Ear Nose Throat surgeon based out of Bangalore, India. In order to gather information from a diverse group of ENT specialists from different parts of the country, a strategy to collect information at a national level ENT conference was adopted. A team of two researchers were appointed by the authors for data collection and the author enrolled at a 4 day national level ENT conference held in Gurgaon, Haryana in January 2016. ENT specialists were selected at random and a preliminary one-minute screening interview was carried out which included basic demographic questions (Name, city/region of practice and years of experience) and an estimate of the average number of CRS patients seen per month. Those ENT specialists who had more than 5 years of clinical experience and see an average of 15 or more CRS cases per month were selected for a detailed interview.
The detailed interview included questions pertaining to the typical duration from onset of CRS to time of surgical intervention and the reasons for such delays as per the doctor’s understanding.
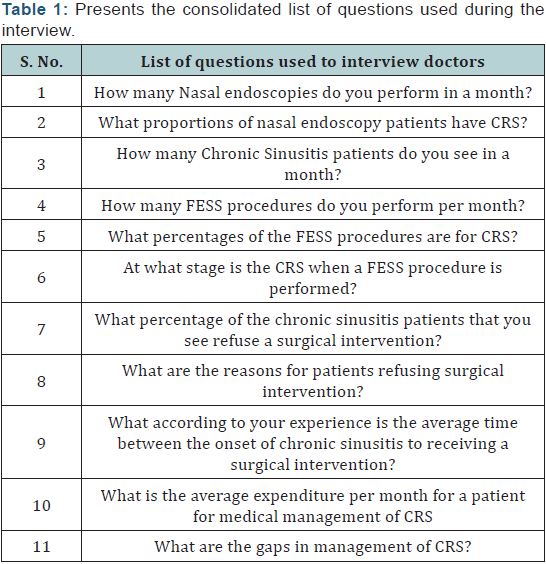
Other questions included number of FESS surgeries performed per month, percentage of patients who undergo FESS surgery, and for those who do not undergo FESS surgery when indicated - what were the typical reasons etc (Table 1) in the Tables and Figures section presents the consolidated list of questions used during the interview. By the end of 4 days 200 ENT specialists underwent the preliminary interview and 81 out of these 200 qualified for a detailed interview. The results were tabulated and recorded. No statistical analysis was indicated for this data as only descriptive statistics were being compiled.
Results
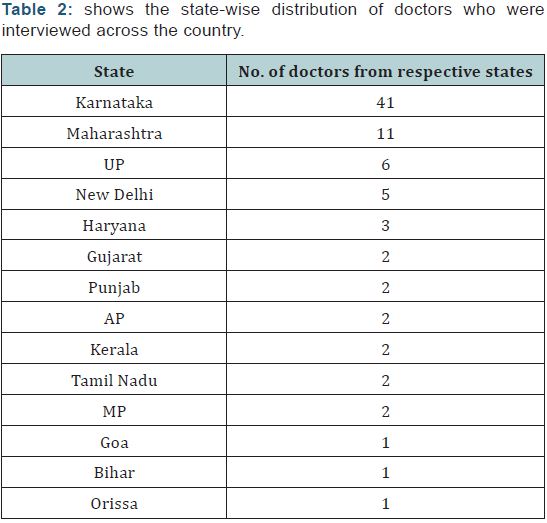
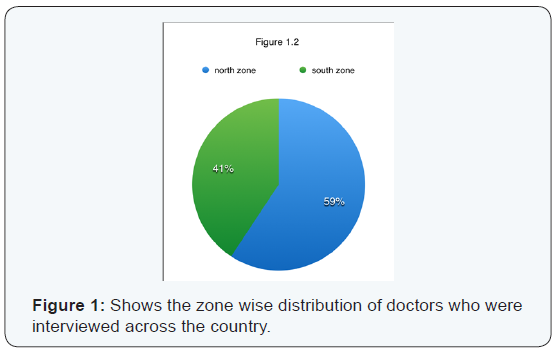
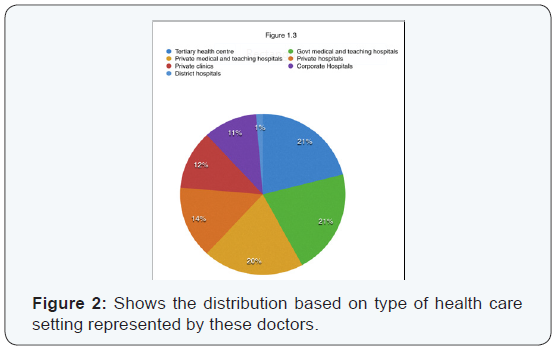
A total of 81 ENT specialists, 12 women and 69 men, with an average 14.62 years of experience underwent the detailed interview. The ENT specialists represented 14 states out of the 29 states in the country and represented many of the health care settings that prevail in India. Table 2 in the Tables and Figures section shows the state-wise distribution of doctors across the country. Figure 1 shows the zone wise distribution of doctors across the country. Figure 2 in the Tables and Figures section shows the distribution based on type of health care setting represented by these doctors.
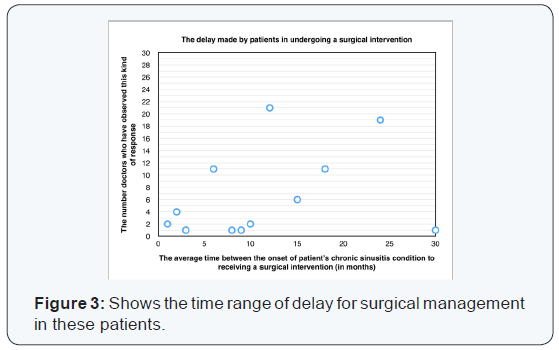
These 81 ENT specialists on an average reported seeing 158 cases of CRS per month. They perform an average of 16 ESS procedures per month. 55% (9) of these surgeries are carried out for patients diagnosed with CRS. The survey showed that 45% of patients who are counseled for definitive surgical management in the form of ESS, do not undergo surgery immediately and delay it for varying durations of time. It is estimated based on the responses gathered that the average delay from the time MMT fails till the patient undergoes definitive surgical management is 14 months (Range of 2 to 36 months).
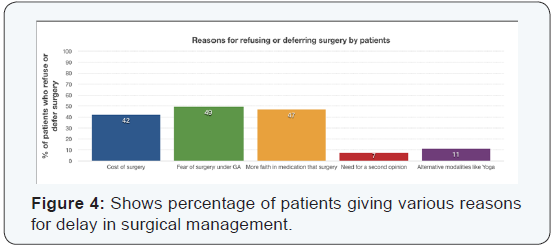
Figure 3 in the Tables and Figures section shows the time range of delay for surgical management in these patients. According to the ENT specialists interviewed, the reasons for surgical delay are often multi factorial. Upon analysis of the responses from the interview, 5 dominant refusal/delay reasons emerged. Roughly 50% of the doctors felt the biggest reason for delay was the fear of undergoing a surgical procedure under General Anaesthesia while around 47% of doctors believed the reason was patients feel they will recover with medications and do not want to undergo an invasive procedure such as an ESS. 42% felt that cost was one of the main reasons whereas 7% and 12% of the ENT specialists felt need for second opinion or trying out alternative forms of healing such as Yoga and Ayurveda were reasons patients delayed definitive management. Figure 4 in the Tables and Figures section shows the percentage of people giving various reasons for delay in surgical management. In addition to staying morbid during these 14 months, the doctors surveyed estimated that patients spend an average 1500 INR per month on medical management. This mounts up to around 22,000 INR over 14 months.
Discussion
Studies have shown that patients who undergo surgery primarily have two types of fear; one of bodily harm and the other of death [15]. Fear of surgery is a well-known factor that contributes to delay in undergoing surgery and prolonged morbidity with chronic diseases. Breisen et al. [16] in an article which aims to understand why patients with cataract refuse free surgery in Kenya reveals that people who refused surgery often reported to know someone whose condition worsened or even became blind after surgery. On being re-interviewed, several people admitted that they had actually never met someone who had unsuccessful surgery but only heard rumors. It was concluded that in Africa, a rumor of blinding eye surgery was commonly used by patients to justify their refusal to have cataract surgery where underlying reasons appeared to be related to shame, fear of surgery or missing social support [16].
Similarly, Karlson et al. [17] in an article on gender differences in patient preferences contributing to differential utilization of elective surgery demonstrated that women were more fearful of undergoing hip or knee surgery for chronic osteoarthritis. Women preferred to suffer arthritis pain rather than risk surgery to avoid disrupting care giving roles for dependent spouses and others during the long recovery time. In India, typically a self-pay system is prevalent where factors like cost and hospitalization time also play a role. The results that emerge from this study show that previously studied factors contribute to surgical delay and/or refusal. In the specific case of CRS and ESS, it has already been well established that due to lack of clear guidelines on Maximal Medical Therapy (MMT), patients are often put on medical management for many months and sometimes years, despite limited improvement [11].
In addition to all the studied contributors to surgical delays, the ENT specialists who were interviewed in this study believe that other factors such as fear of undergoing a procedure under general anaesthesia (GA), feeling that there is no immediate need for surgery, need for exploring alternate medications, cost and need for second expert opinions are also key reasons for delaying FESS. A recent prospective study carried out by Ocampo et al. [18] compared medical management with surgical management of CRS showed that patients who underwent ESS early had greater improvements in quality of life, reduced exposure to antibiotics, and fewer missed days from work compared to those who delayed ESS. In developed reimbursed markets (like UK and USA), minimally invasive solutions such as balloon sinuplasty or osmotic Ostia dilation for management of CRS have addressed these concerns to a large extent.
Patients who want to defer surgery can opt for a minimally invasive, in-office procedure to gain relief from their symptoms. Describing the first year experience of using balloon sinuplasty, Hopkins et al, concludes that sinuplasty offers an acceptable and minimally invasive option for patients who refuse ESS as they are unable to accept the associated risks of ESS [19]. Studies on balloon sinuplasty carried out in India, such as the publication by Raghunandhan et al. [20] highlight the key advantages of this interventional technique over the conventional ESS, is mucosal preservation while bypassing the osteomeatal complex, to access the occluded natural Ostia of the paranasal sinuses. This minimally invasive nature of the technology addresses the fear of invasive surgery in patients. A follow up study carried out by Raghunandhan et al. [20] in 2013 concluded that the balloon sinuplasty shown to be an efficient, minimally invasive tool in the armamentarium of the endoscopic rhinologist. This solution has eliminated the need for postoperative debridement and decreased the frequency of follow-up endoscopies.
In spite of the advantages of in-office balloon sinuplasty, the high cost of balloon sinuplasty devices in India, the procedure has primarily been performed under GA in the operating theatre for those who have insurance coverage primarily as a hybrid (ESS + balloon sinuplasty) procedure. The true benefit of this minimally invasive solution has not yet been achieved due to the limitations created by an expensive and completely disposable device and the requirement of a skilled assistant. If such a procedure were to be performed under local anaesthesia in the outpatient setting, immediate intervention can be provided to the patient at affordable prices without the need for hospitalisation and GA.
Conclusion
Based on the results of this study 45% of patients with CRS remain untreated and delay definitive management for an average 14 months, spending around INR 22,000 on medical management during this time. Typically, morbidity increases and often a more invasive surgery are required eventually. Thus, patients are suffering with a poor quality of life, increasing their risk of complications and being financially burdened by this delay. Fear of undergoing a surgical procedure under General Anaesthesia, feeling they will recover with medications and do not feel they require to undergo an invasive procedure such as an ESS, Cost, need for second opinion and trying out alternative forms of healing such as Yoga and Ayurveda are reasons for delaying definitive management.
There is a need for a minimally invasive solution for CRS that can be provided soon after MMT fails, in the outpatient setting at affordable prices. If such an alternative were to be priced lower than an invasive surgery with hospitalization and/or long term medical management, it would be a more economically viable solution for patients as well. Having such an option would significantly alleviate the concerns of many patients and provide them with immediate relief and improved quality of life.
Acknowledgment
We would like to thank the organizers of the 68th AOICON held at Gurgaon and Karnataka State Conference held at NIMHANS, Bengaluru and all the doctors who took the interest and time to participate in the interview.
References
- Halawi AM, Smith SS, Chandra RK (2013) Chronic rhinosinusitis: epidemiology and cost. Allergy Asthma Proc 34(4): 328-334.
- Rudmik L, Smith TL, Schlosser RJ, Hwang PH, Mace JC, et al. (2014) Productivity costs in patients with refractory chronic rhinosinusitis. Laryngoscope 124(9): 2007-2012.
- Smith KA, Orlandi RR, Rudmik L (2015) Cost of adult chronic rhinosinusitis: a systematic review. Laryngoscope 125(7): 1547-1556.
- Pratibha Masand (2012) 1 in 8 Indians hit by Chronic Rhinosinusitis: A study.
- Benninger MS, Sindwani R, Holy CE, Hopkins C (2015) Early versus delayed endoscopic sinus surgery in patients with chronic rhinosinusitis: impact on health care utilization. Otolaryngol Head Neck Surg 152(3): 546-552.
- Soler ZM, Smith TL (2010) Quality of life outcomes afterfunctional endoscopic sinus surgery. Otolaryngol Clin North Am 43(3): 605-612.
- Smith TL, Kern R, Palmer JN, Schlosser R, Chandra RK, et al (2013) Medical therapy vs surgery for chronic rhinosinusitis: a prospective, multi-institutional study with 1-year follow-up. Int Forum Allergy Rhinol 3(1): 4-9.
- Smith KA, Smith TL, Mace JC, Rudmik L (2014) Endoscopic sinus surgery compared to continued medical therapy for patients with refractory chronic rhinosinusitis. Int Forum Allergy Rhinol 4(10): 823-827.
- Rudmik L, Soler ZM, Mace JC, Schlosser RJ, Smith TL (2014) Economic evaluation of endoscopic sinus surgery versus continued medical therapy for refractory chronic rhinosinusitis. Laryngoscope 125(1): 25-32.
- Lund VJ (2005) Maximal medical therapy for chronic rhinosinusitis. Otolaryngol Clin North Am 38(6): 1301-1310.
- Dautremont JF, Rudmik L (2015) When are we operating for chronic rhinosinusitis? A systematic review of maximal medical therapy protocols prior to endoscopic sinus surgery. Int Forum Allergy Rhinol 5(12): 1095-1103.
- Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, et al. (2014) Understanding of regional variation in the use of surgery. Lancet 382(9898): 1121-1129.
- Venkatraman G, Likosky DS, Morrison D, Zhou W, Finlayson SR, et al. (2011) Small area variation in endoscopic sinus surgery rates among the Medicare population. Arch Otolaryngol Head Neck Surg 137(3): 253-257.
- Rudmik L, Holy CE, Smith TL (2015) Geographic variation of endoscopic sinus surgery in the United States. Laryngoscope 125(8): 1772-1778.
- Surman OS. Fear of Surgery
- Briesen S, Geneau R, Roberts H, Opiyo J, Courtright P (2010) Understanding why patients with cataract refuse free surgery: the influence of rumours in Kenya. Trop Med Int Health 15(5): 534-539.
- Karlson EW, Daltroy LH, Liang MH, Eaton HE, Katz JN (1997) Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med 102(6): 524-530.
- Ocampo CJ, Grammer LC (2013) Chronic rhinosinusitis. J Allergy Clin Immunol Pract 1(3): 205-211.
- Hopkins C, Noon E, Bray D, Roberts D (2011) Balloon sinuplasty: our first year. J Laryngol Otol 125(1): 43-52.
- Raghunandhan S, Prashanth S, Natarajan K, Kumar RA, Kameswaran M (2009) Balloon sinuplasty- the first Indian experience. Indian J Otolaryngol Head Neck Surg 61(2): 99-104.
- Raghunandhan S, Bansal T, Natarajan K, Kameswaran M (2013) Efficacy & outcomes of balloon sinuplasty in chronic rhinosinusitis: a prospective study. Indian J Otolaryngol Head Neck Surg 65(2): 314- 319.





























